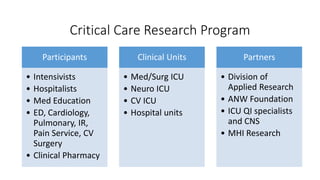
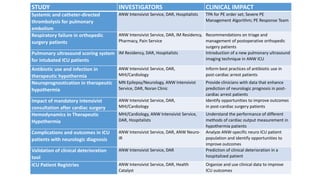
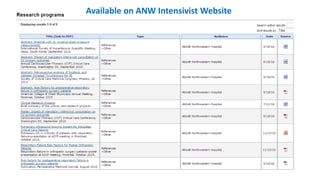
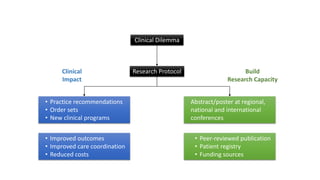
1) The document discusses a critical care research program at Abbott Northwestern Hospital with the goals of conducting studies to improve patient outcomes, enhance quality of care, and reduce costs.
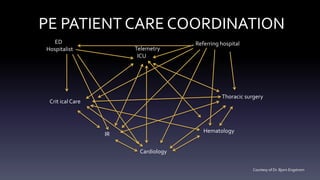
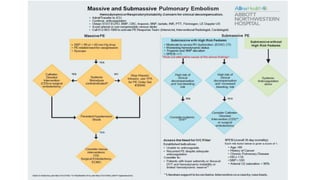
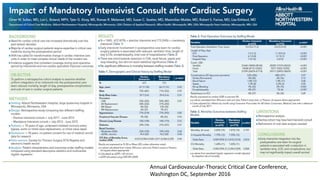
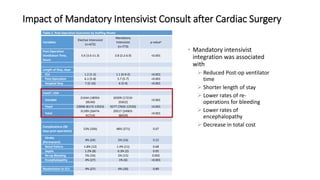
2) The program involves intensivists, hospitalists, and other clinical specialties conducting studies and presenting findings to improve practice.
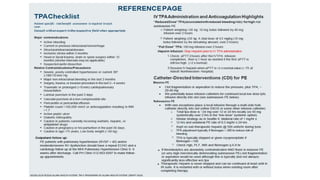
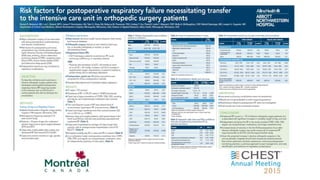
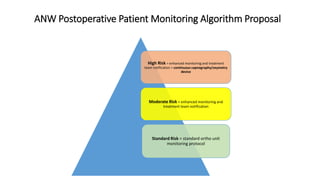
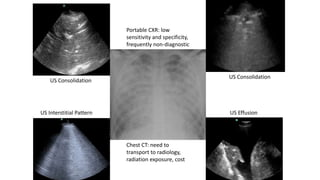
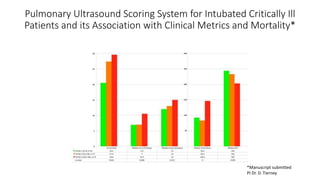
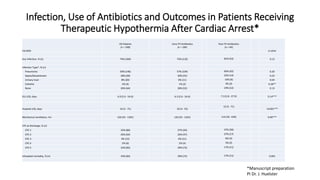
3) Several ongoing studies are summarized that examine issues like postoperative monitoring, pulmonary ultrasound scoring, infection risks, and outcomes after procedures.