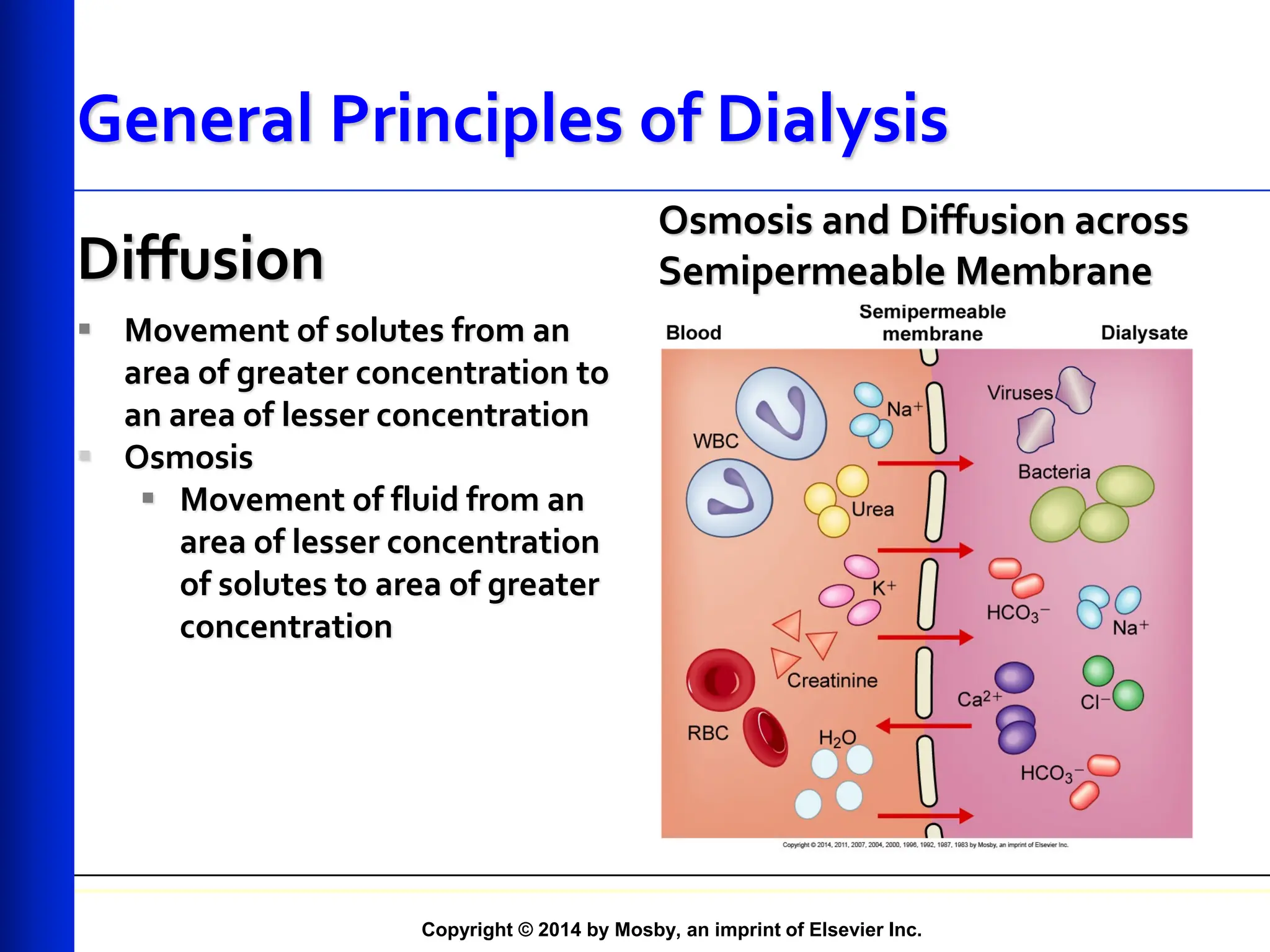
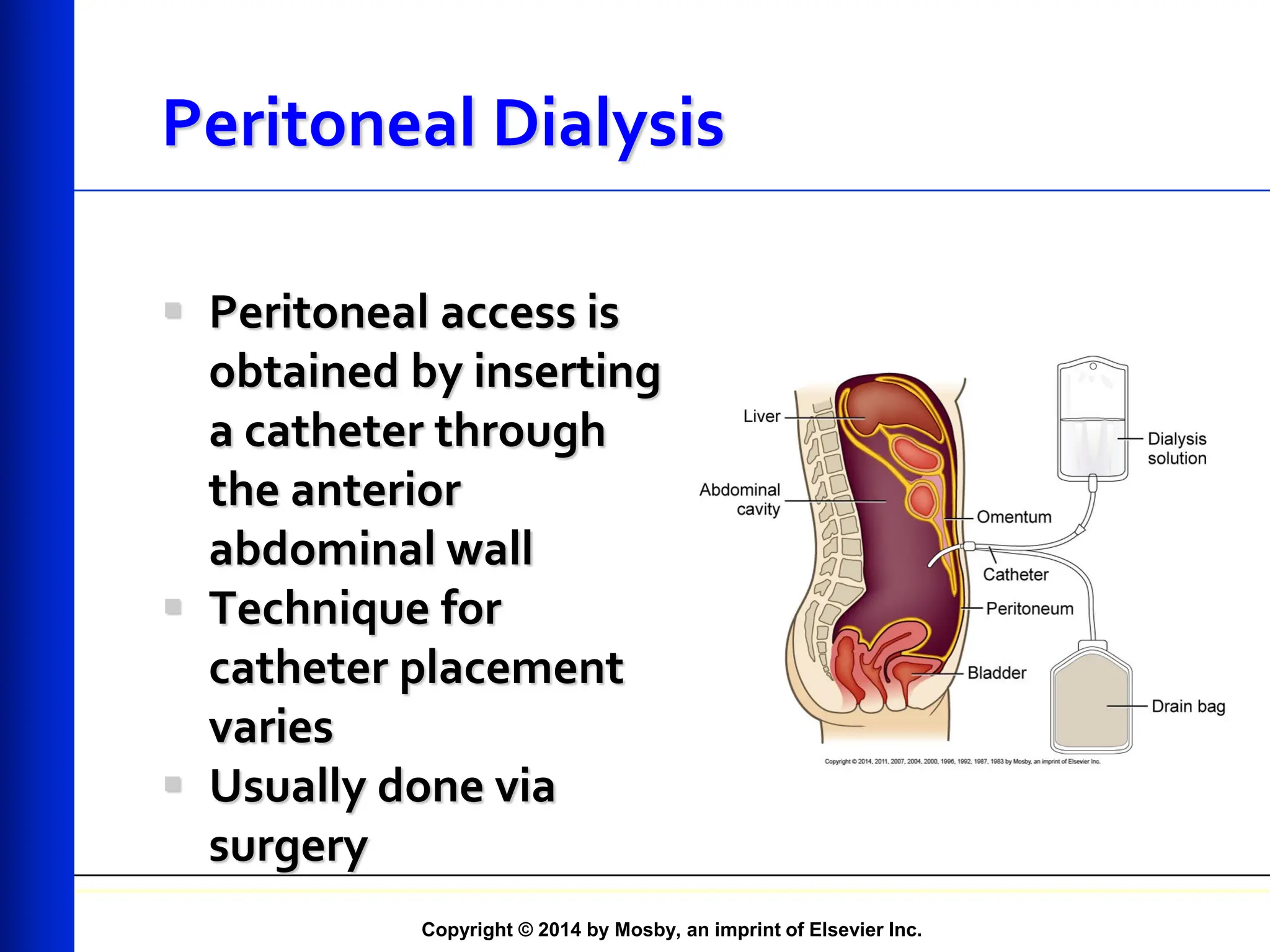
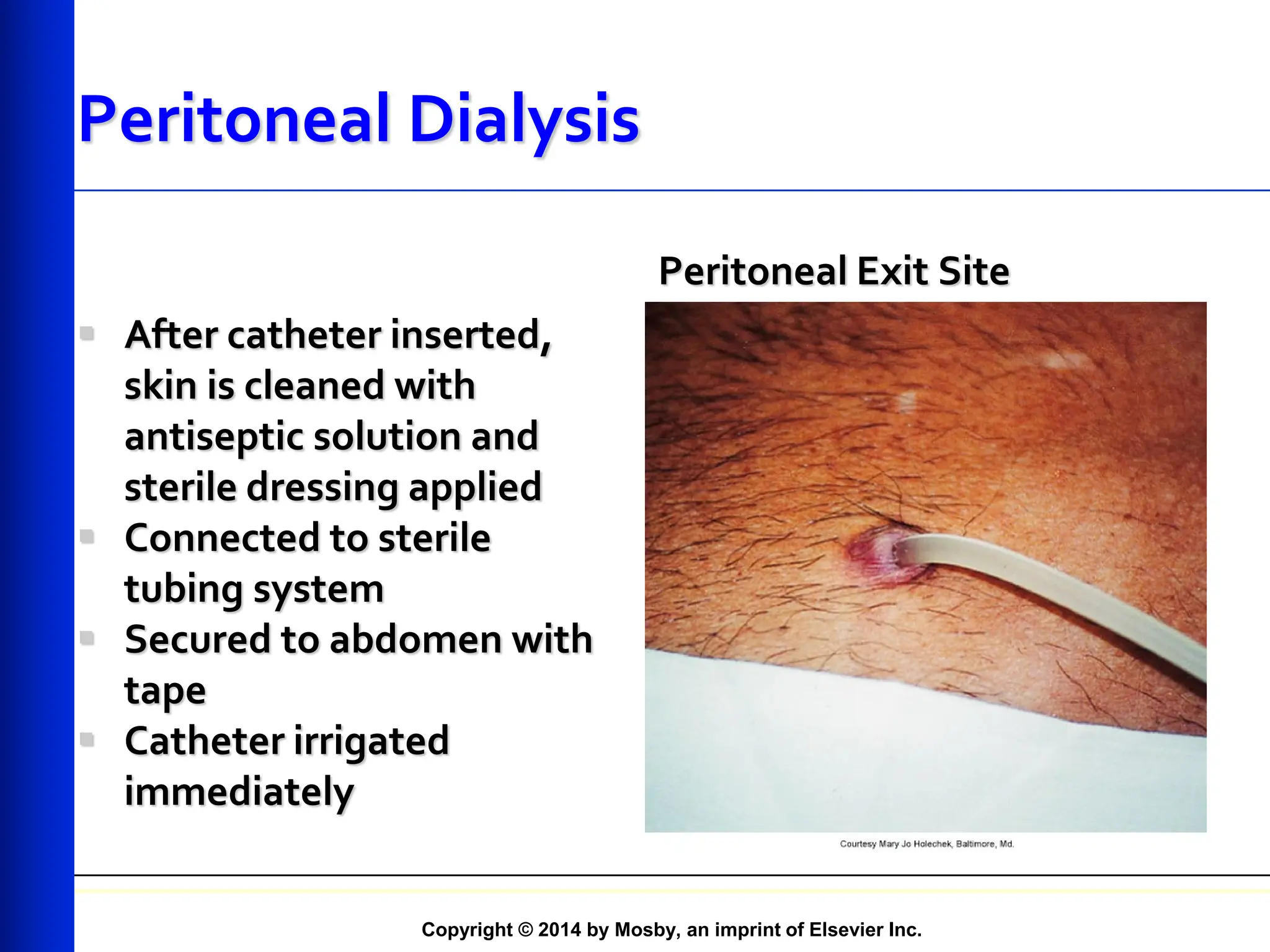
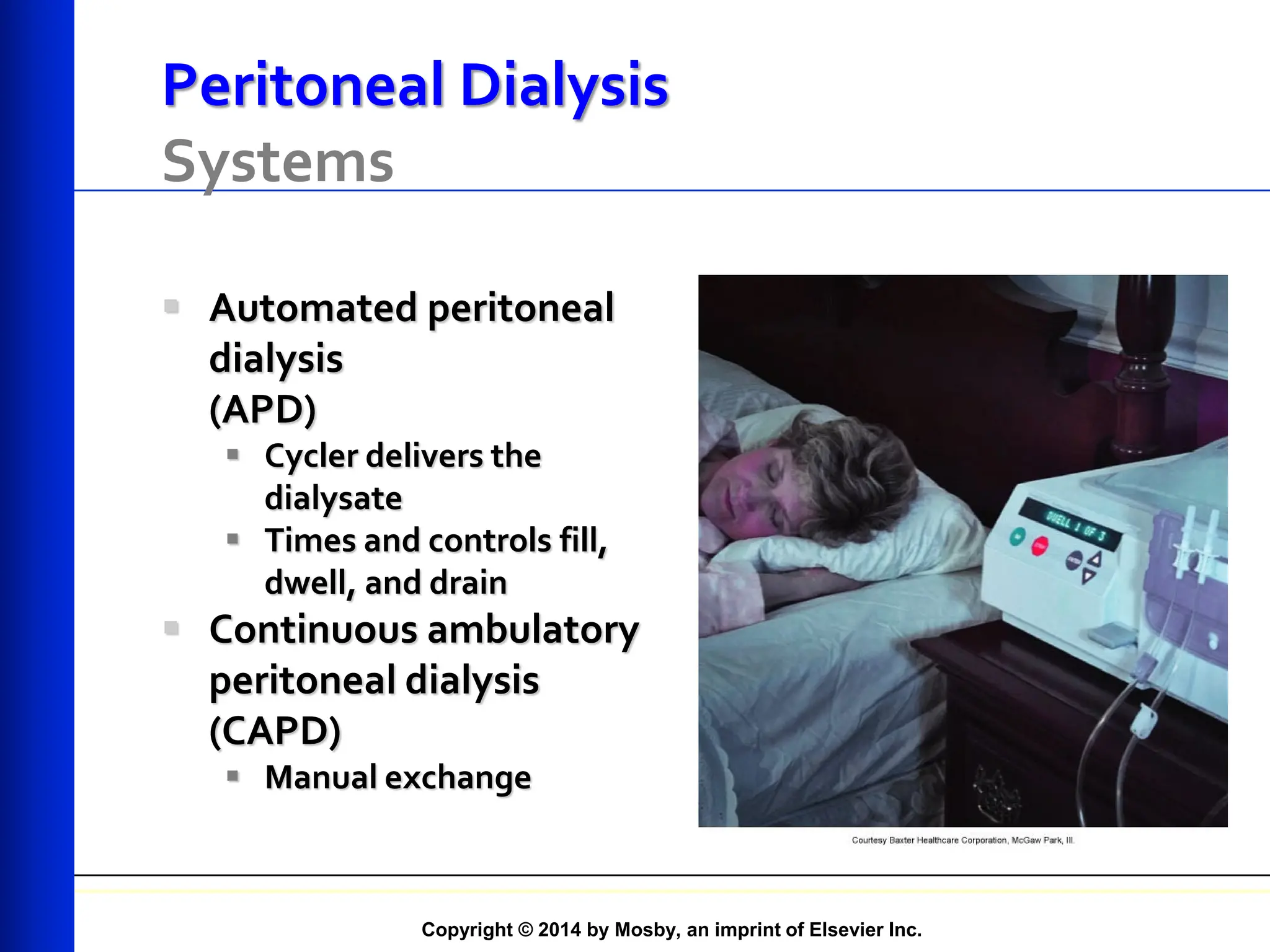
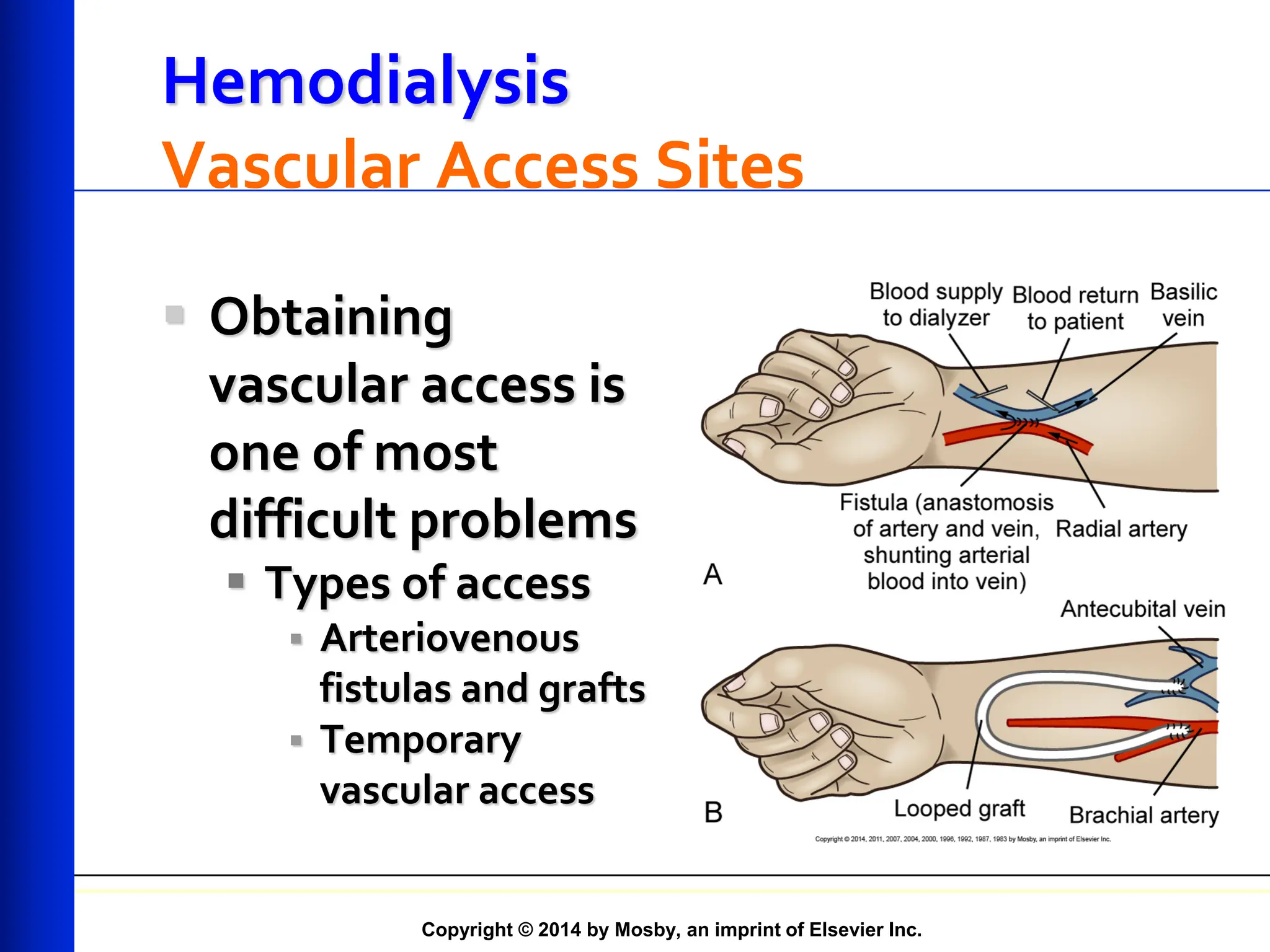
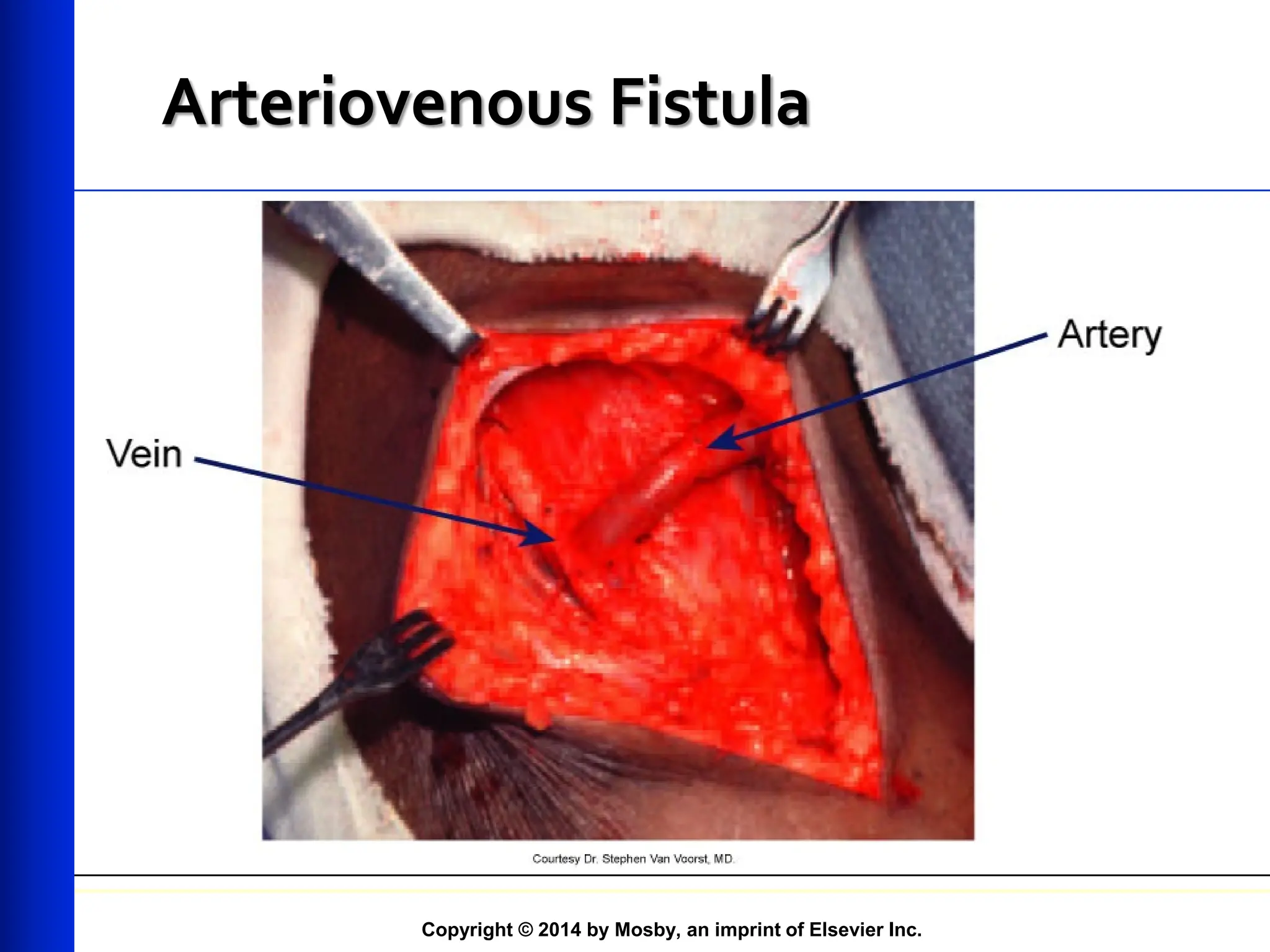
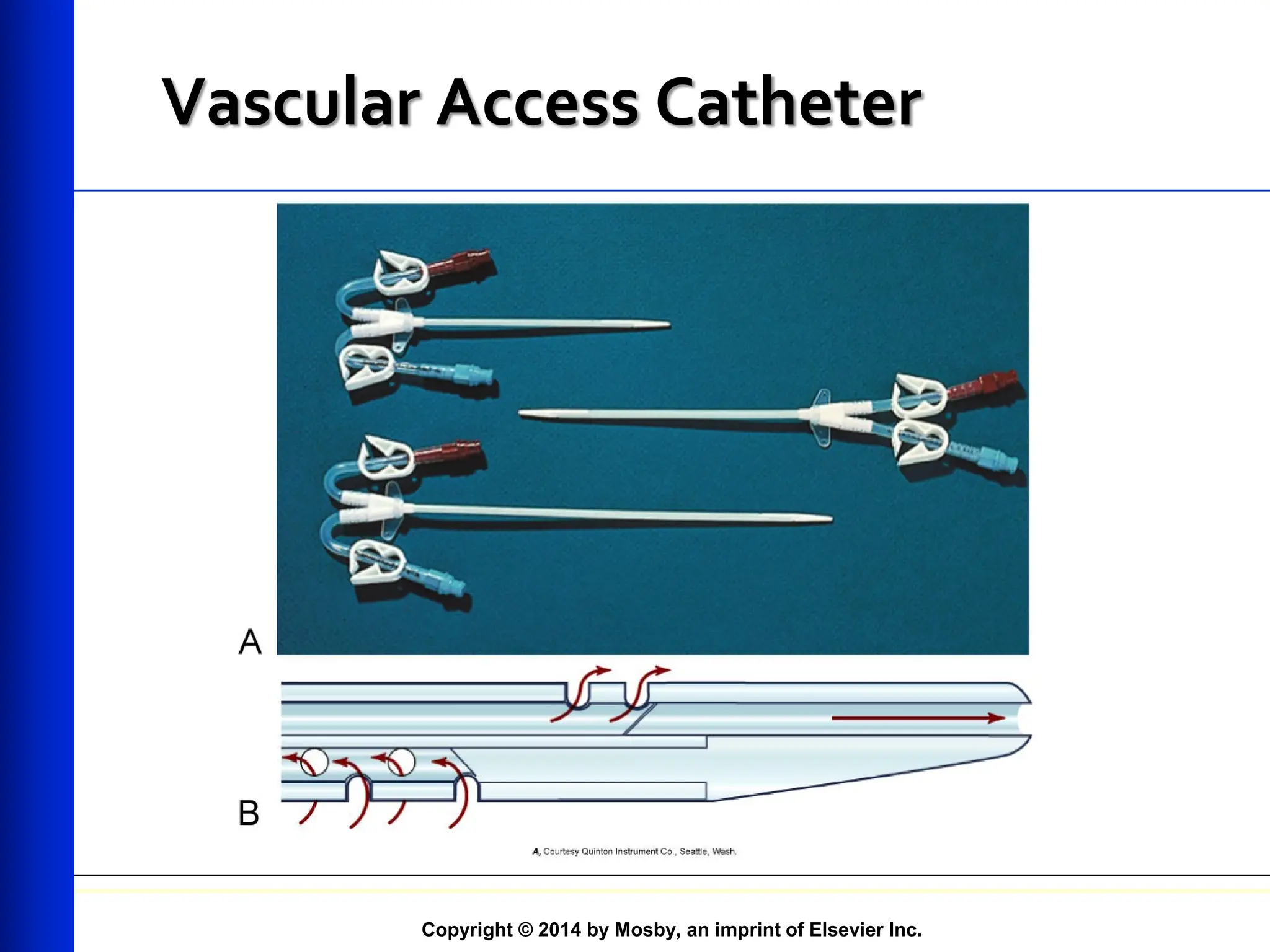
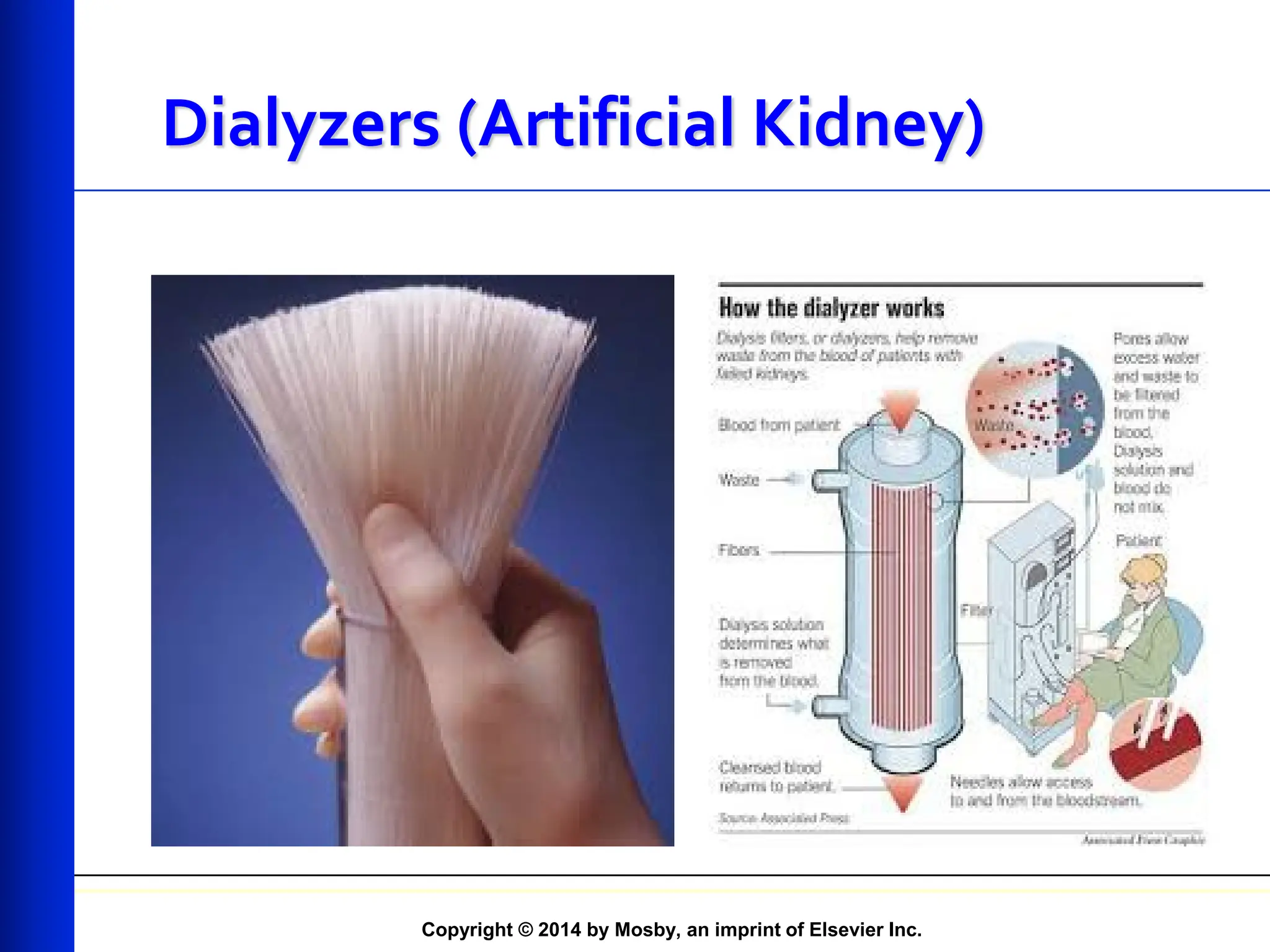
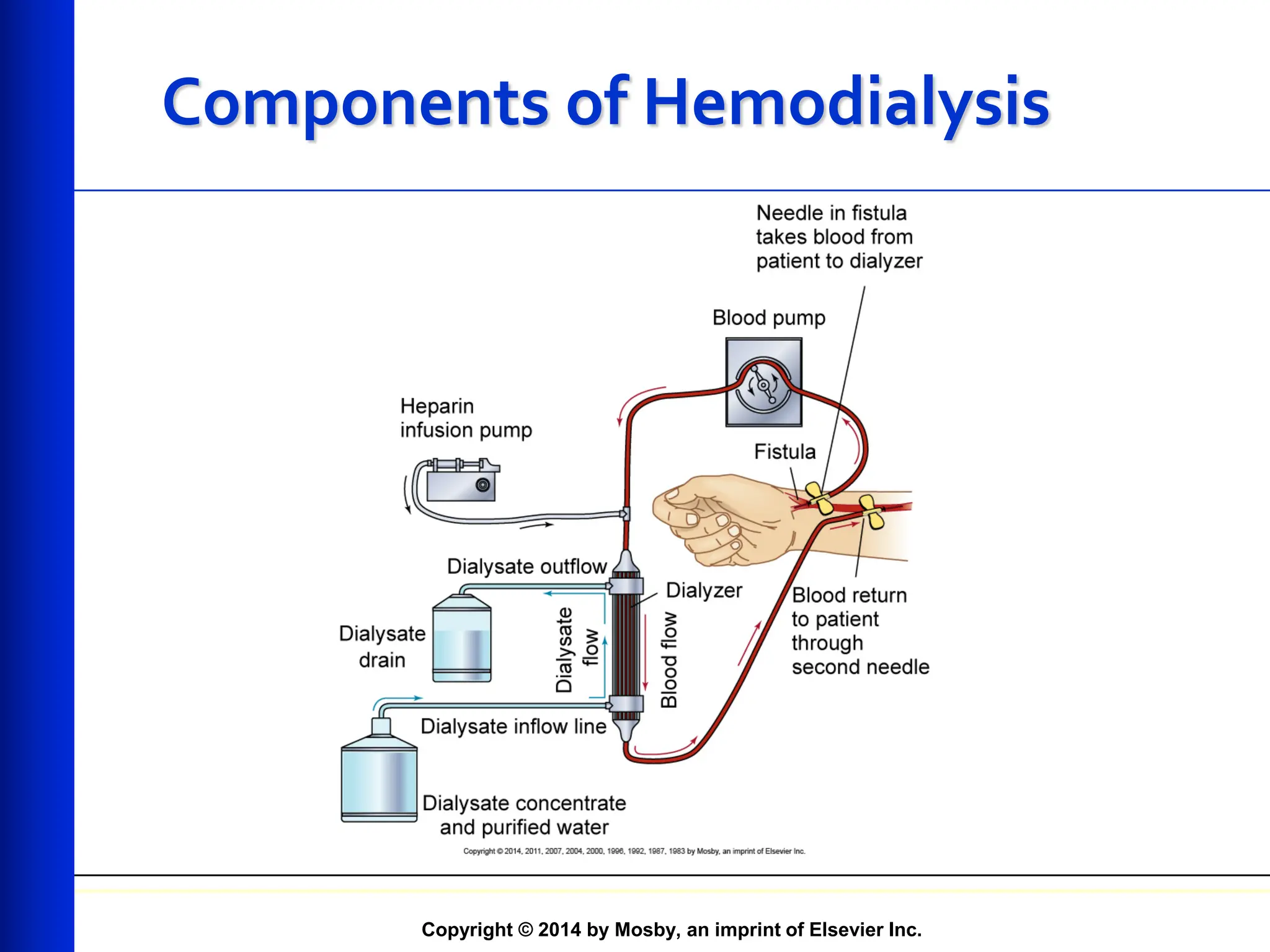
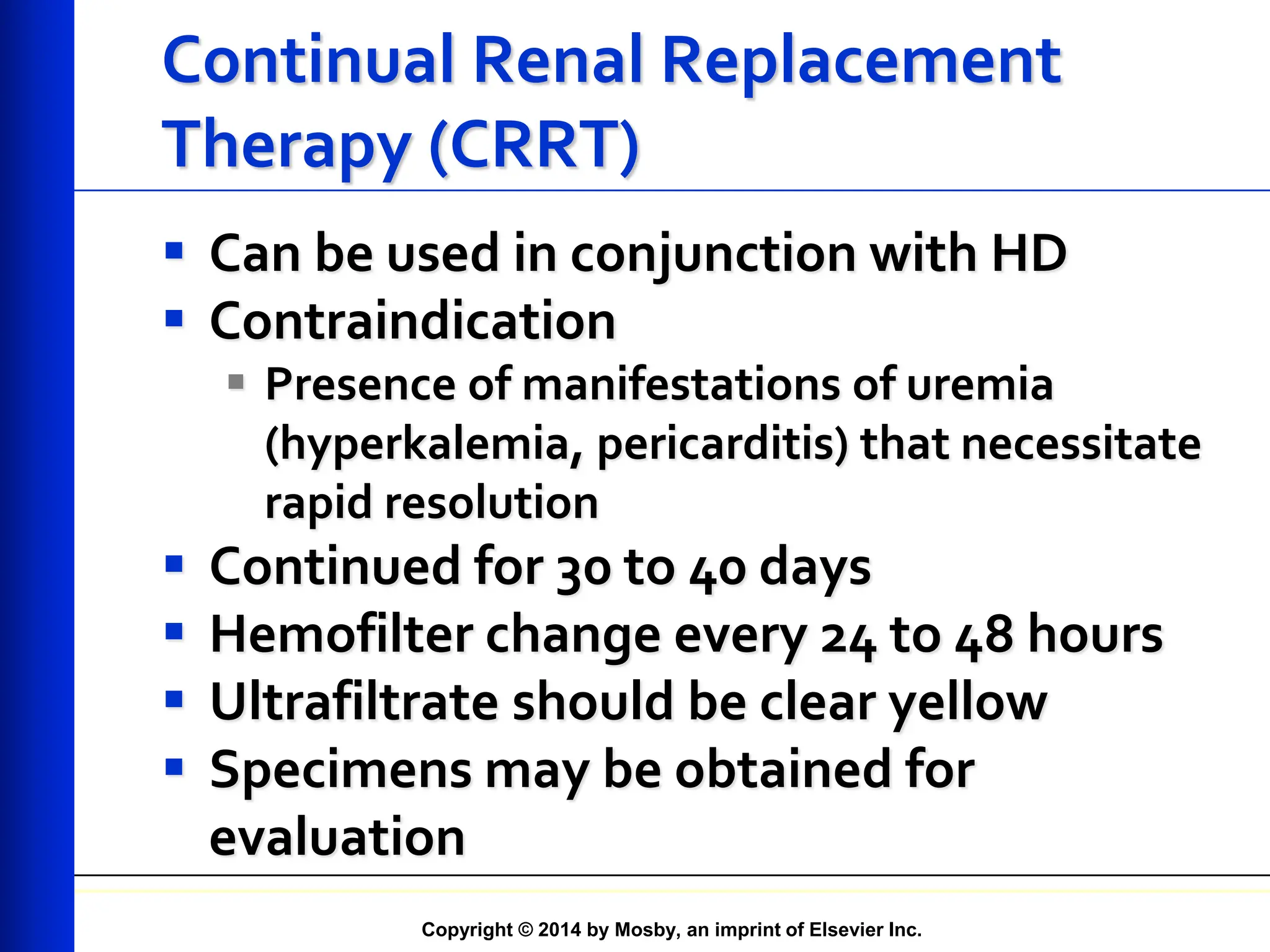
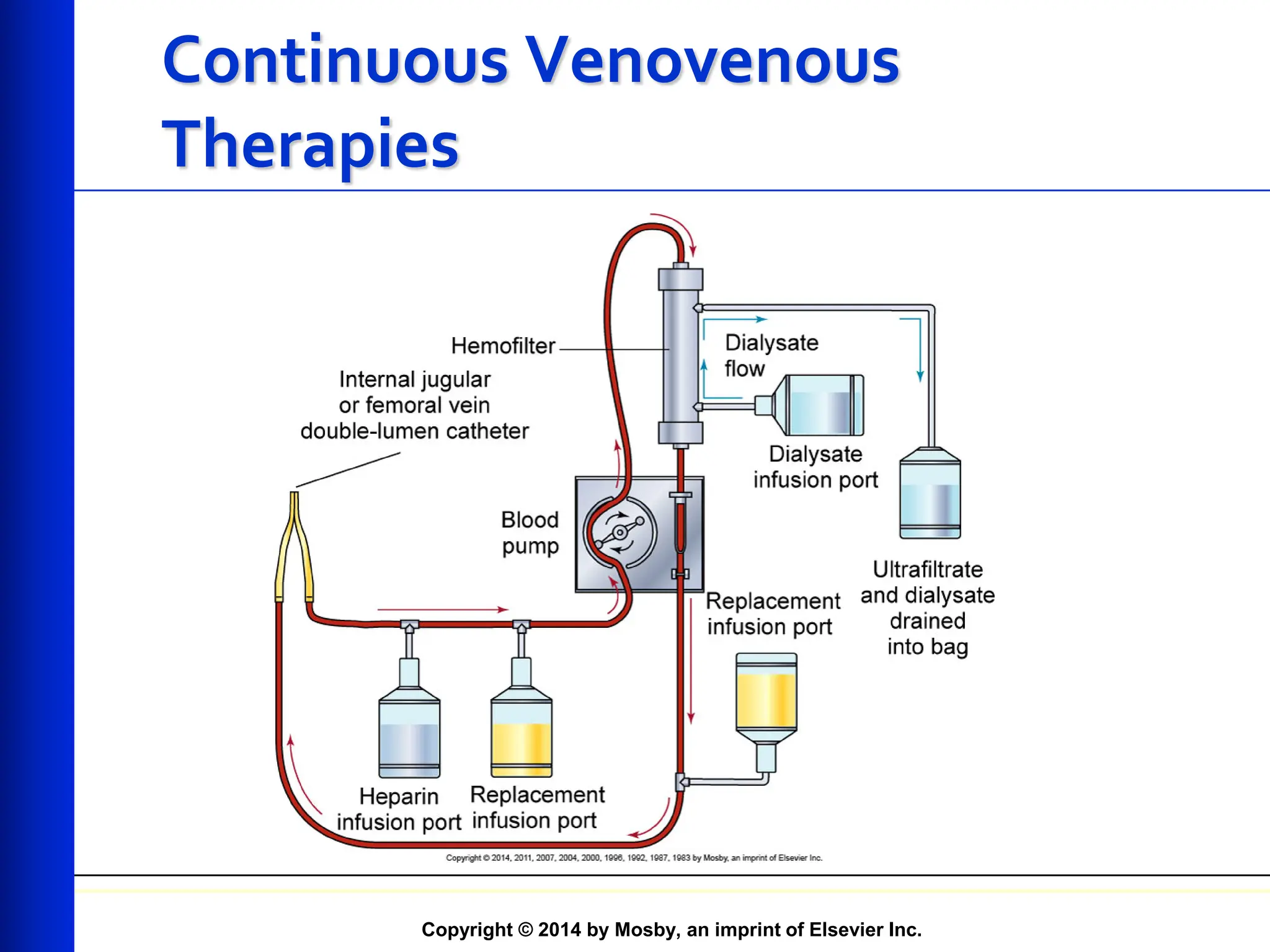
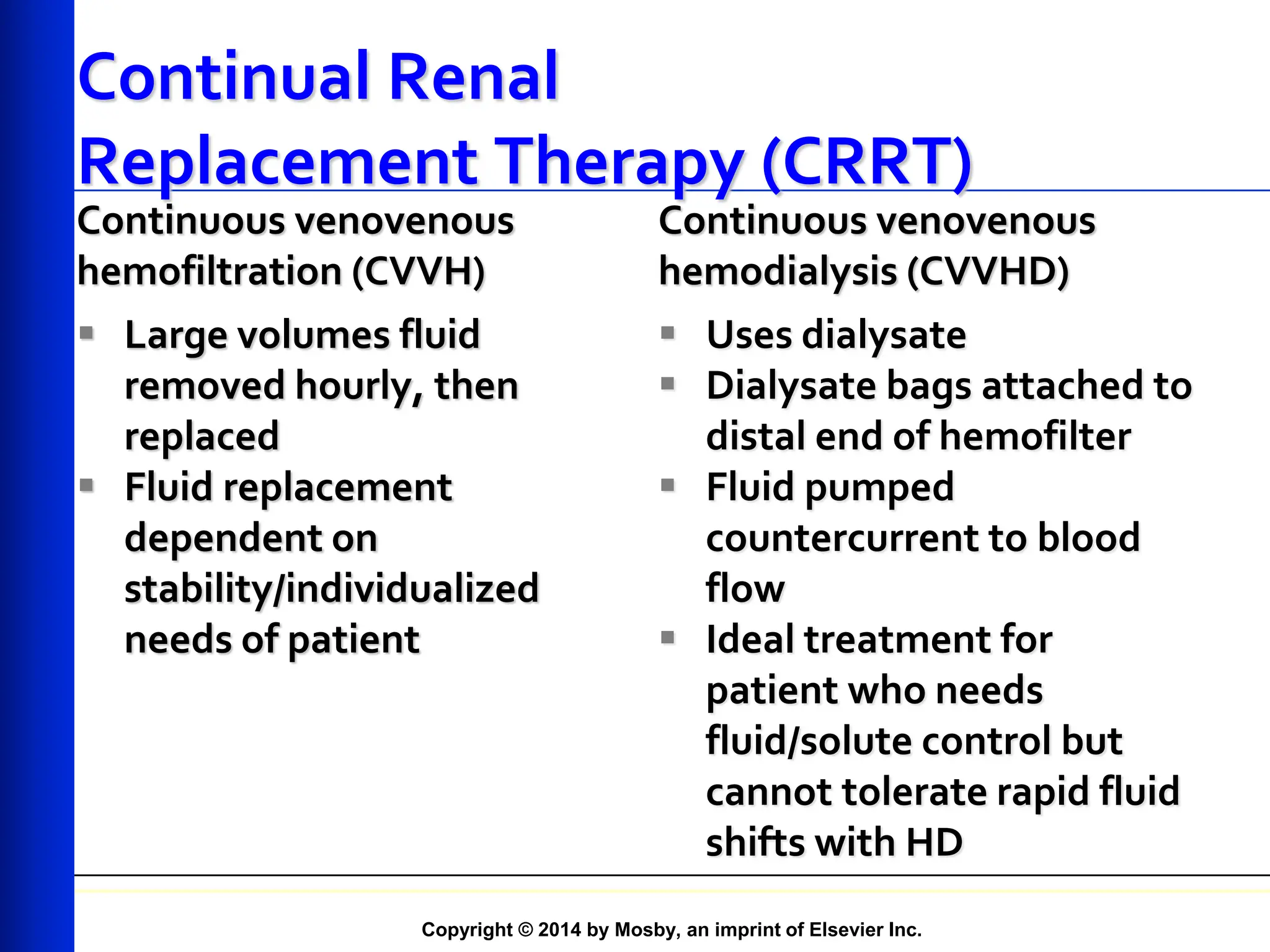
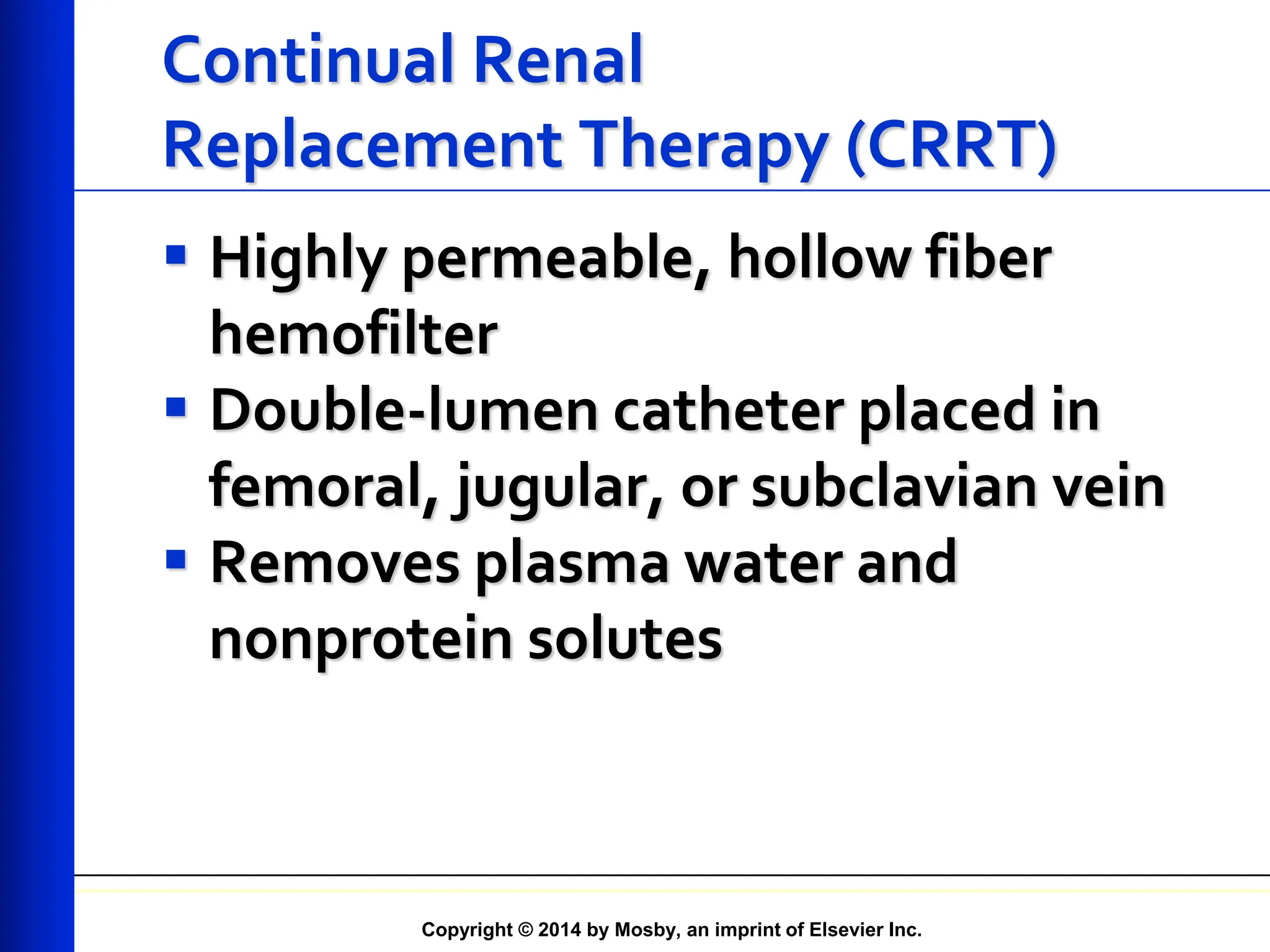
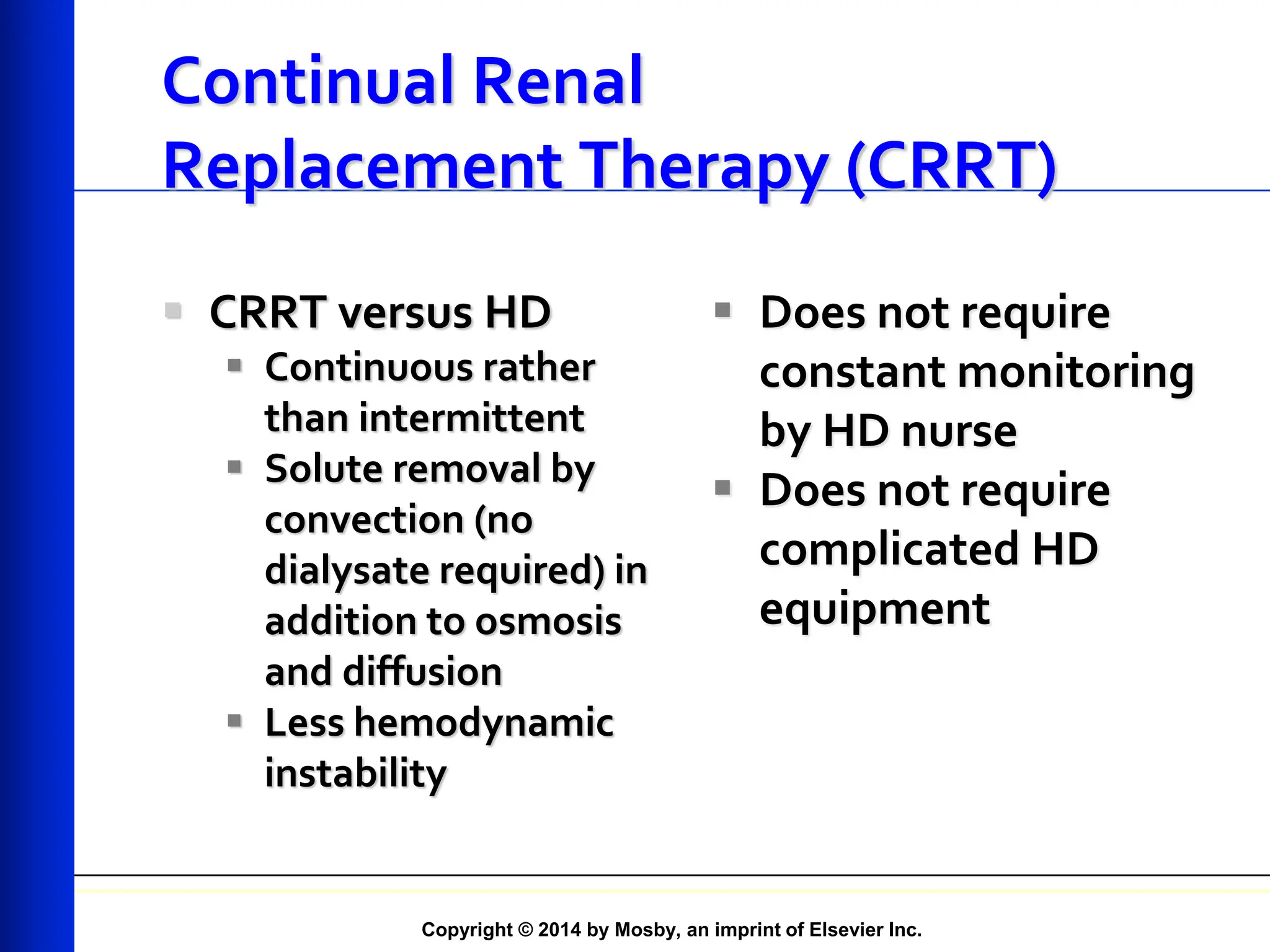
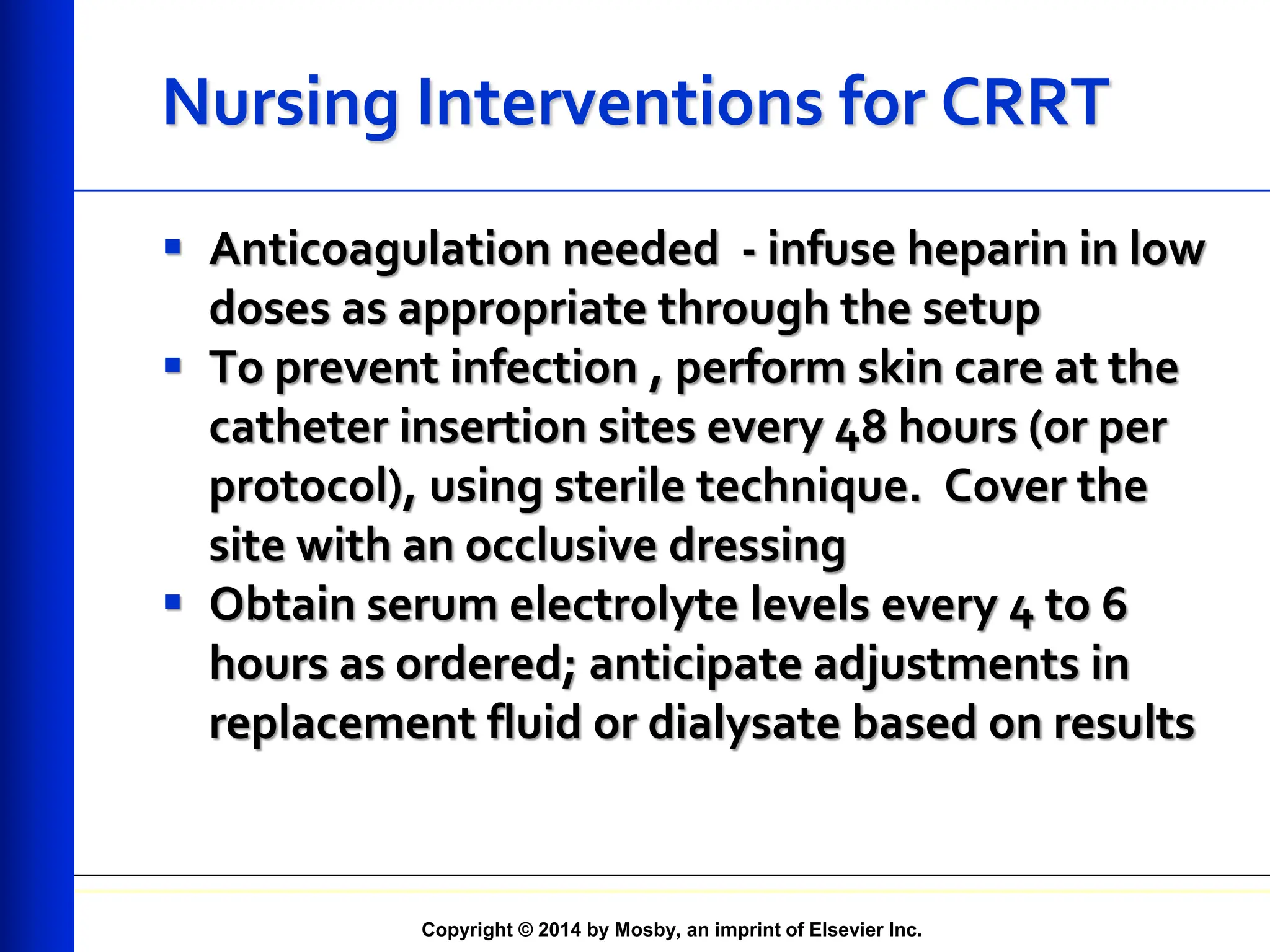
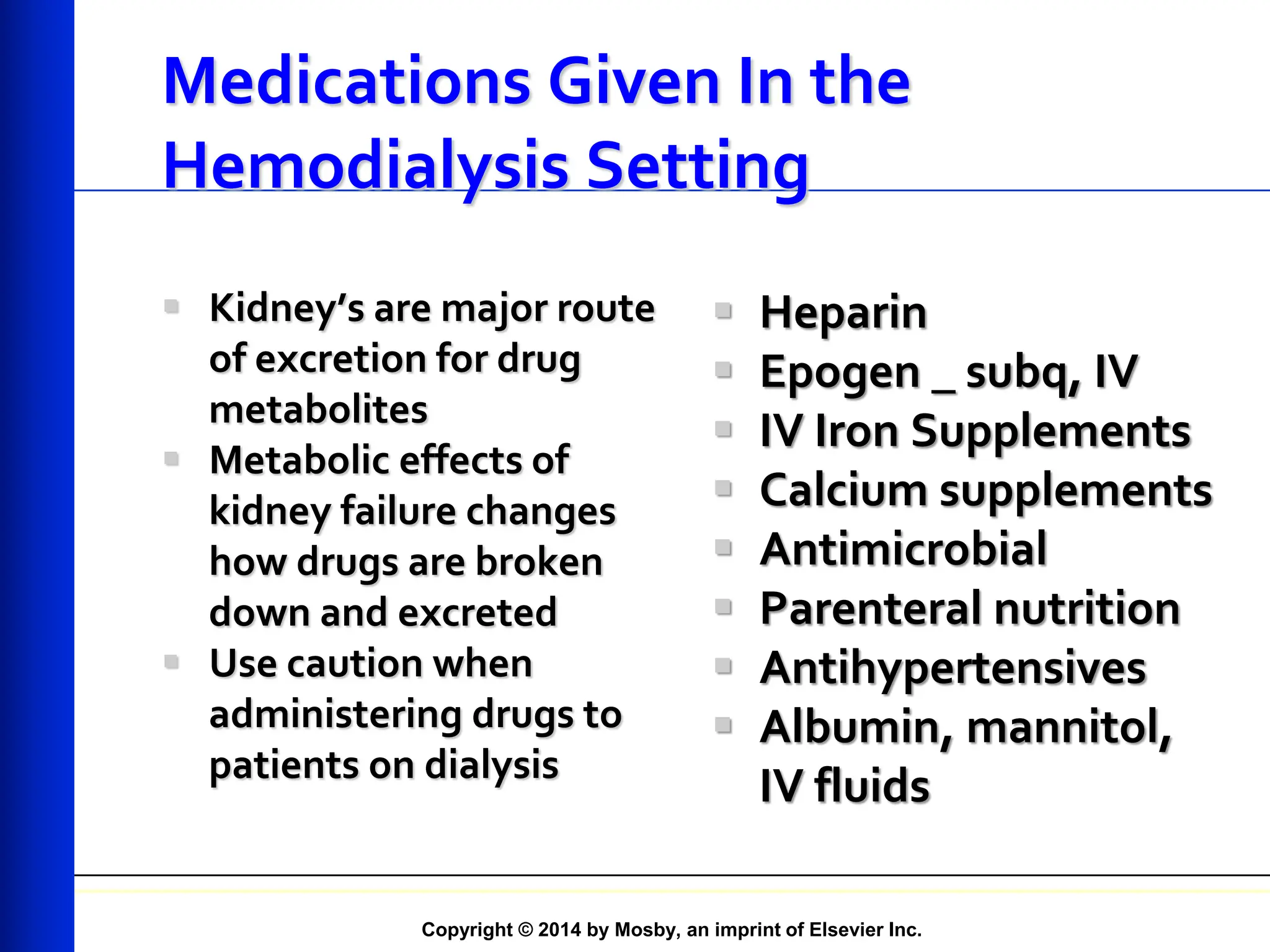
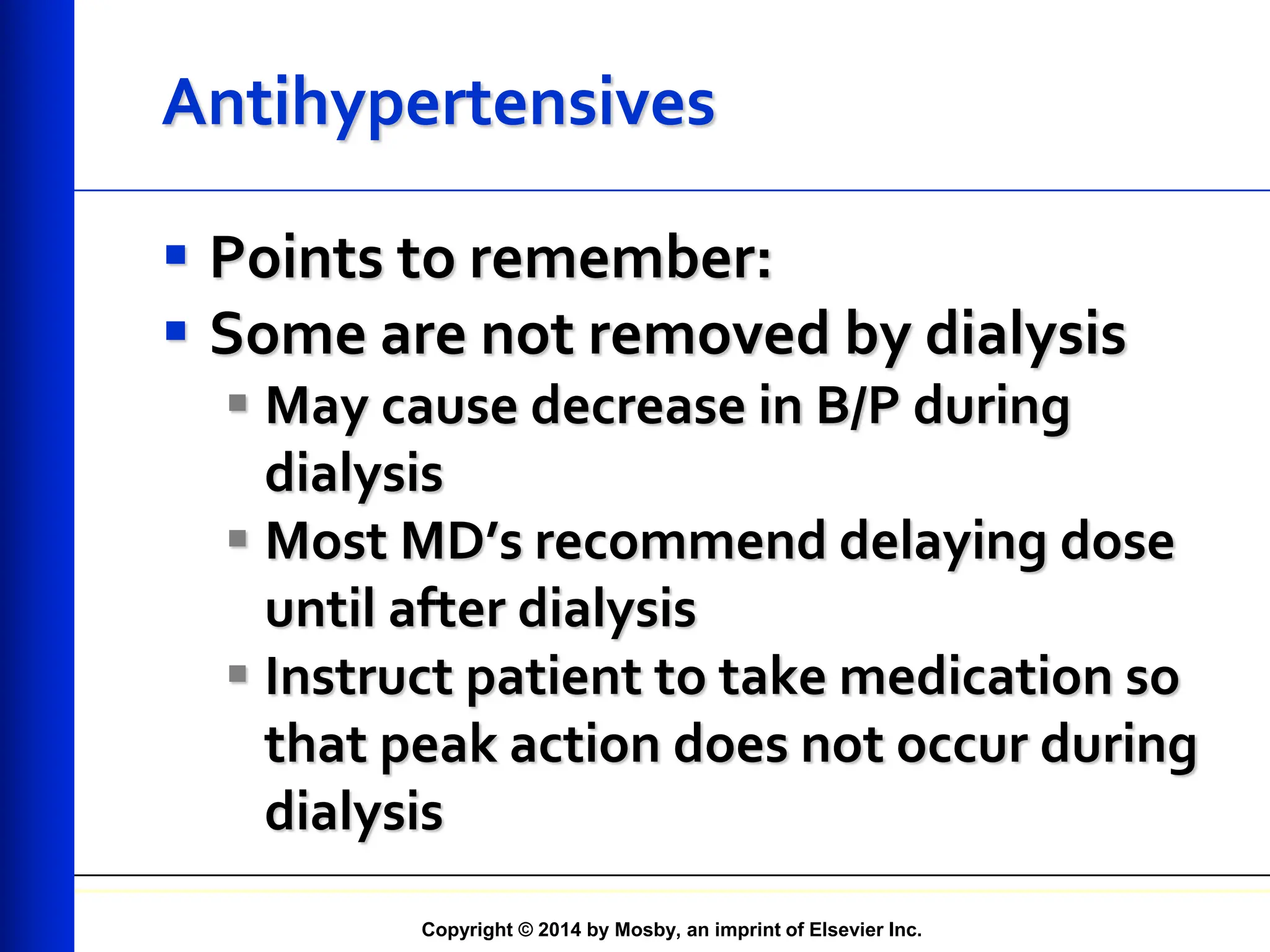
The document provides an overview of dialysis, including important lab values for monitoring patients, the types and principles of dialysis methods such as peritoneal and hemodialysis, and their respective procedures and complications. It emphasizes the significance of maintaining proper electrolyte balance and the role of dialysis in treating end-stage kidney disease (ESKD) when renal function declines. Additionally, it covers nursing interventions and considerations for medication management in dialysis settings.