This document discusses several dermatological conditions and their treatments. It covers:
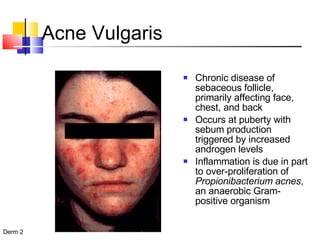
1) Acne vulgaris, its causes and treatment options including topical retinoids, benzoyl peroxide, antibiotics, and isotretinoin.
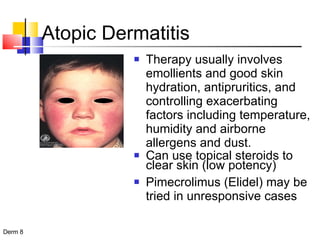
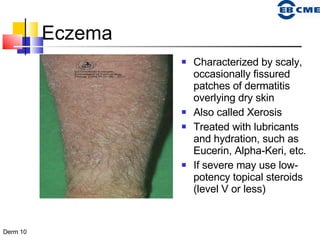
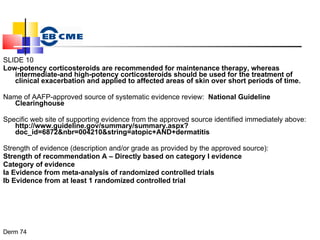
2) Atopic dermatitis/eczema, its genetic basis and treatment with emollients, topical steroids, and pimecrolimus.
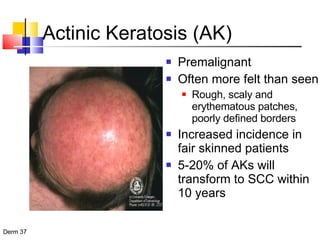
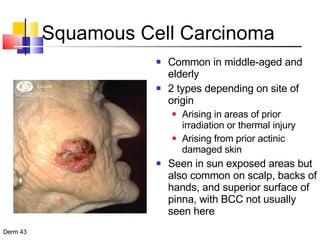
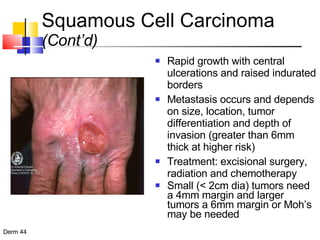
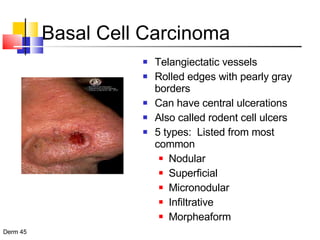
3) Common skin cancers like basal cell carcinoma and squamous cell carcinoma, their characteristics and treatments including surgery, radiation, and chemotherapy.