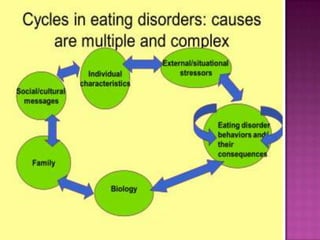
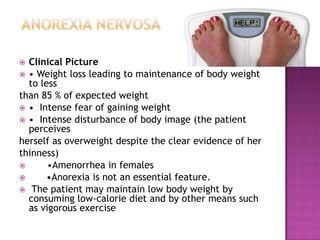
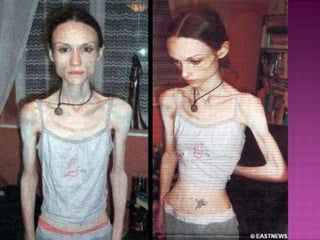
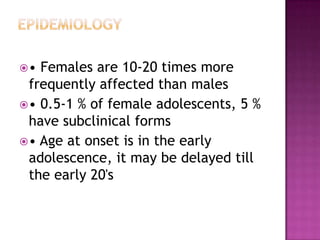
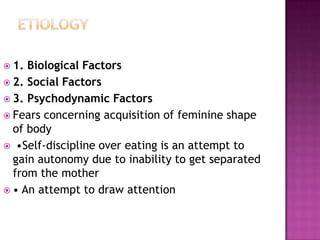
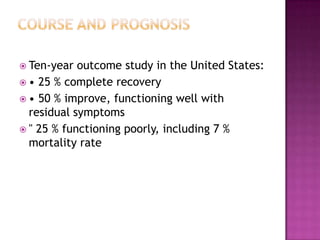
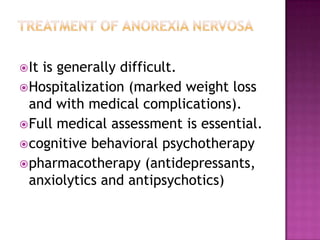
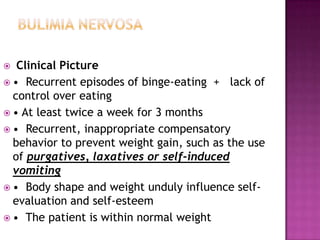
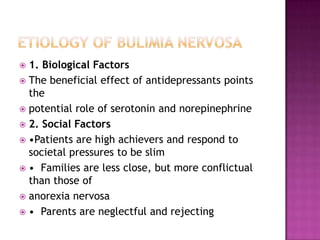
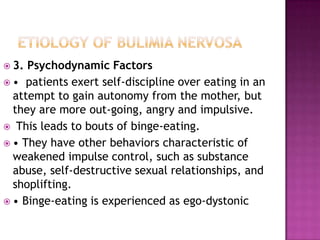
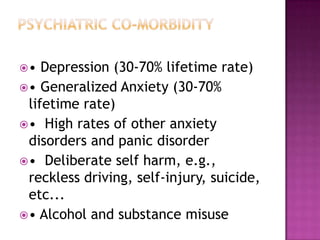
This document discusses eating disorders such as anorexia nervosa and bulimia nervosa. It covers the clinical picture, medical complications, risk factors, comorbidities, prognosis and treatment options. Anorexia is characterized by weight loss and fear of gaining weight while bulimia involves binge eating and compensatory behaviors. Both have higher prevalence in females and can lead to long term medical issues if not properly treated through psychotherapy and medication.