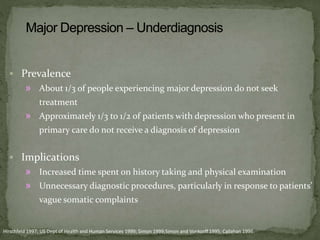
This document discusses depression, including its epidemiology, definitions, classification, diagnostic criteria, and treatment. Some key points:
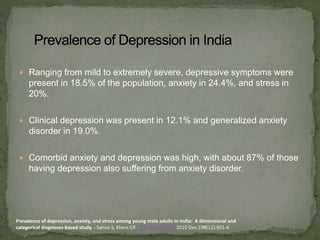
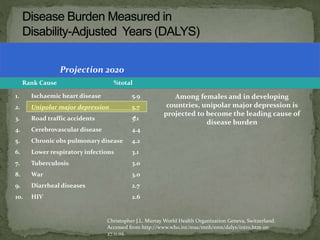
- Depression is the 3rd leading cause of disease burden worldwide and is projected to become the leading cause by 2030.
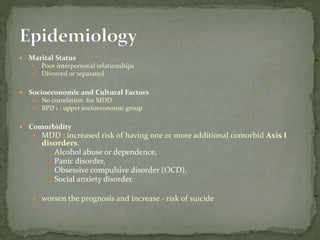
- Major depression has a prevalence of 5% and 15% of the population will experience a major depressive episode at some point in their life.
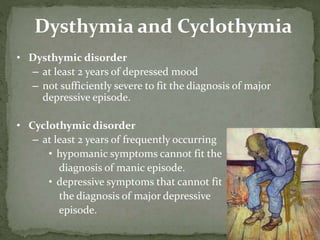
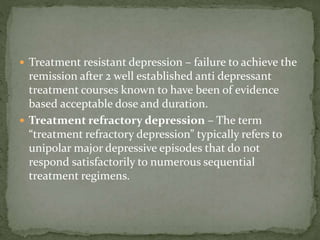
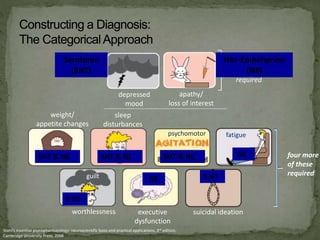
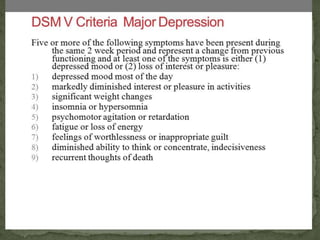
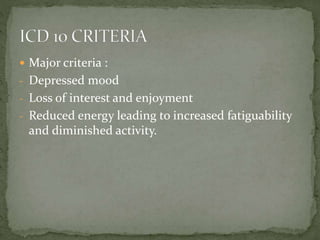
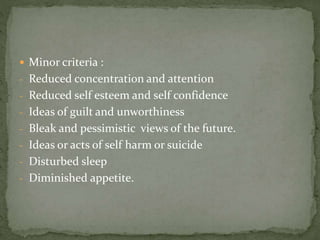
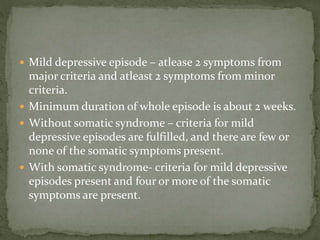
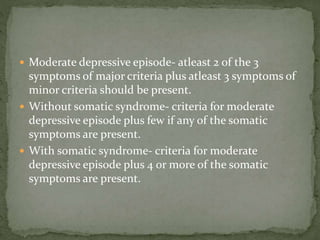
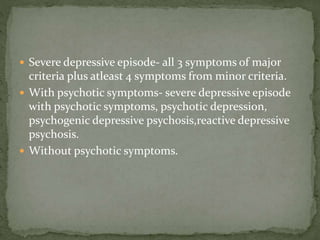
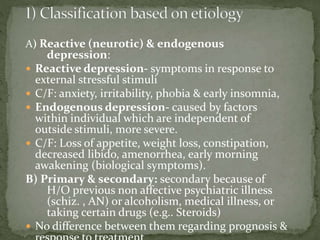
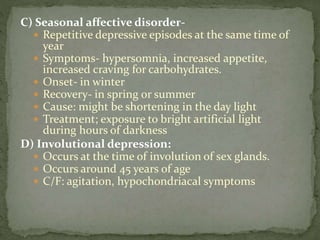
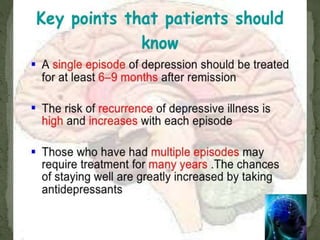
- Depression is classified based on severity from mild to severe. Diagnosis requires a certain number of symptoms from major and minor criteria groups.
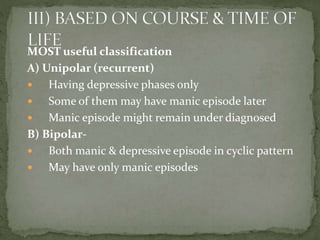
- Depression can be classified as unipolar (recurrent depression only) or bipolar (episodes of mania and depression).
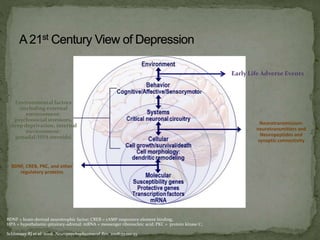
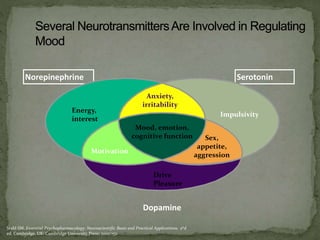
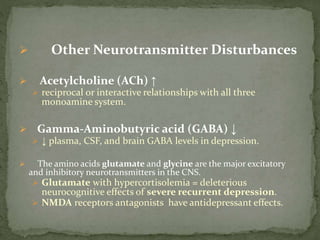
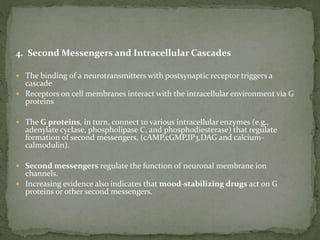
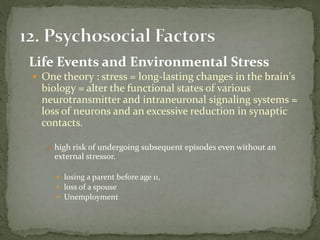
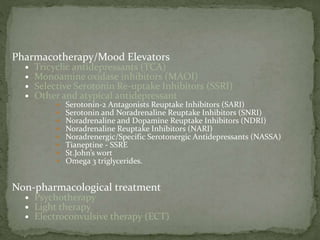
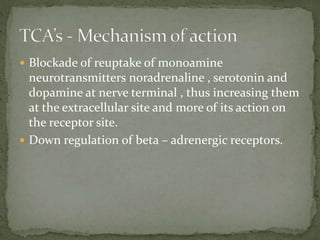
- Causes of depression involve biological factors like neurotransmitter im