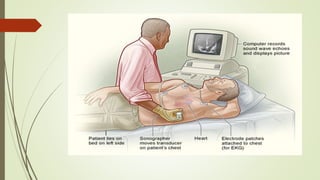
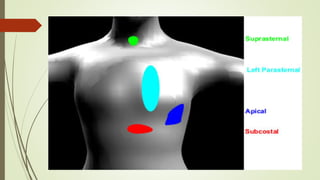
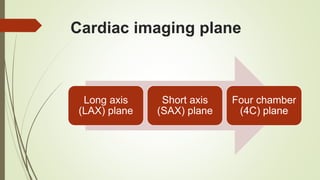
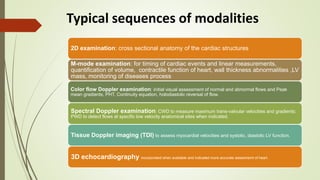
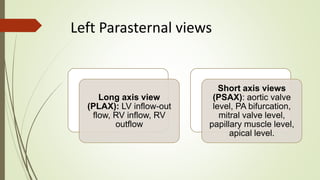
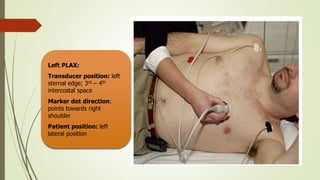
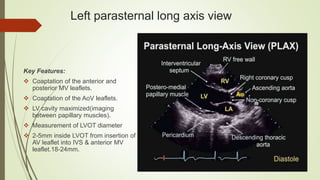
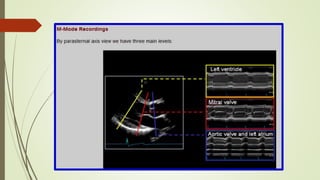
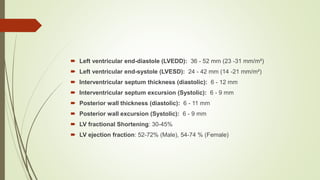
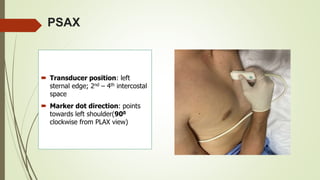
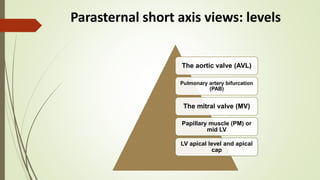
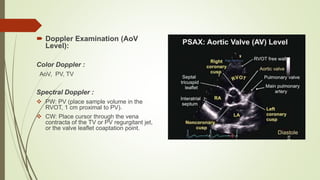
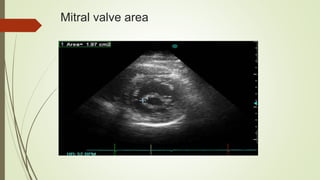
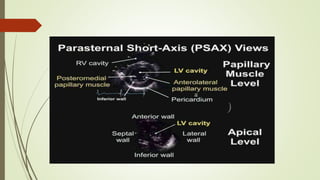
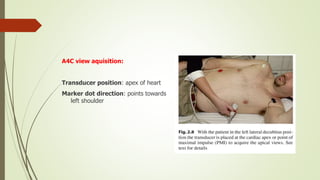
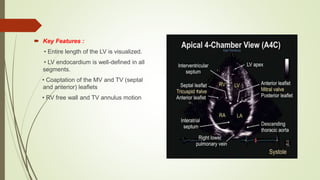
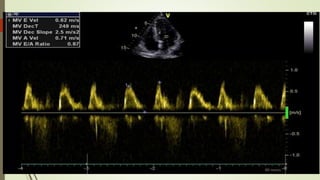
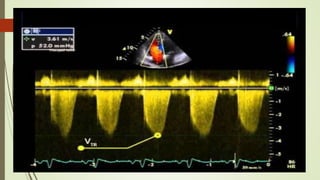
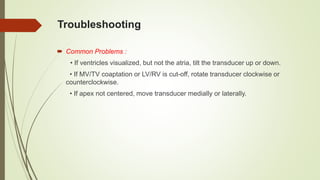
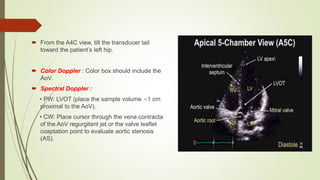
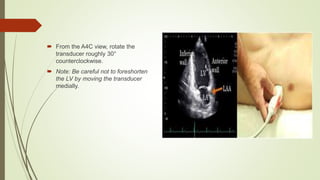
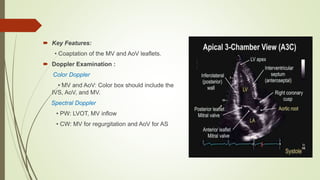
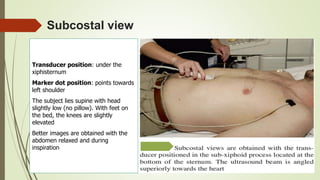
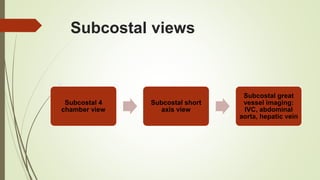
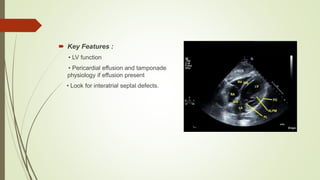
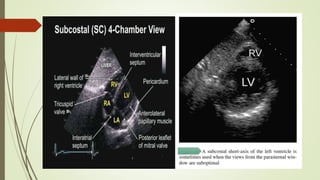
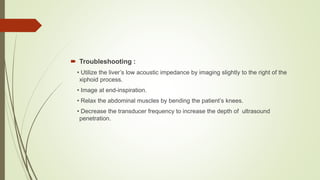
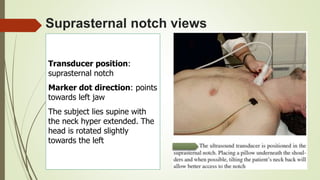
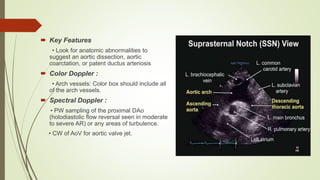
This document provides an overview of echocardiogram views and measurements. It describes the standard views obtained from the parasternal, apical, subcostal, and suprasternal windows. For each view, it indicates the transducer position, imaging plane, and cardiac structures visualized. It also provides typical Doppler sequences and includes normal measurements for cardiac structures. Troubleshooting tips are provided for technically difficult studies.