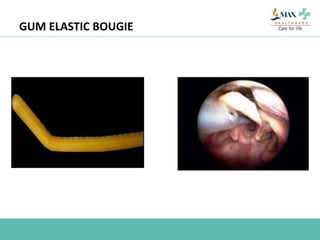
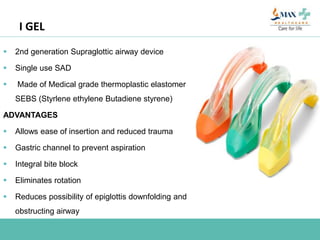
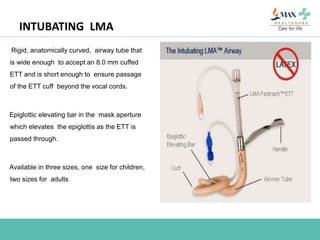
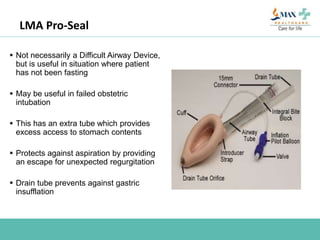
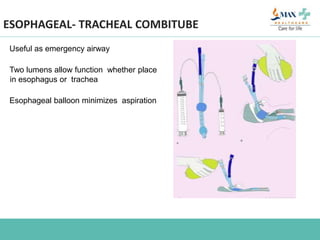
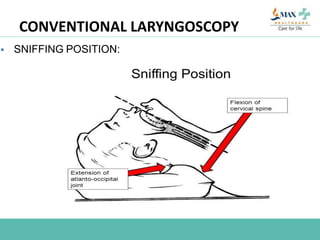
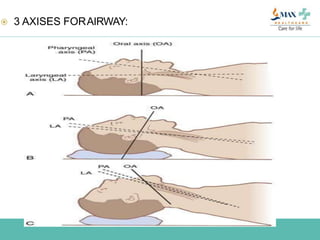
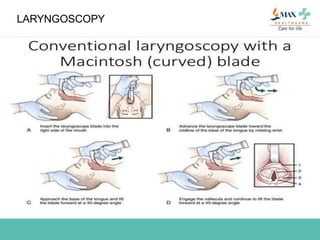
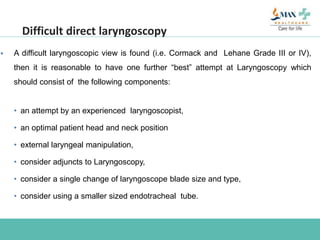
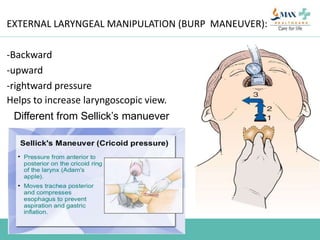
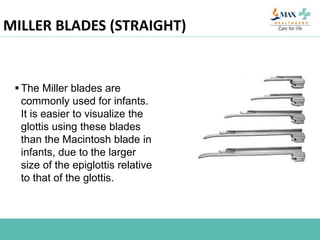
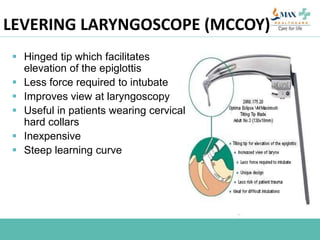
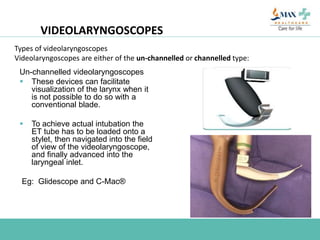
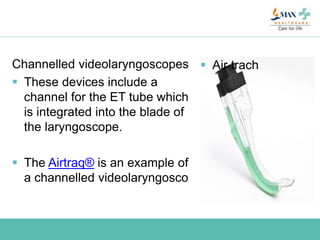
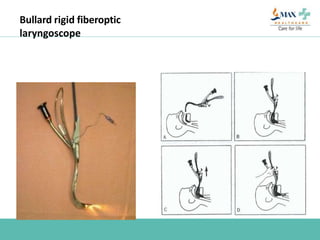
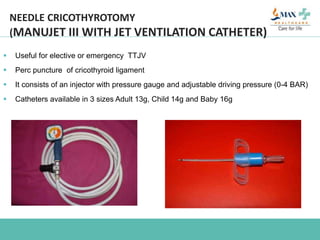
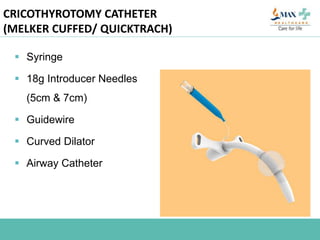
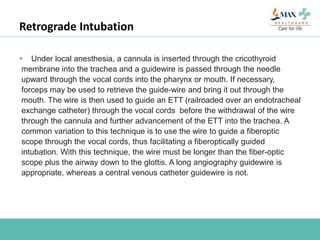
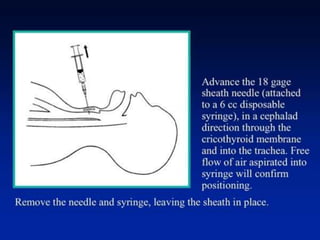
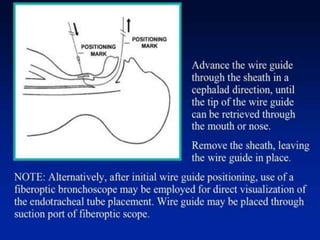
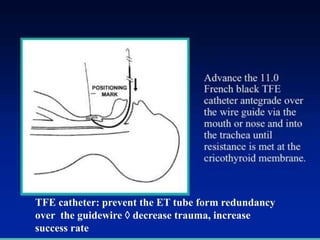
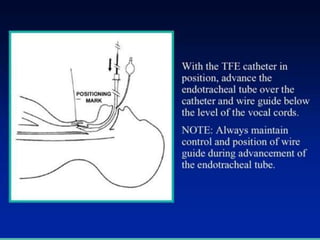
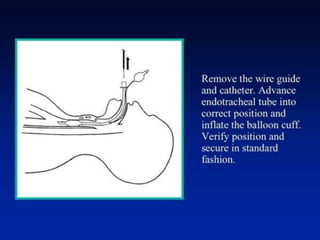
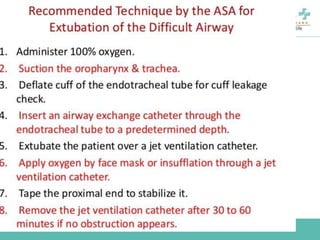
The document discusses difficult airway management in the ICU. It begins by defining difficult mask ventilation and difficult tracheal intubation. It then discusses managing the anticipated difficult airway, unanticipated difficult airway, and cannot intubate cannot ventilate scenarios. Various airway devices and techniques are described for establishing an airway, including awake intubation, fiberoptic intubation, bougie, lightwand, supraglottic airways, and surgical airways like needle cricothyrotomy. Factors like blade selection, external laryngeal manipulation, and videolaryngoscopy are also covered to optimize first attempt intubation success in difficult airways.