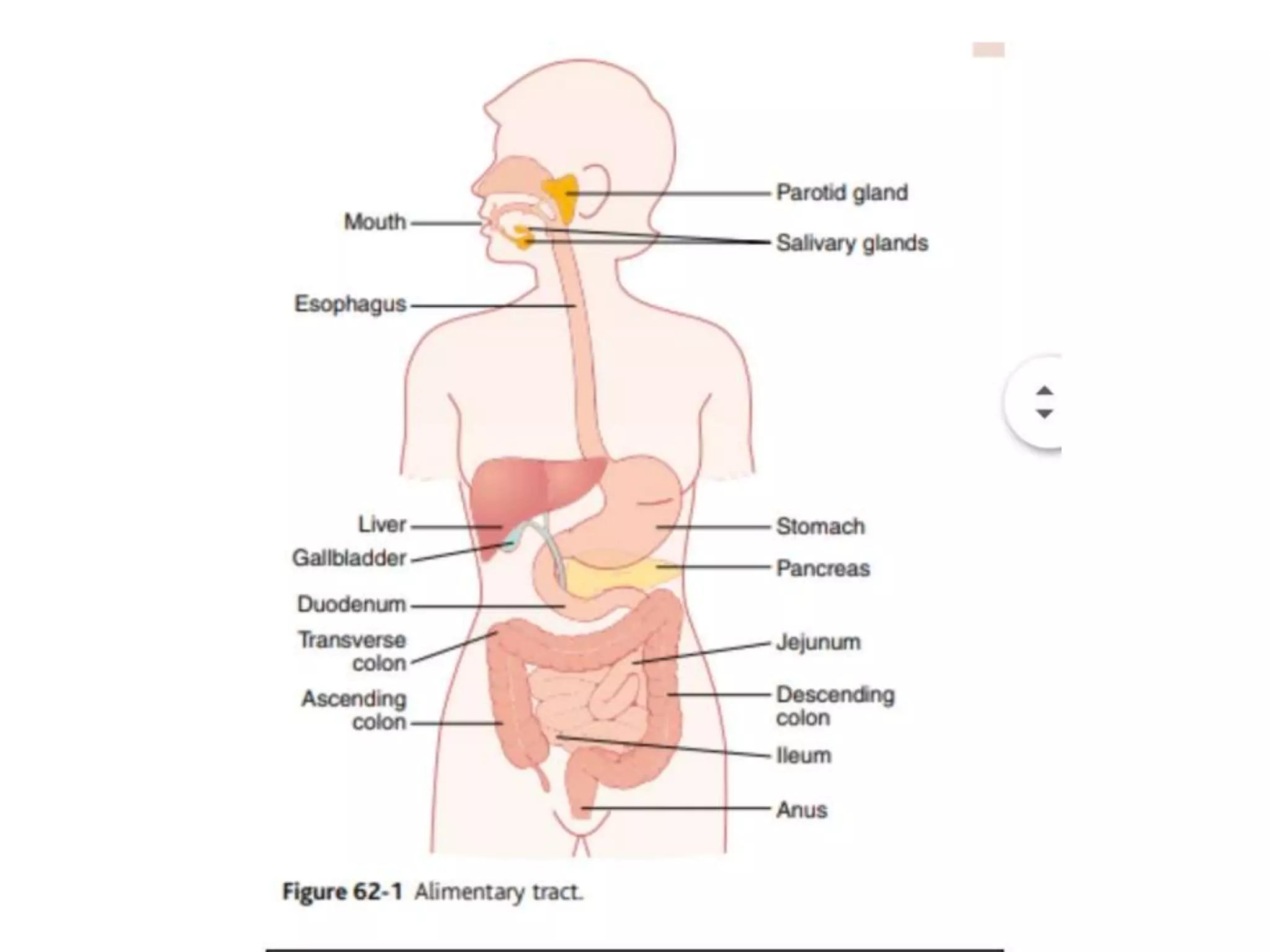
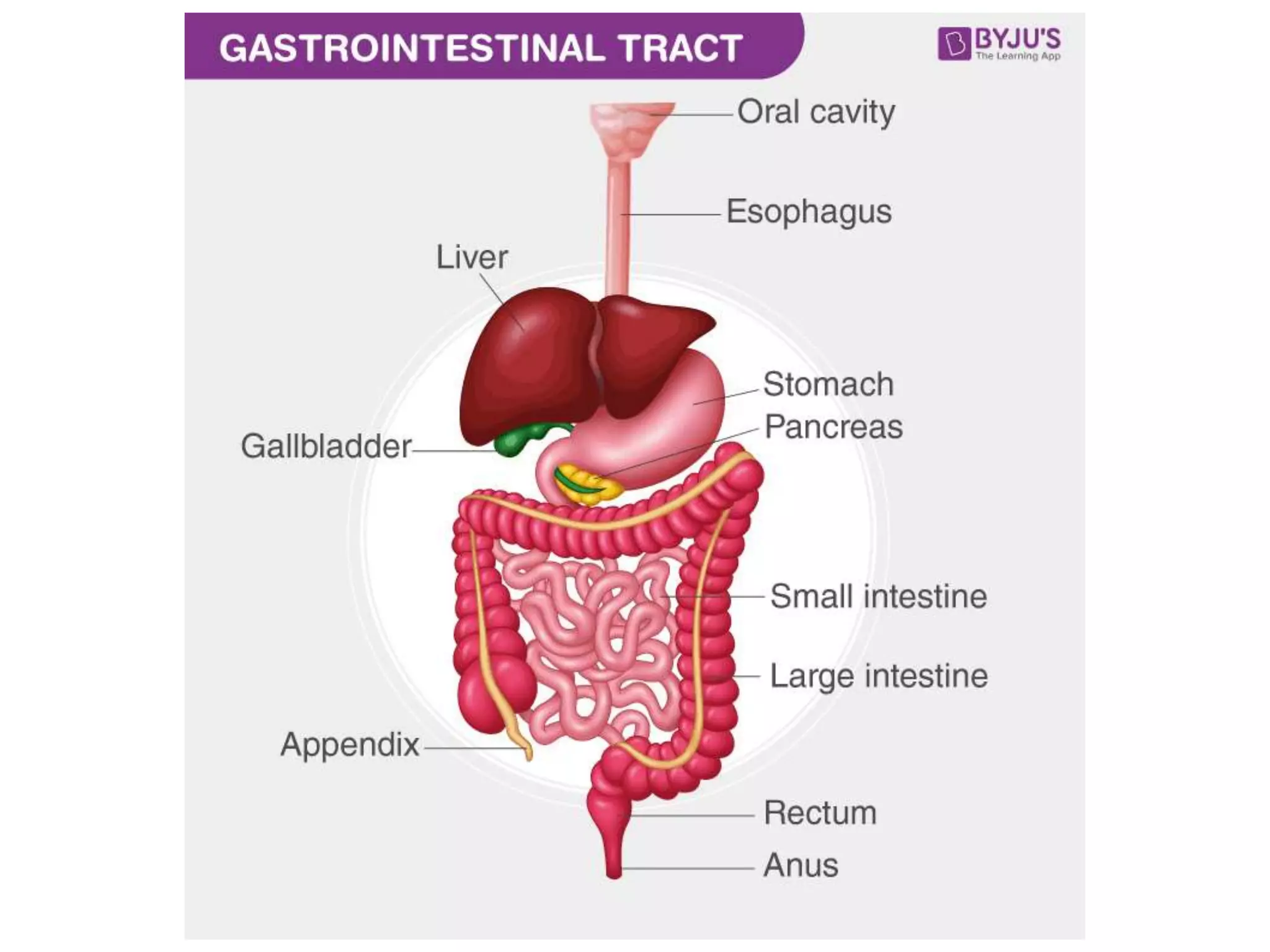
The digestive system breaks down food into nutrients that can be absorbed and used by the body. It has four main functions - ingestion, digestion, absorption, and egestion.
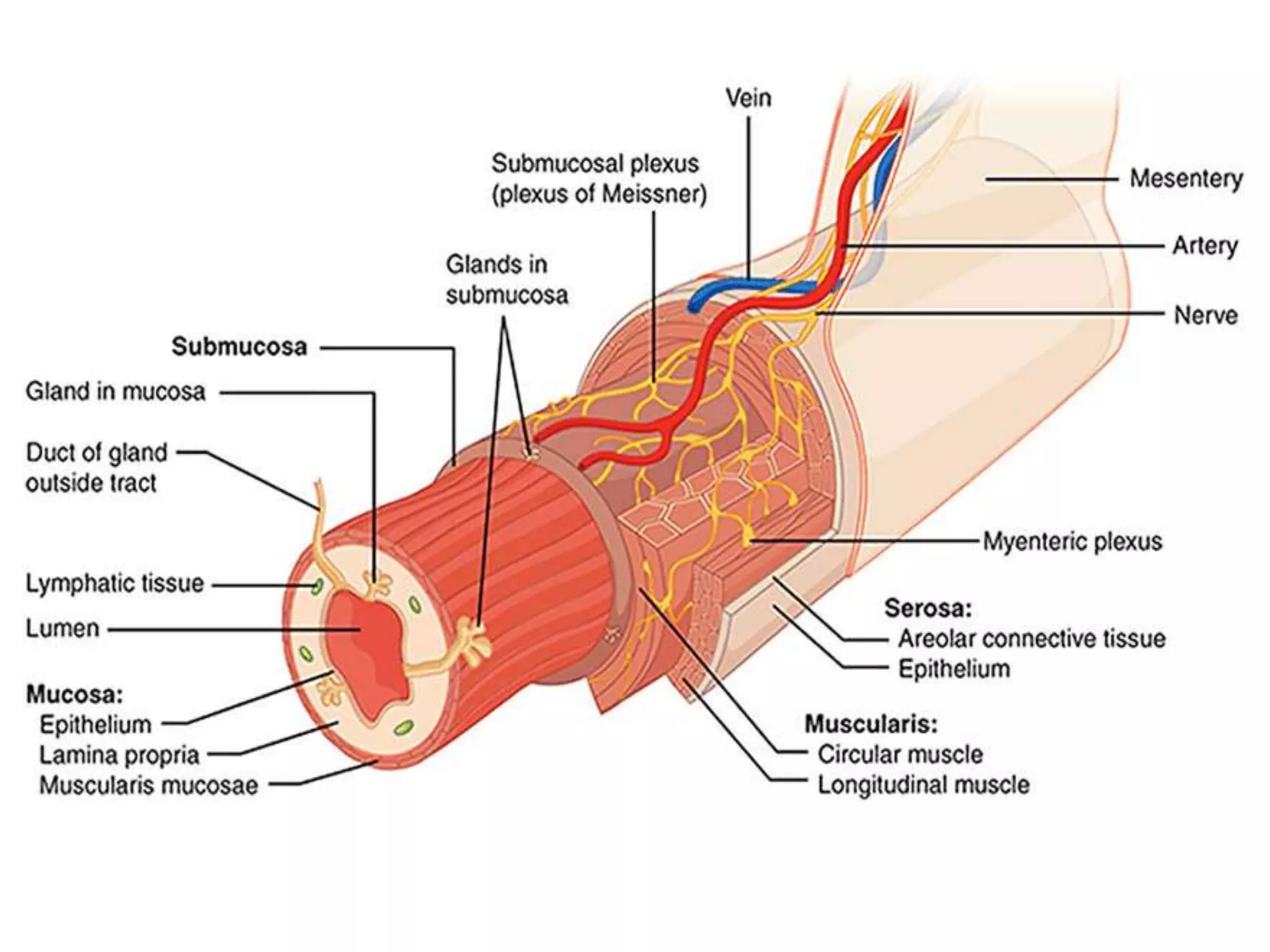
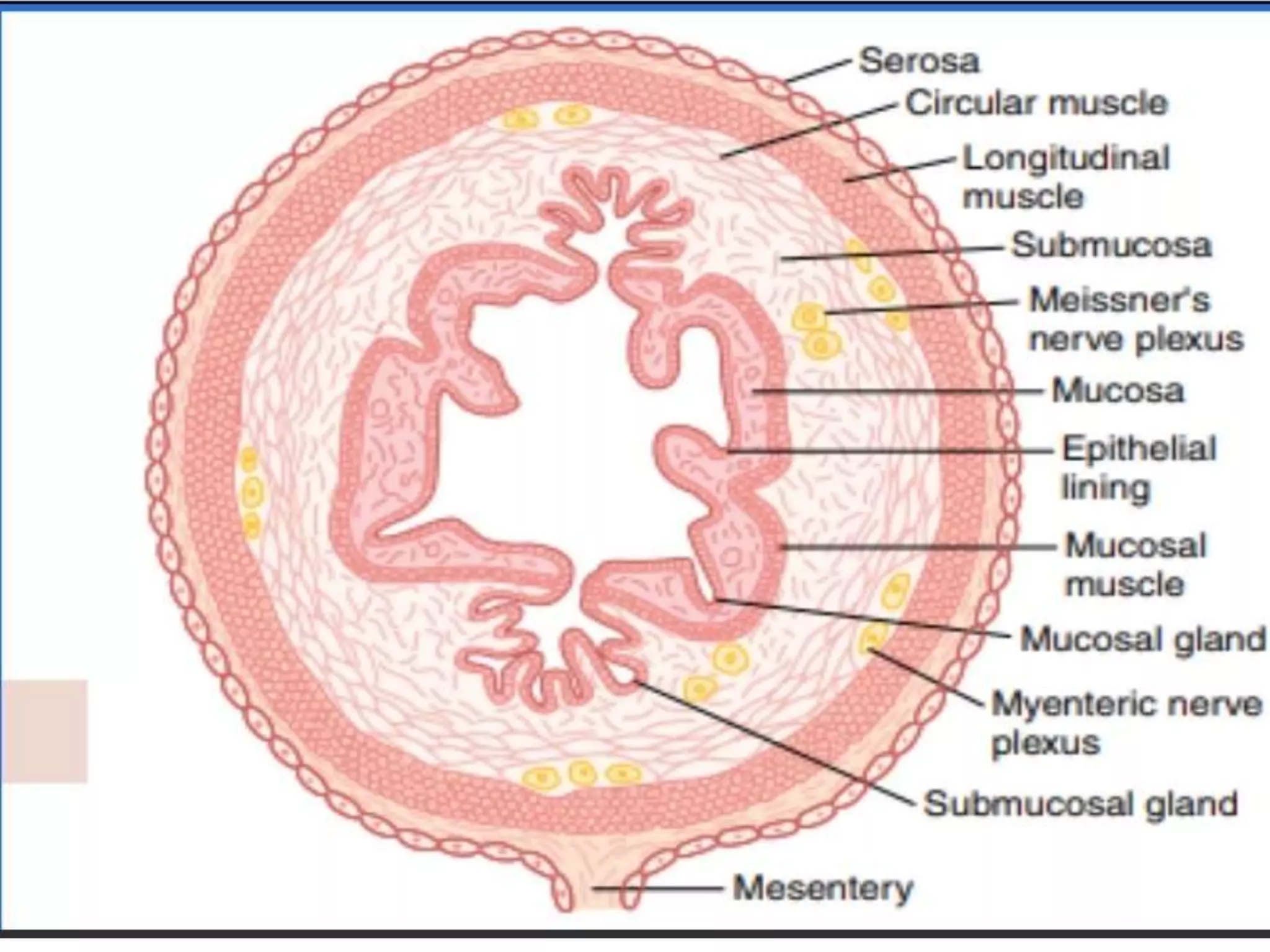
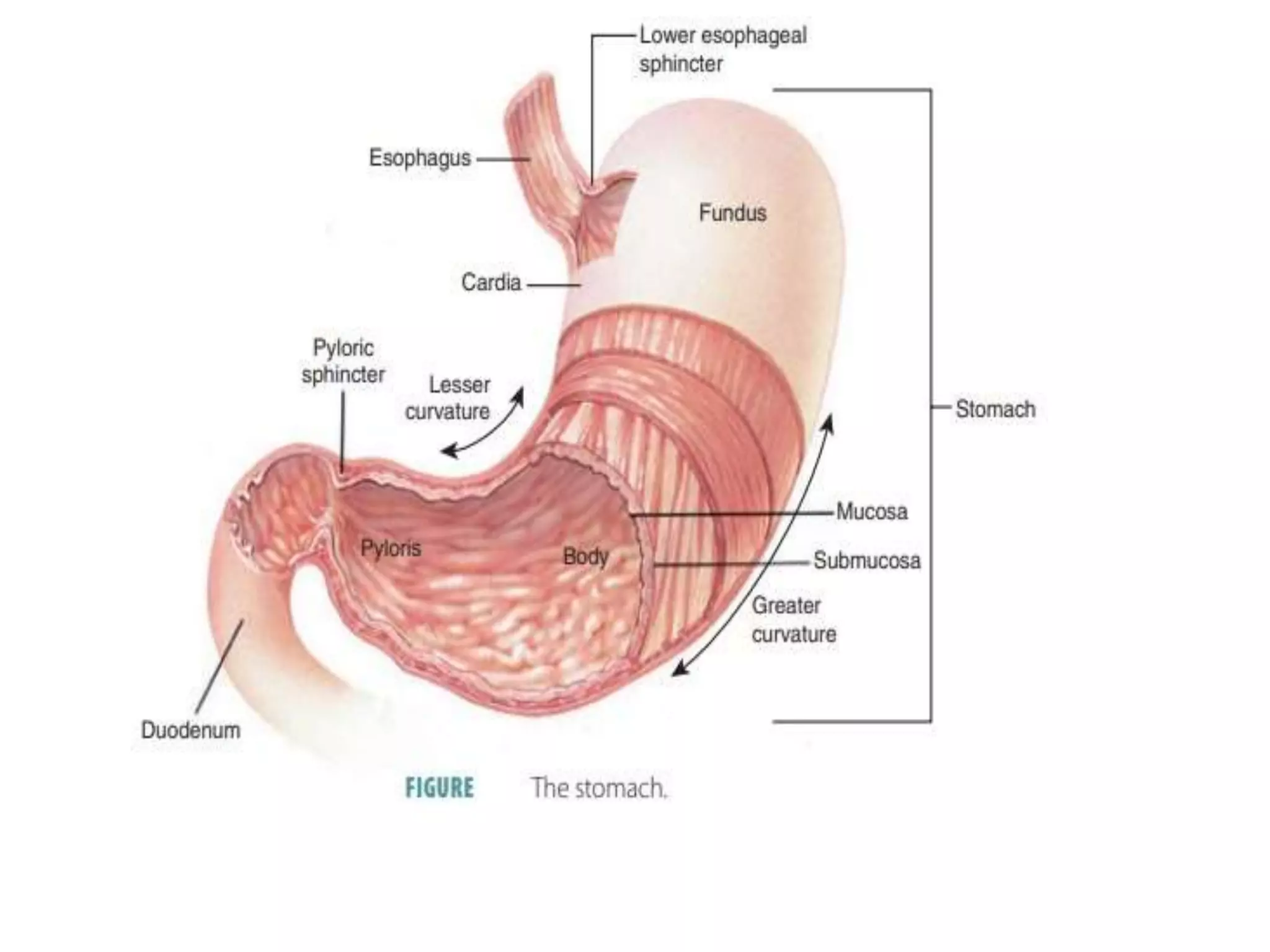
The gastrointestinal tract has four layers - mucosa, submucosa, muscularis and serosa. The mucosa contains the epithelial lining, lamina propria and muscularis mucosa.
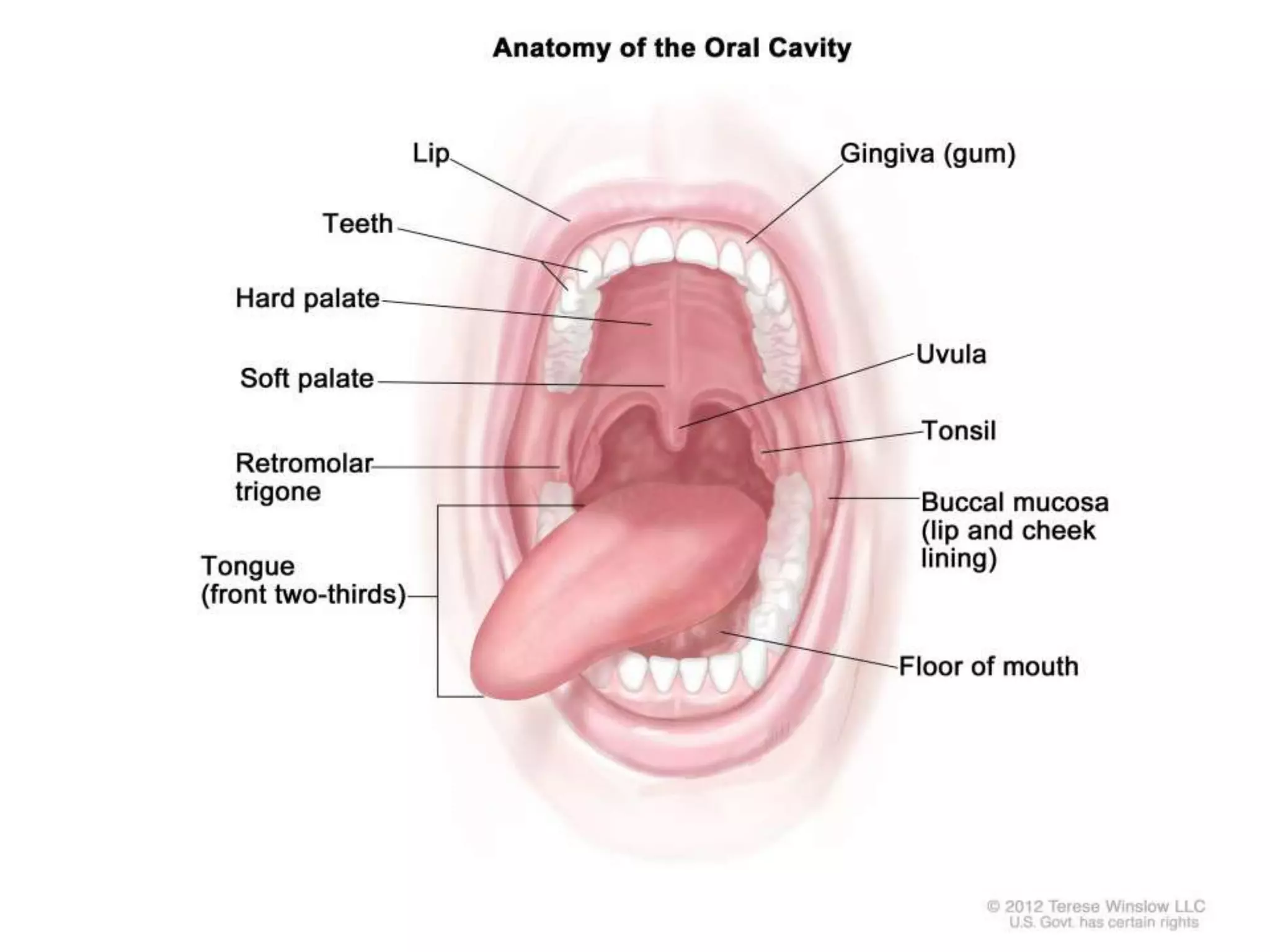
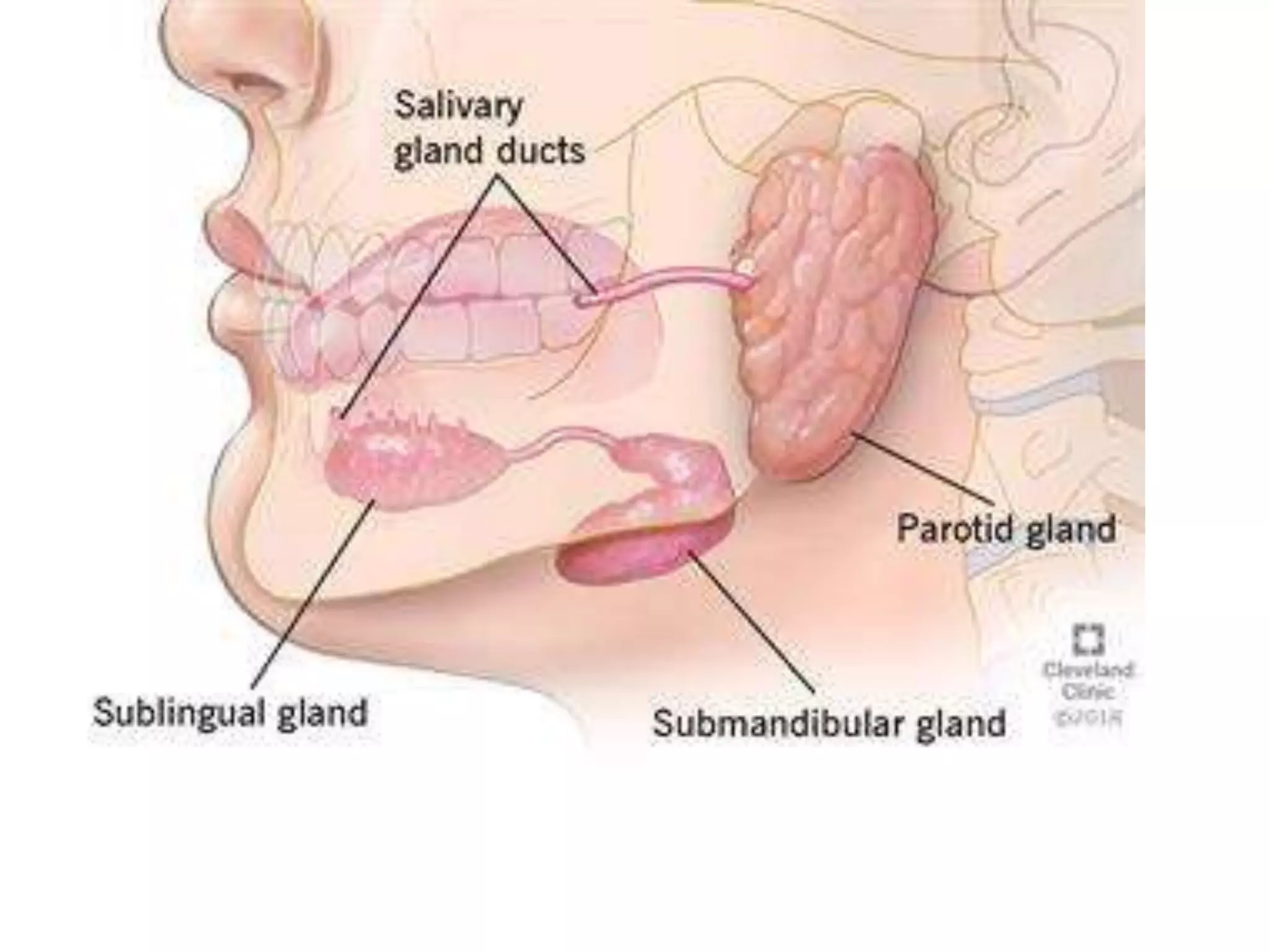
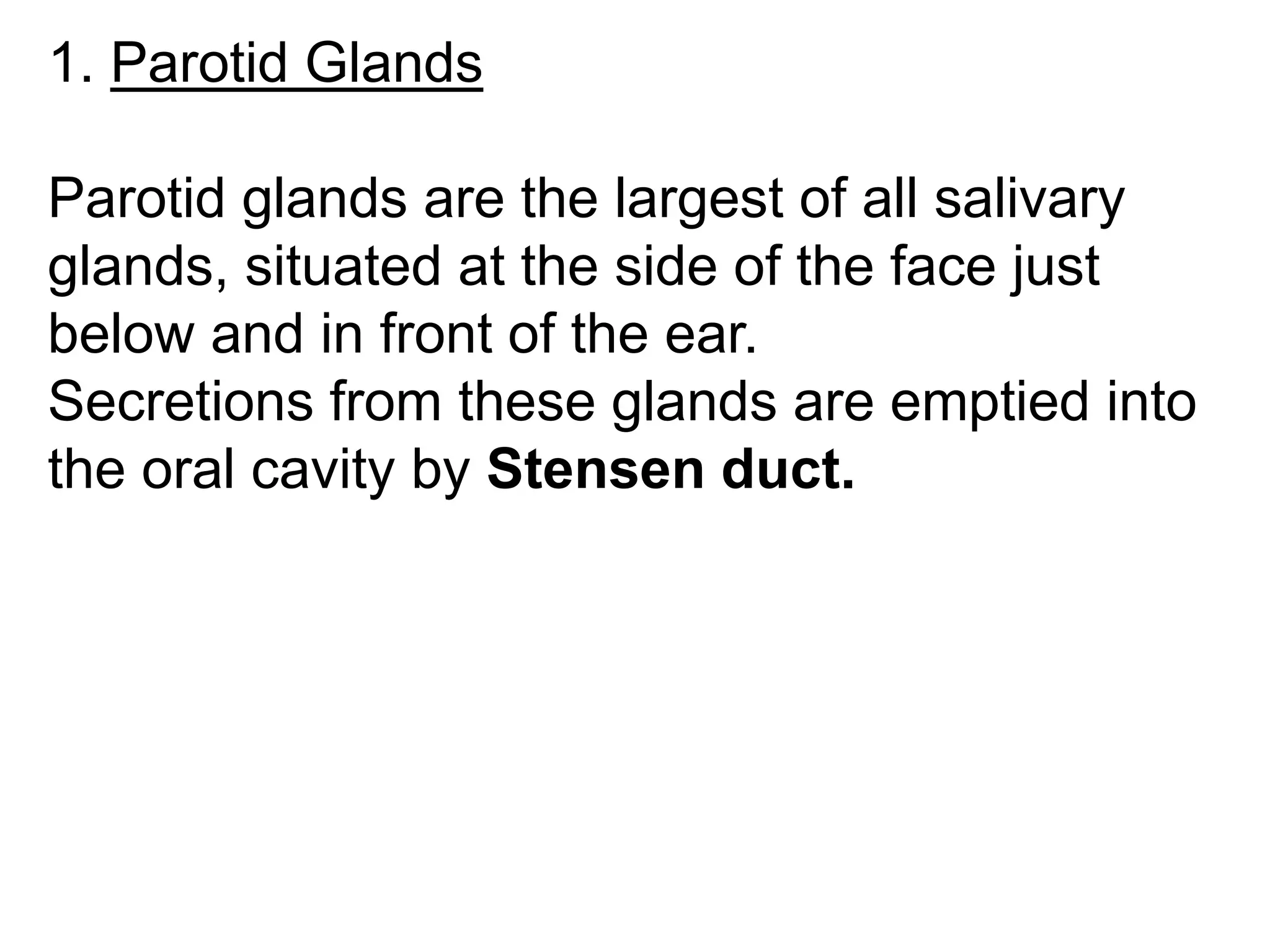
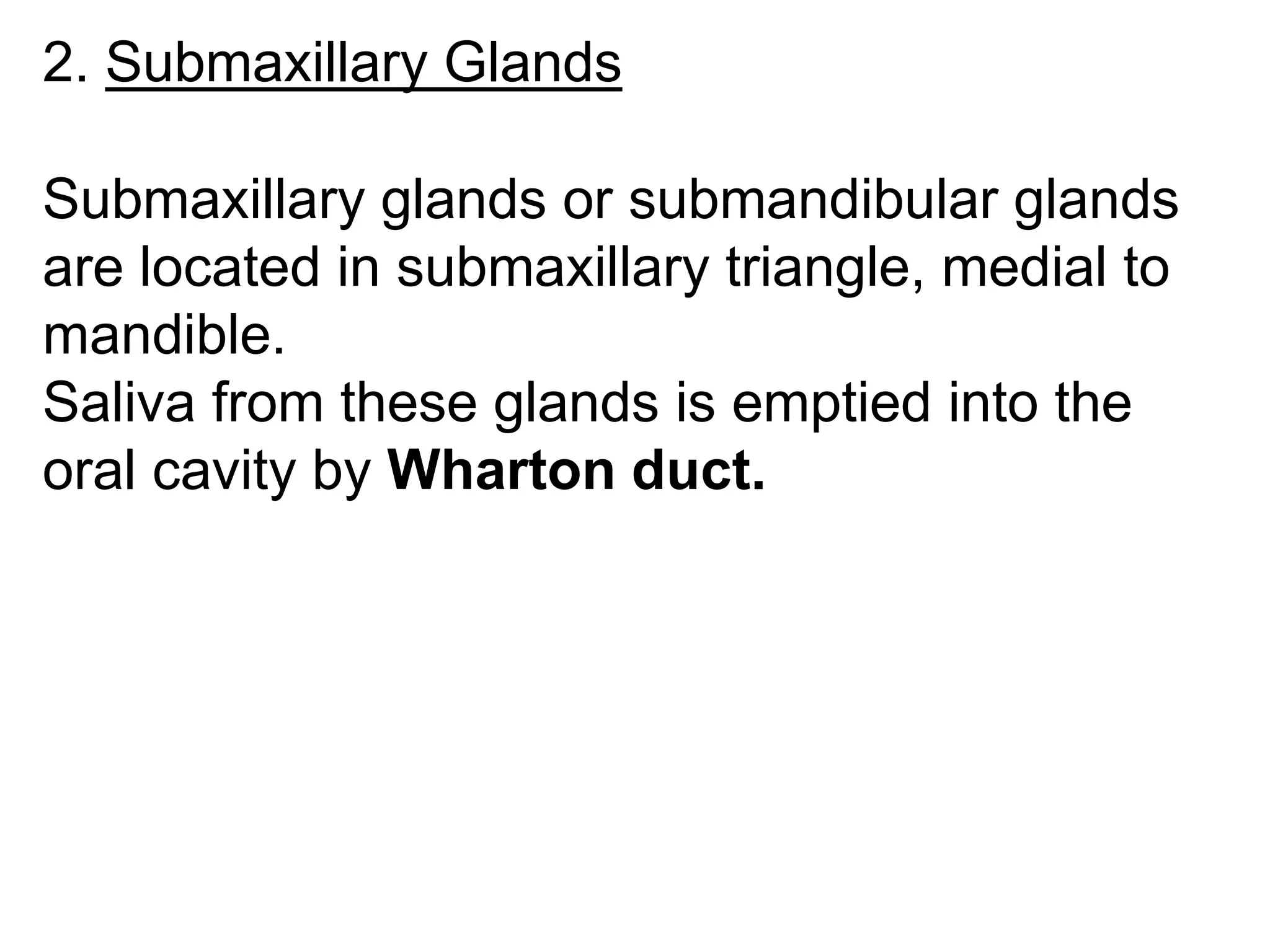
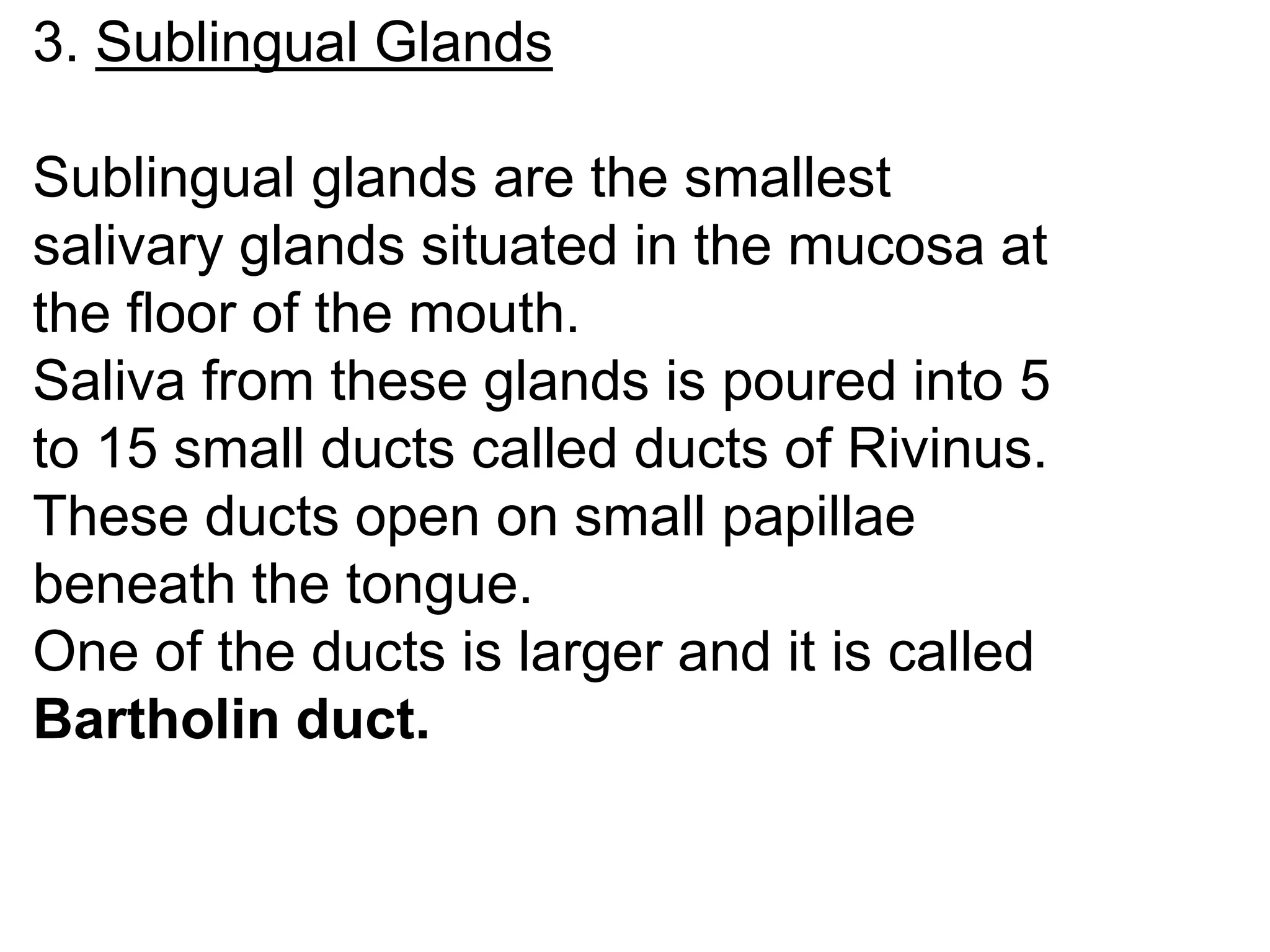
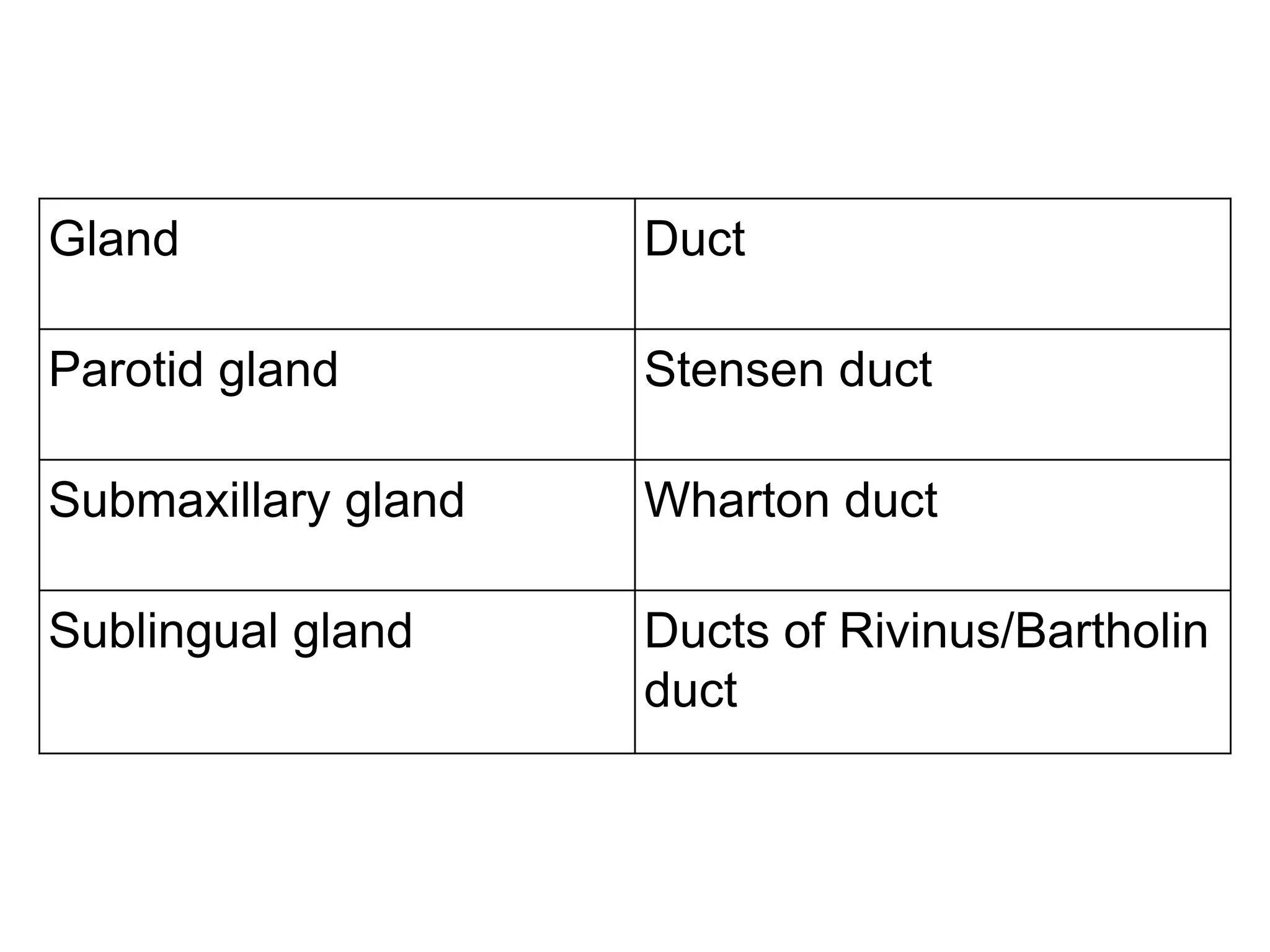
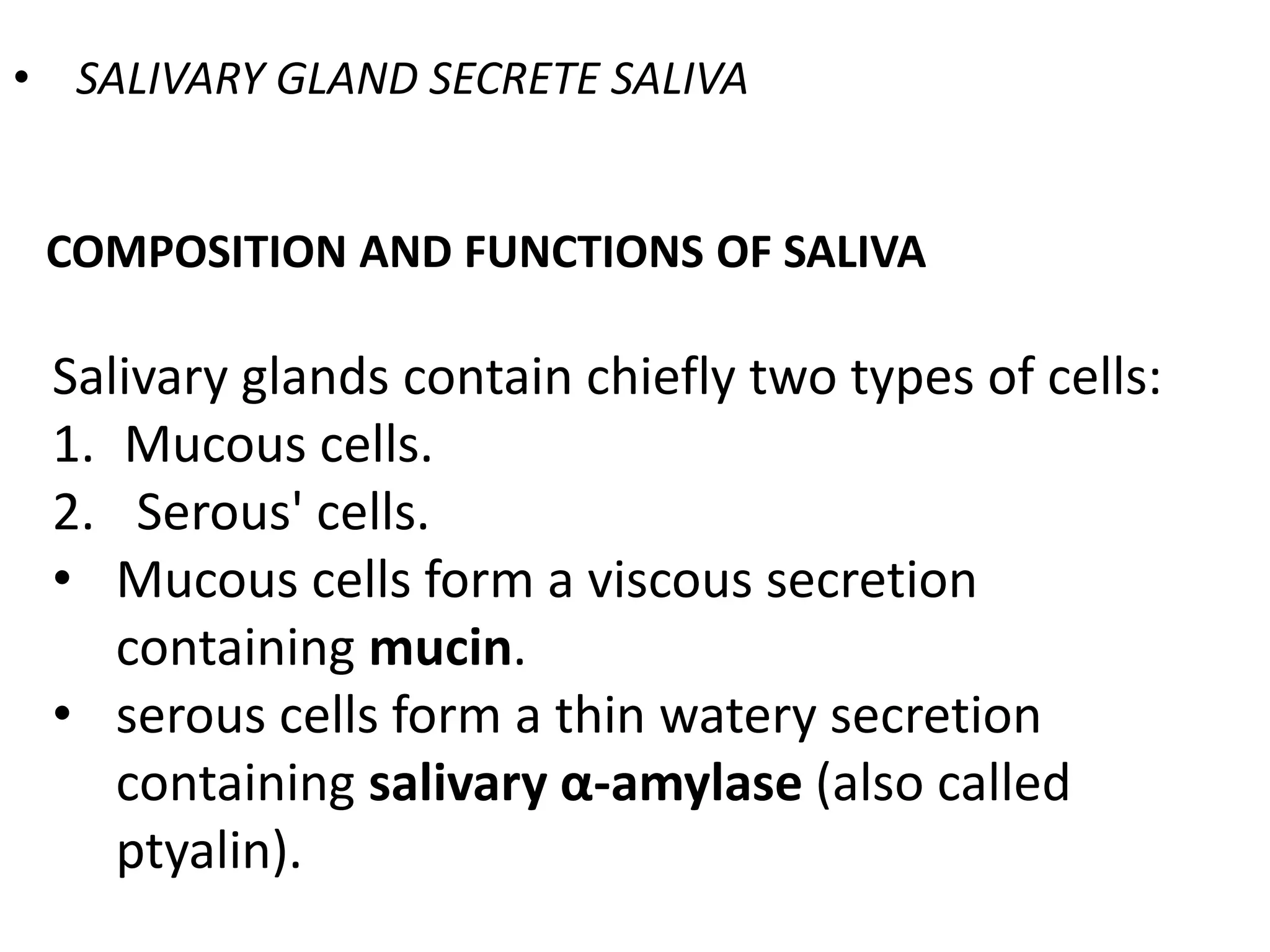
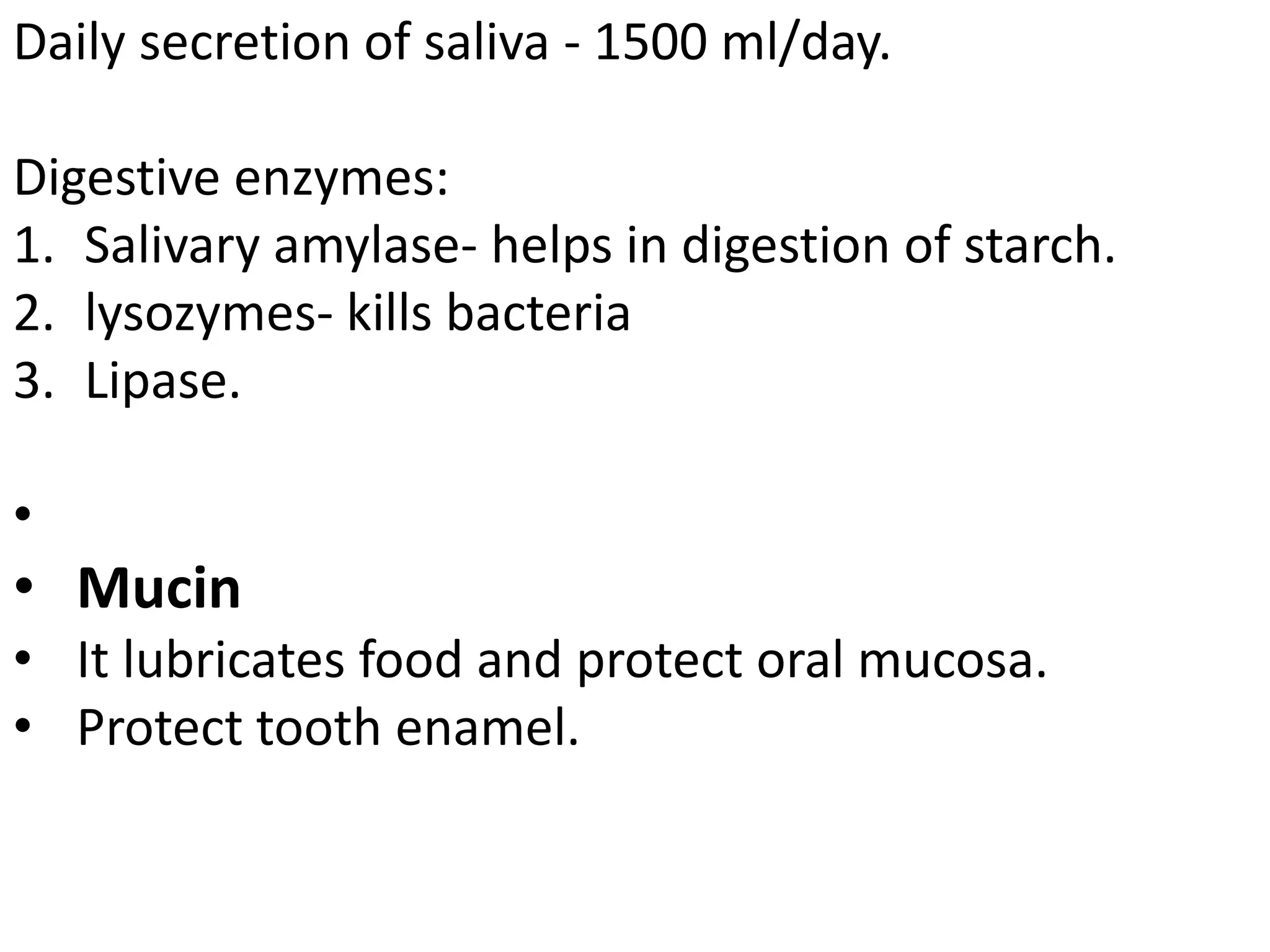
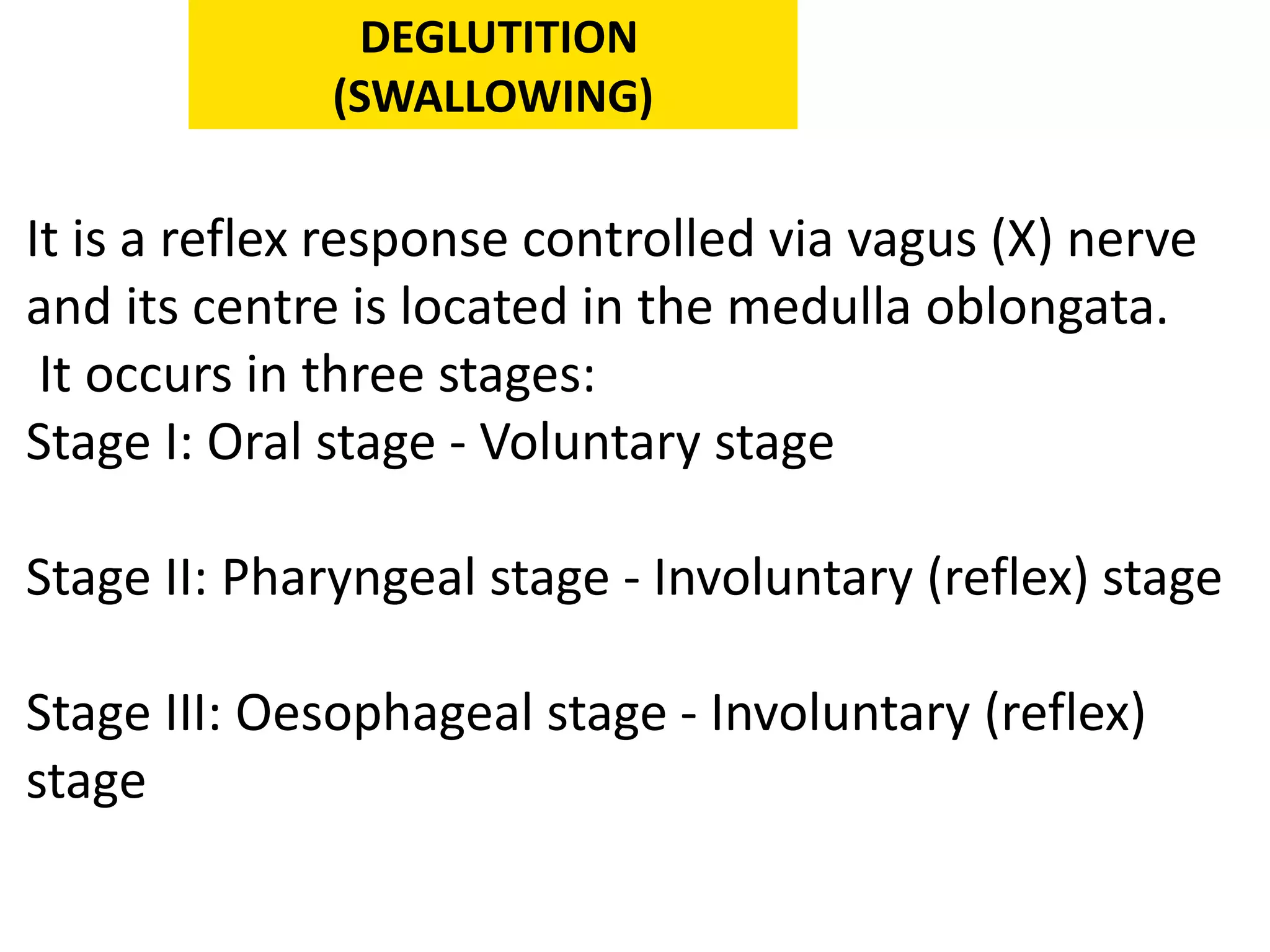
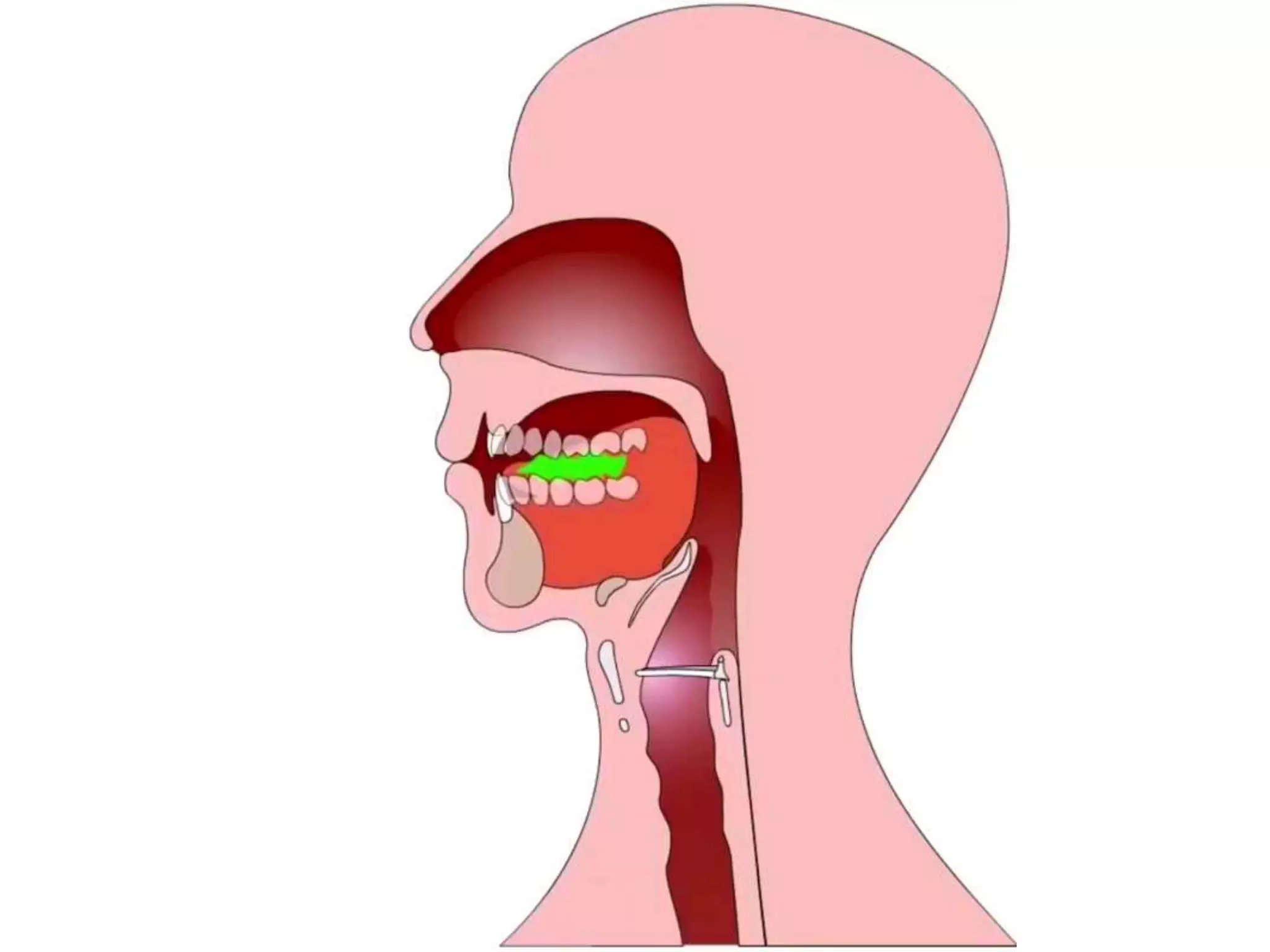
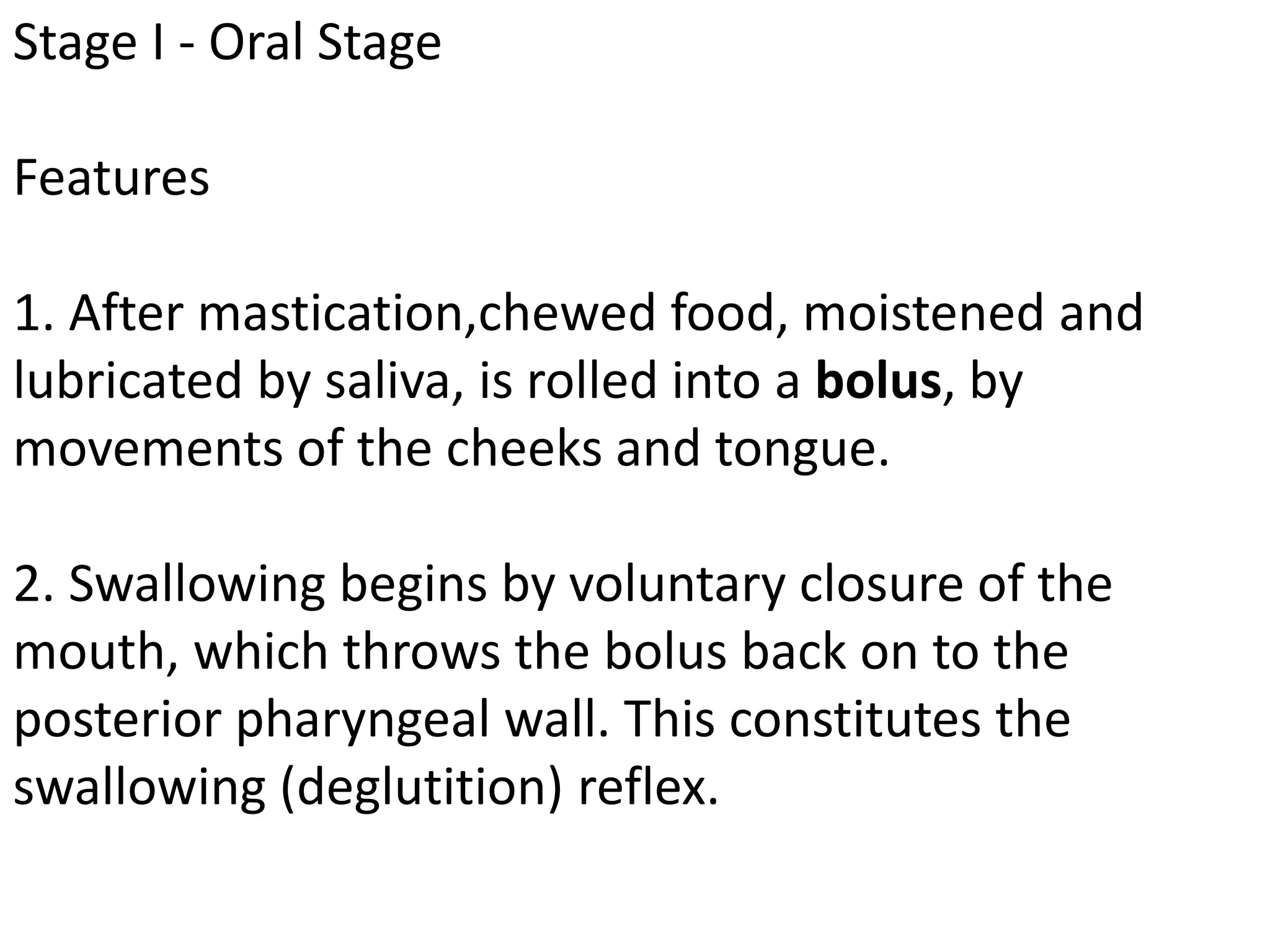
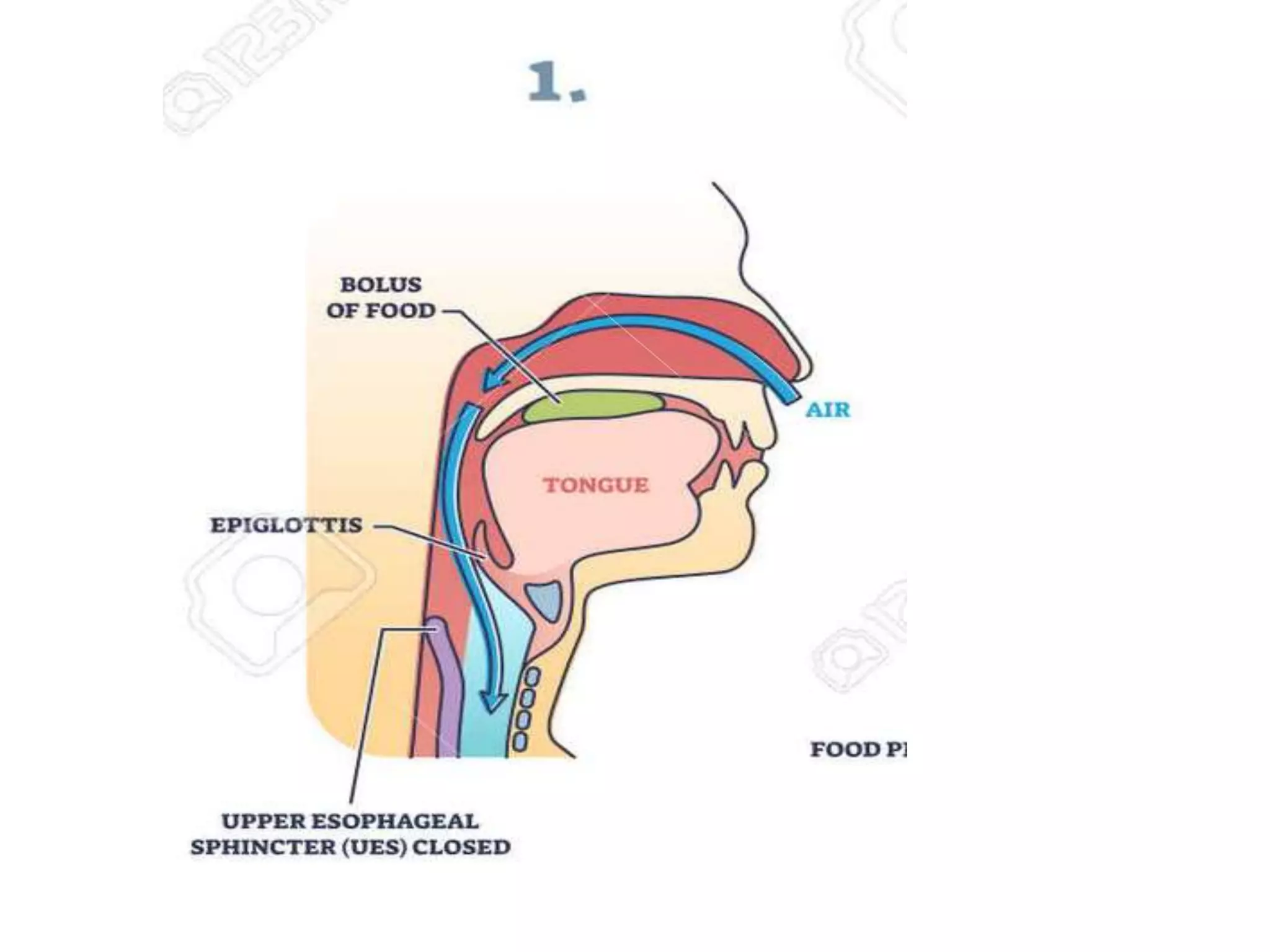
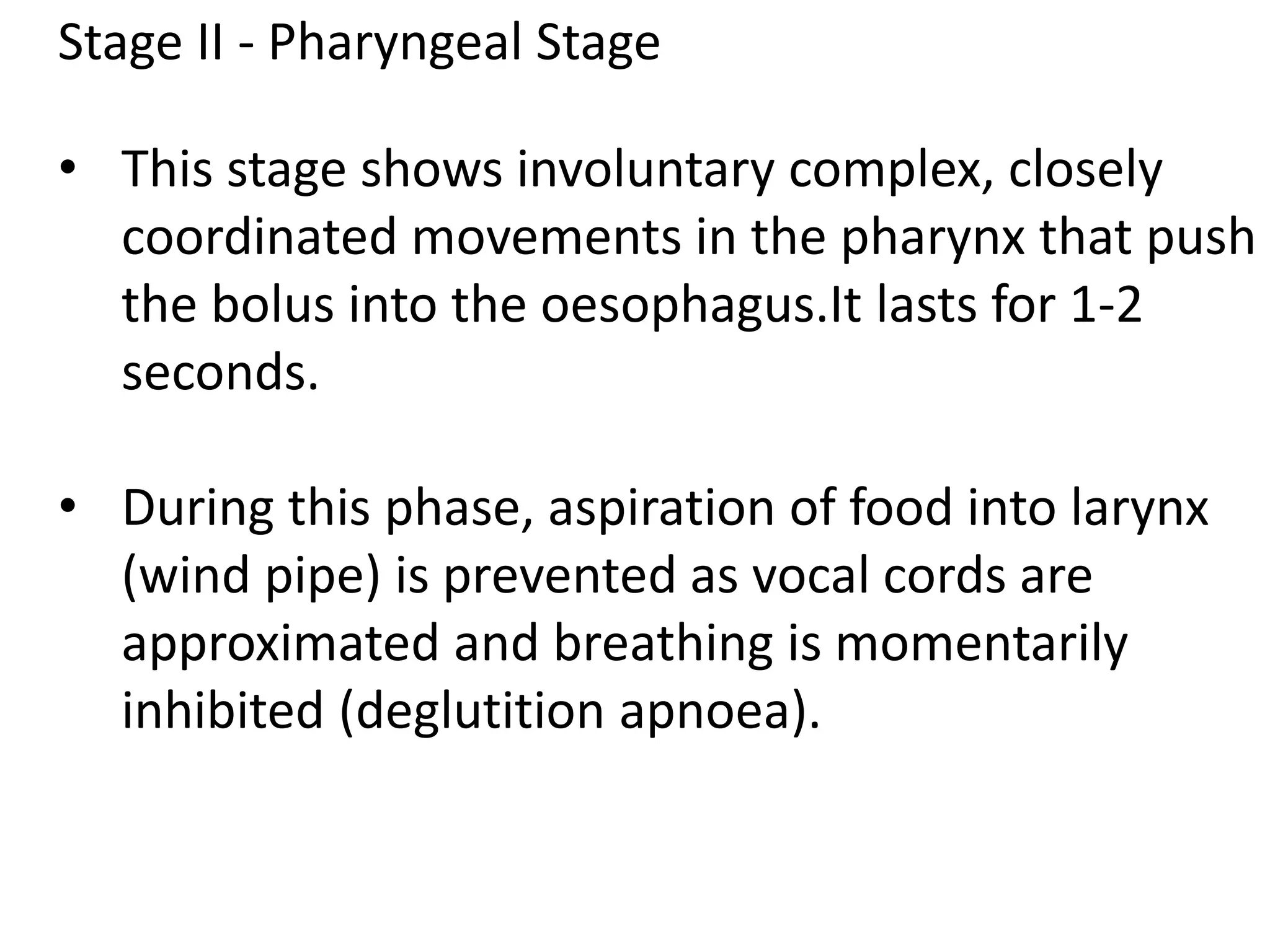
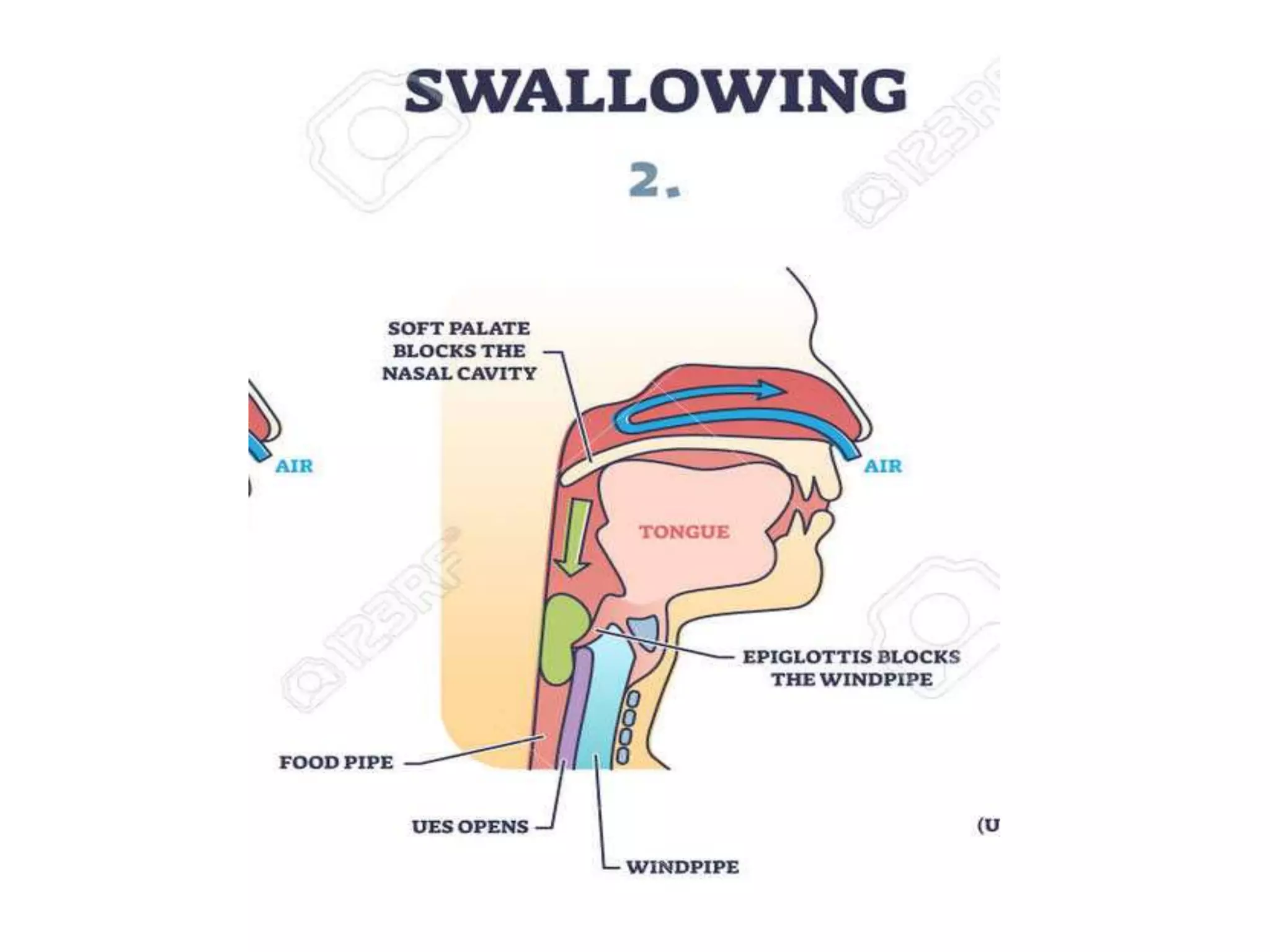
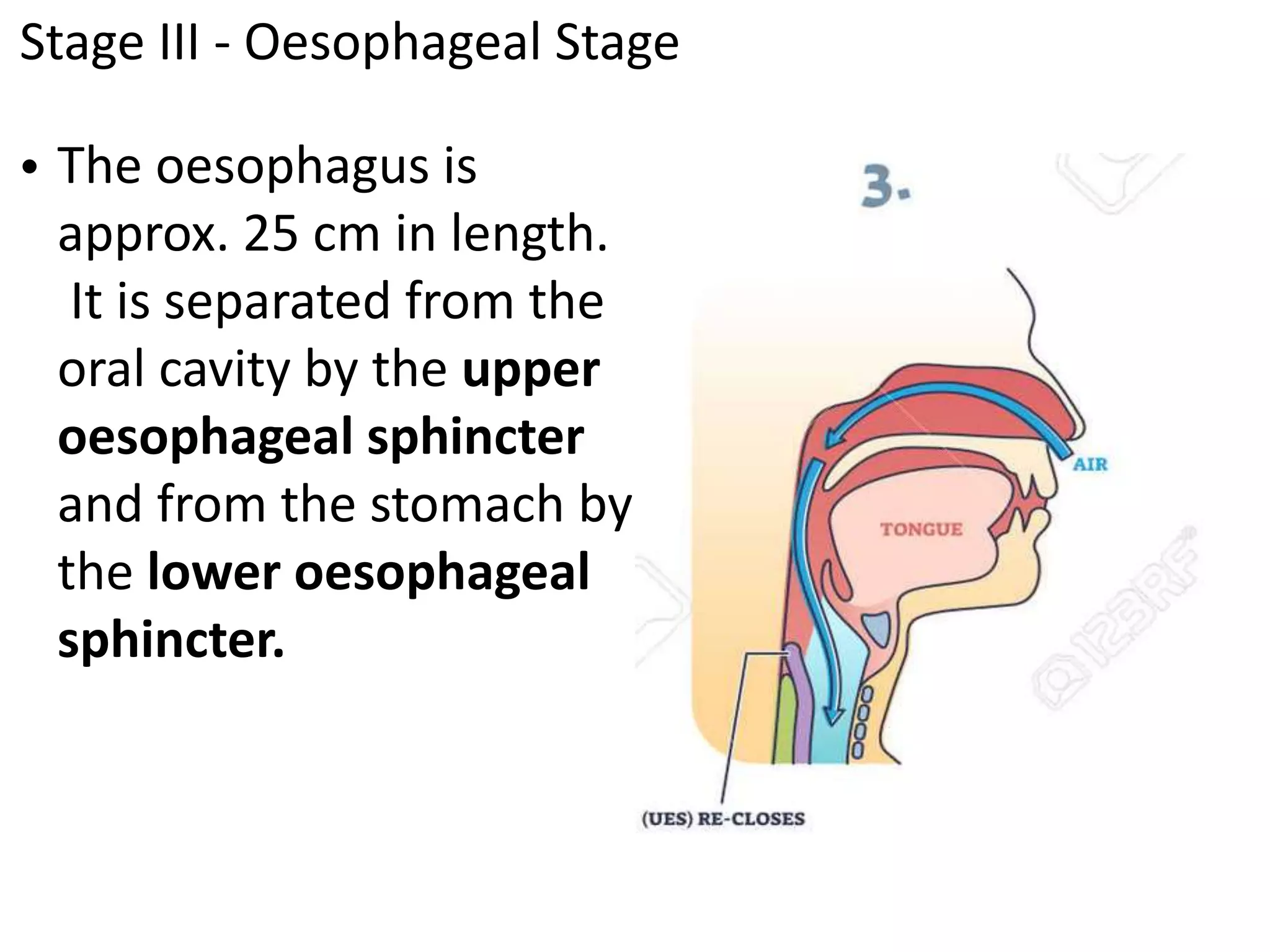
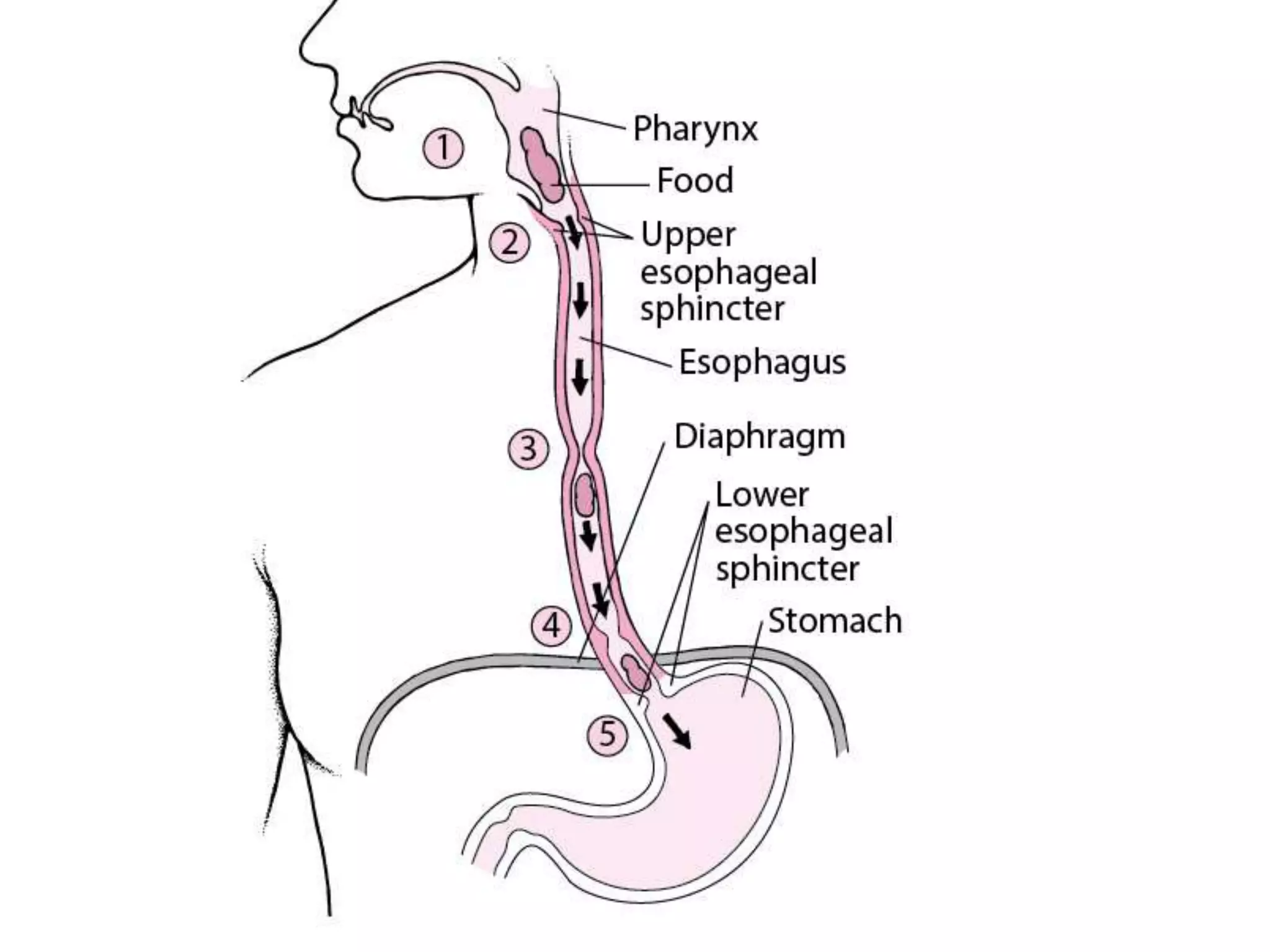
The mouth's functions include ingestion, chewing, tasting and swallowing food. Saliva contains amylase and is produced by the parotid, submandibular and sublingual glands. Swallowing has three stages - oral, pharyngeal and esophageal. Peristalsis propels food through the