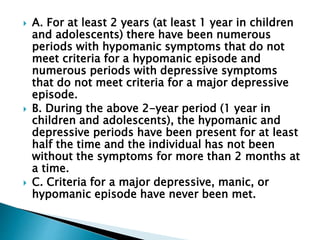
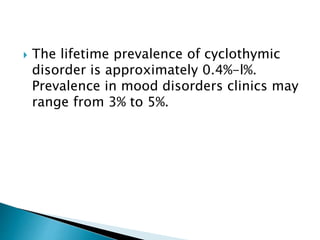
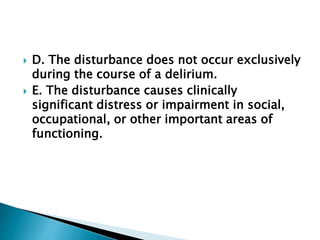
The document outlines the diagnostic criteria for cyclothymic disorder and substance/medication-induced bipolar and related disorders, emphasizing the duration and nature of mood disturbances, along with the requirement of significant distress or impairment in functioning. It provides prevalence statistics, age of onset for cyclothymic disorder in children, and specifics on the relationship between substance use and mood disturbances. Additionally, it mentions that there are no comprehensive epidemiological studies on substance-induced manic disorders and describes how the timing and nature of substance effects can influence the presentation of manic symptoms.