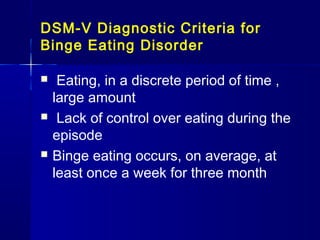
This document provides an overview of eating disorders including anorexia nervosa, bulimia nervosa, binge eating disorder, and obesity. It describes the general characteristics and diagnostic criteria for each disorder according to the DSM-V. For anorexia nervosa and bulimia nervosa, it outlines their epidemiology, biological and psychological etiologies, clinical features, treatment approaches, and prognosis. It also discusses the Eating Disorder Inventory assessment and compares some key aspects of anorexia nervosa and bulimia nervosa.