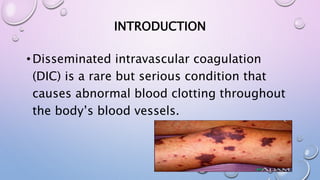
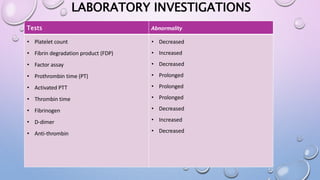
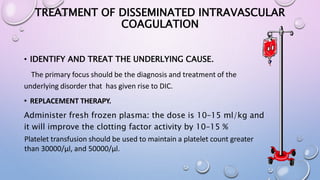
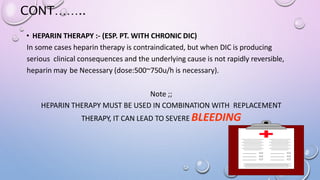
Disseminated intravascular coagulation (DIC) is a serious condition where abnormal blood clotting occurs throughout the body's blood vessels. It involves both excessive clotting and bleeding. DIC can be acute or chronic. Acute DIC develops rapidly and is associated with infection, trauma, or surgery. Chronic DIC develops slowly, often with cancer. Treatment focuses on treating the underlying cause, replacing clotting factors, and controlling clotting with heparin. Complications can include organ damage, hemorrhage, and death. The prognosis depends on the severity and cause, with an overall mortality rate of 10-50%.