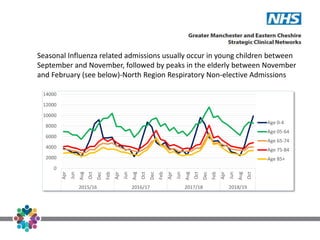
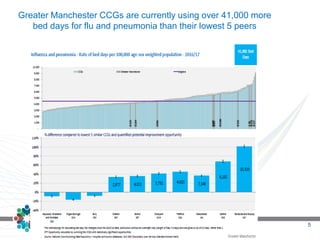
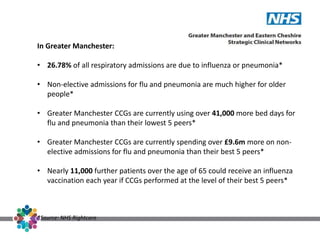
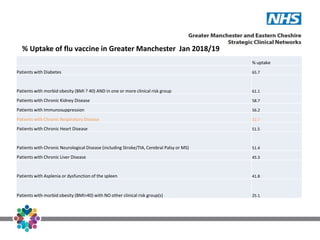
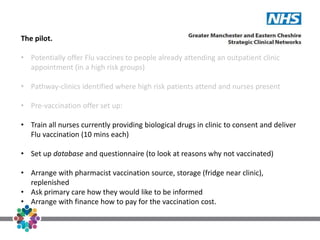
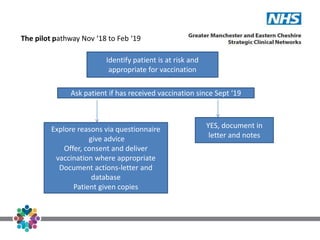
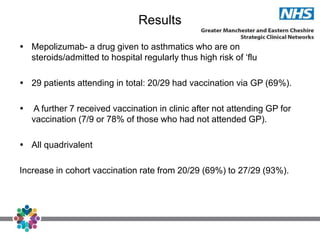
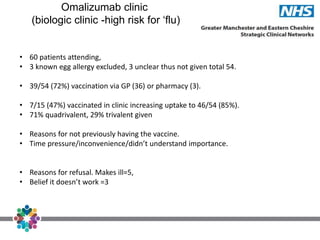
Respiratory admissions in Greater Manchester (GM) have risen significantly, with seasonal influenza being a major factor, leading to increased hospital bed usage and costs. The seasonal influenza vaccine is the most effective prevention method, yet vaccination rates among high-risk groups are low, necessitating initiatives to offer flu vaccinations in outpatient settings. A pilot program demonstrated that delivering vaccinations in clinics can improve uptake among at-risk patients, highlighting the importance of addressing knowledge barriers and convenience issues.