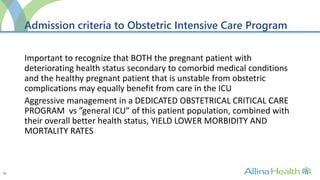
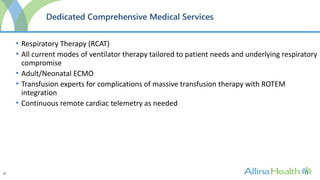
This document outlines plans for an Obstetrical Intensive Care Program with the goals of:
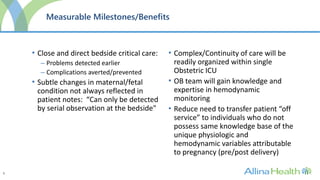
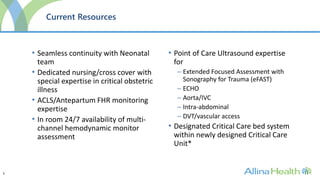
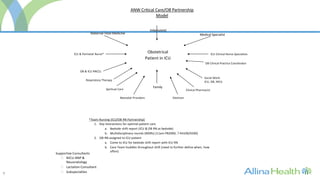
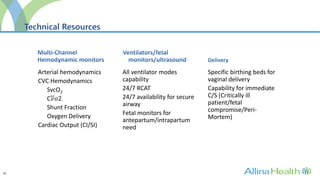
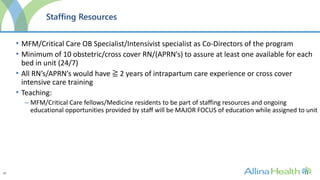
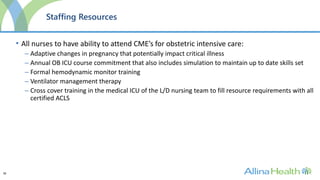
1) Providing comprehensive critical care expertise for obstetric patients through a dedicated program.
2) Serving as a model for critical care of obstetric patients in the Midwest region.
3) Ensuring optimal outcomes for mothers, fetuses, and newborns through collaboration between obstetric, neonatal, and critical care teams.
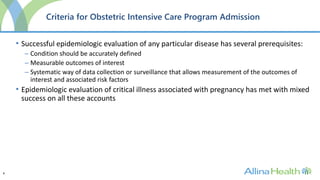
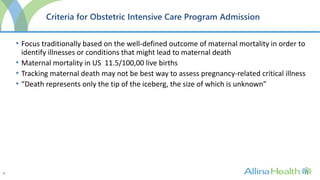
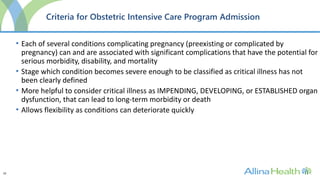
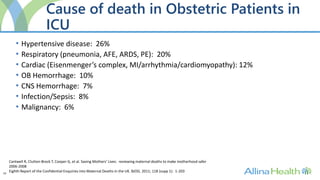
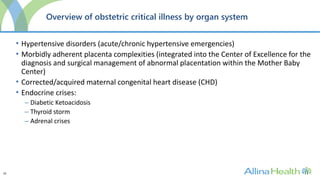
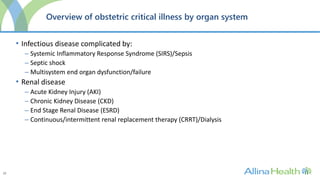
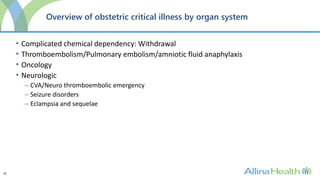
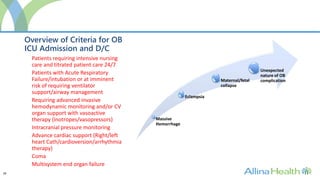
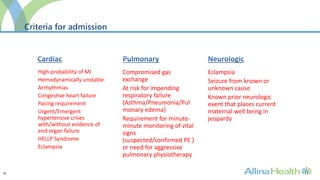
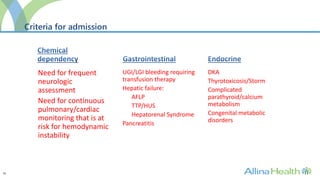
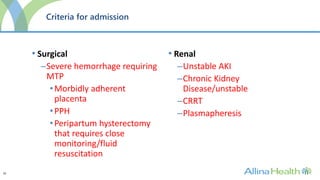
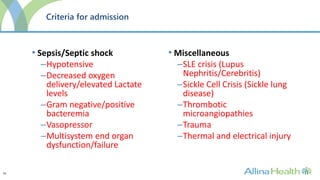
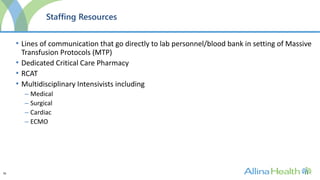
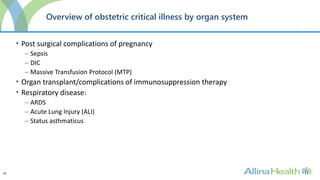
The program would admit patients requiring intensive monitoring and treatment for conditions such as preeclampsia, postpartum hemorrhage, heart disease, infections, and multi-organ dysfunction. It aims to improve outcomes over traditional ICUs through staff trained in obstetric critical