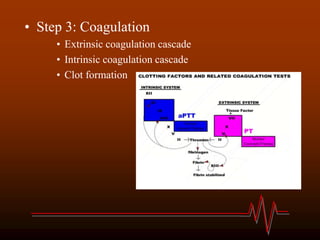
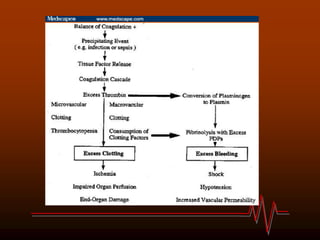
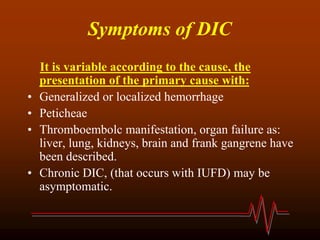
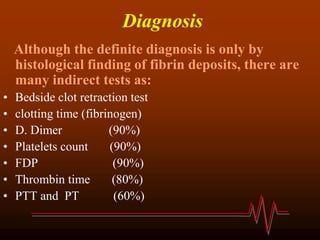
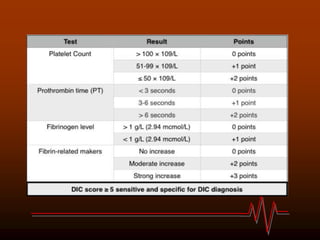
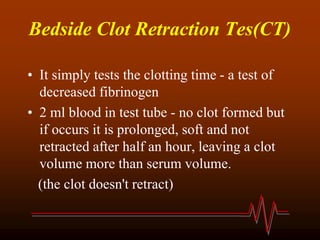
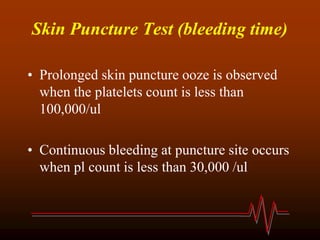
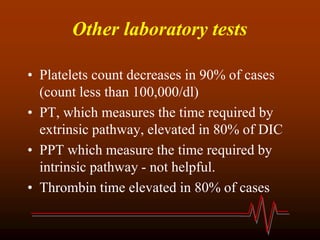
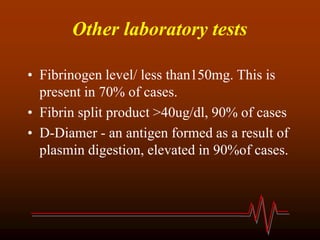
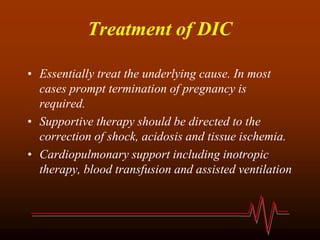
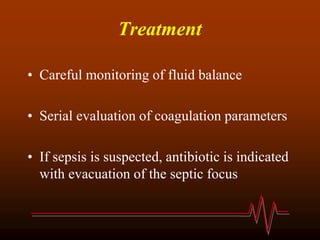
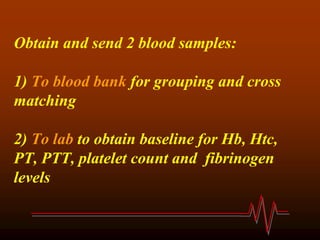
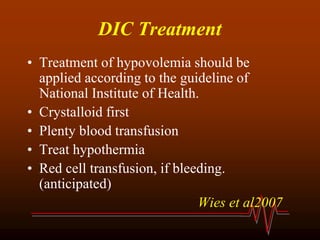
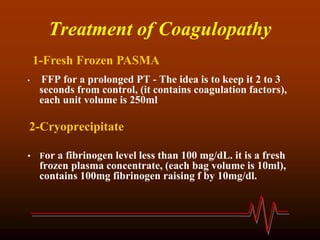
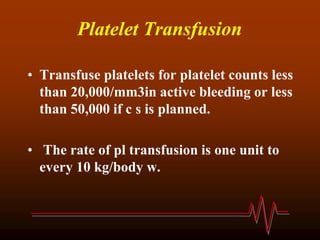
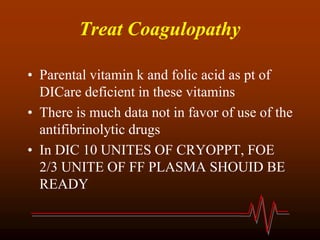
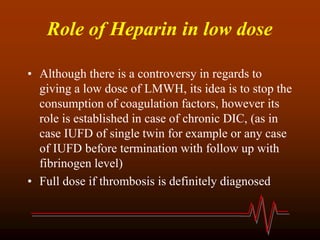
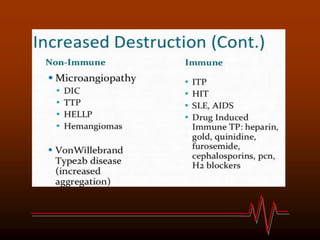
Disseminated intravascular coagulation (DIC) is a pathological condition associated with activation of both the coagulation system and fibrinolytic system. It is considered a secondary phenomenon caused by an underlying disease. DIC can be acute, beginning with clotting in small blood vessels leading to serious bleeding, or chronic, causing blood clotting but usually not bleeding. Common causes include sepsis, trauma, cancer, pregnancy complications, and transfusion. Diagnosis involves tests showing decreased platelets, elevated D-dimer and fibrin split products, prolonged clotting times, and low fibrinogen. Treatment focuses on treating the underlying cause, supportive care, and replacing clotting factors, platelets, and fibrinogen.