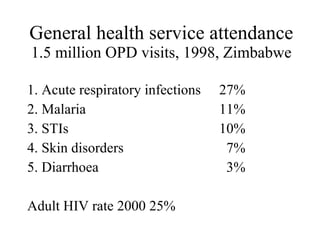
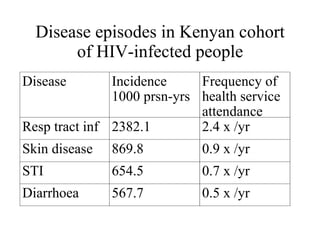
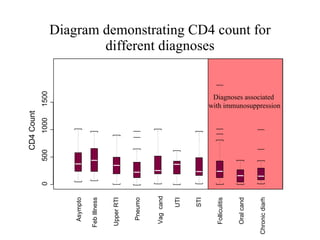
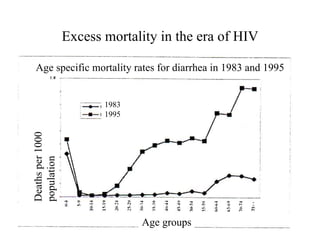
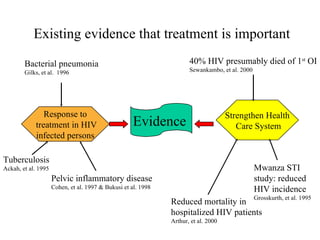
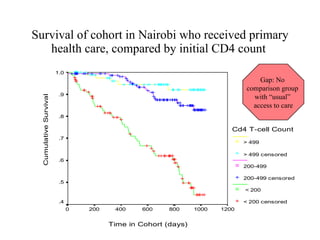
This document discusses the development of syndromic practice guidelines for primary care in high HIV prevalence settings. It argues that standardized case management can improve diagnosis, treatment, and referral. Common outpatient conditions like respiratory infections, malaria, and STIs represent a large portion of health service visits. While disease presentations in early stage HIV may not differ from non-infected individuals, adequate management of selected conditions can reduce mortality and improve quality of life for those with HIV. Further research is still needed on treating certain conditions like pneumonia to help develop standardized syndromic guidelines.