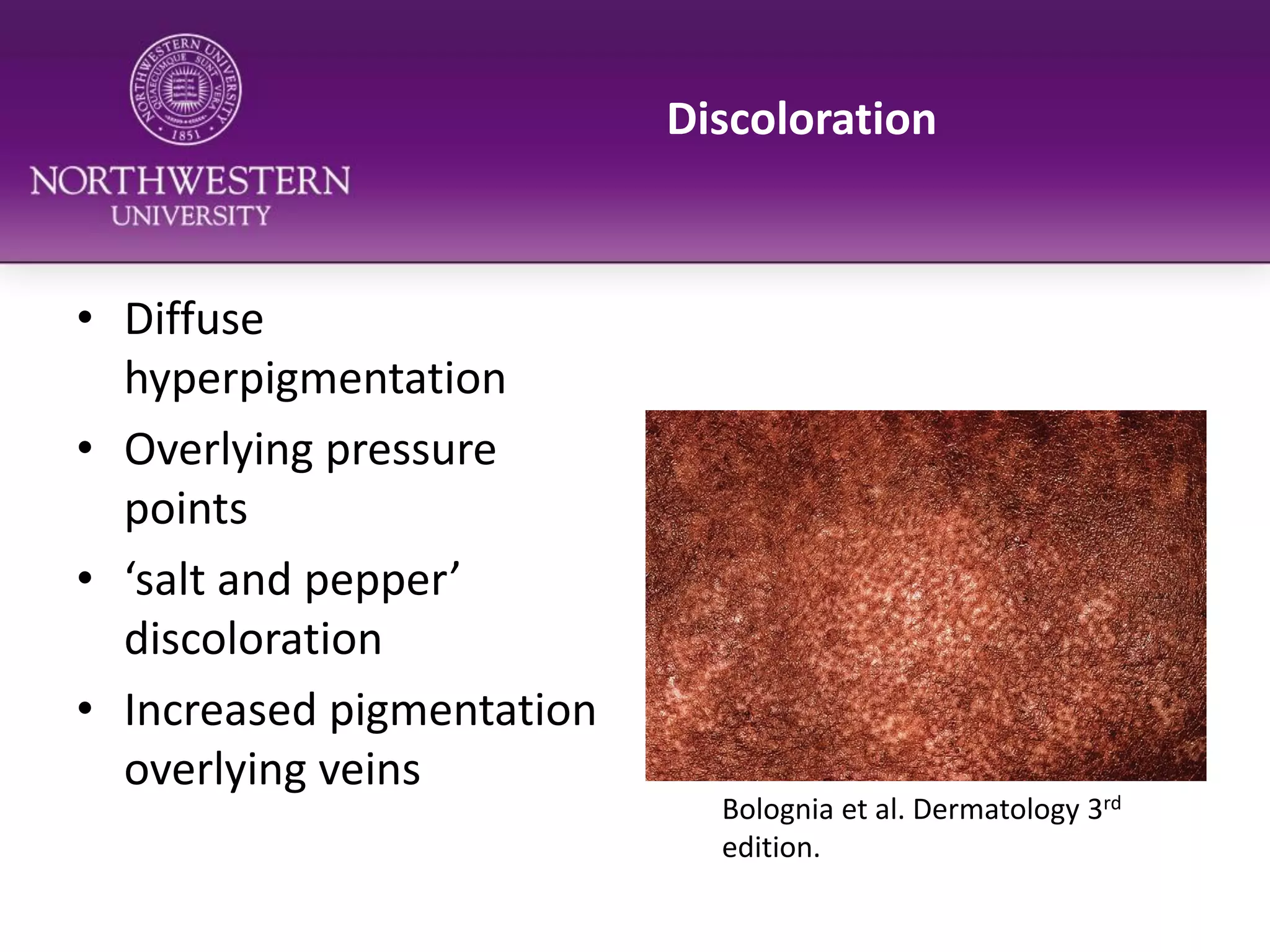
The document discusses the skin complications associated with scleroderma, focusing on conditions such as Raynaud's phenomenon, calcinosis cutis, and telangiectasia. It outlines treatment options and lifestyle modifications to manage these complications, along with the significance of gentle skin care. Additionally, it emphasizes the importance of preventative measures to avoid worsening skin conditions.