This document discusses eating disorders and provides an overview. The key points are:
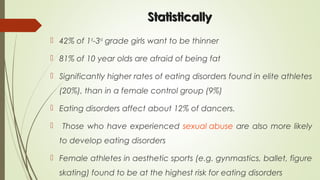
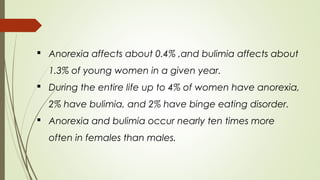
1. Eating disorders have increased threefold in the last 50 years and affect about 10% of the population, with 90% of cases being young women and girls.
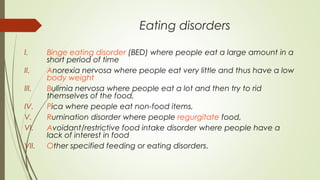
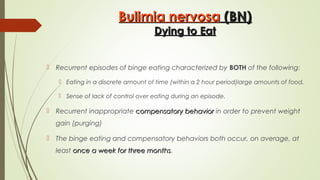
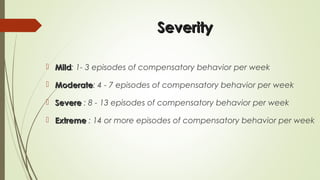
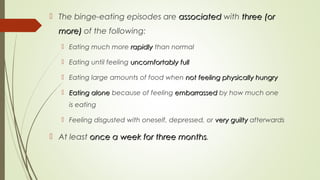
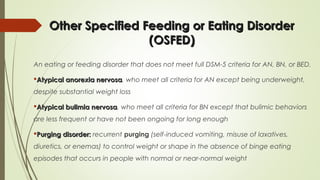
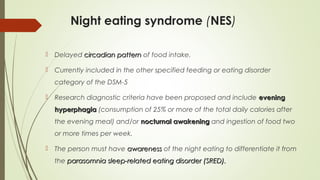
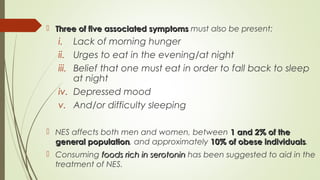
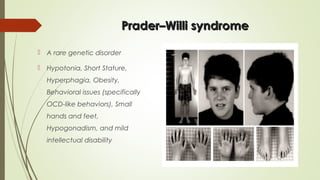
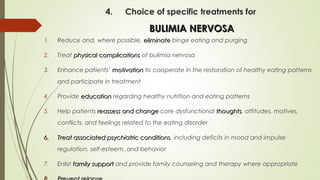
2. Eating disorders include conditions like anorexia nervosa, bulimia nervosa, binge eating disorder, and other specified feeding or eating disorders.
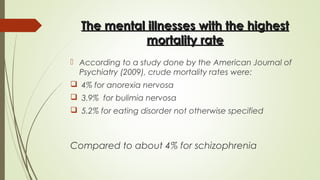
3. Anorexia nervosa and bulimia nervosa have the highest mortality rates of any mental illness according to studies, with crude mortality rates of 4-5.2%.