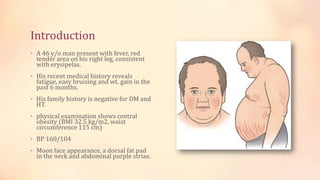
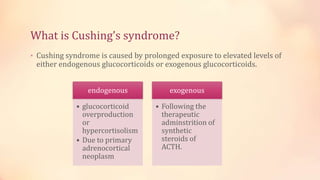
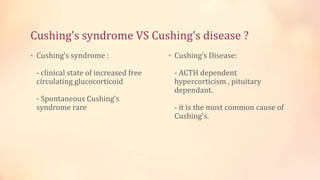
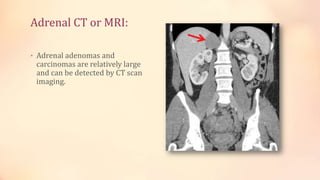
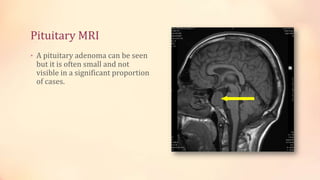
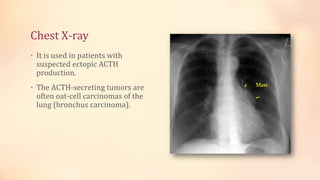
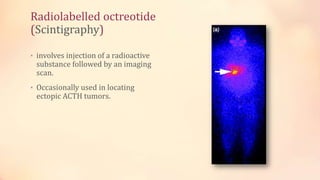
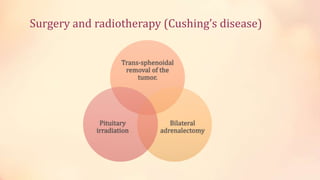
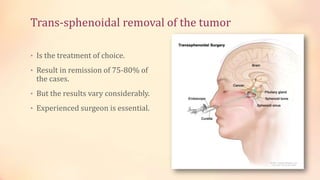
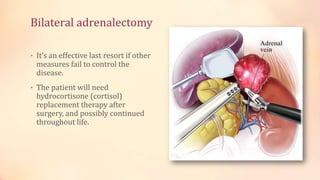
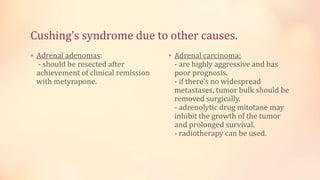
A 46-year-old man presents with signs of Cushing's syndrome, including fever, central obesity, and skin changes, alongside a background of fatigue and weight gain. Diagnostic evaluations recommend radiological investigations like adrenal CT/MRI and pituitary MRI to determine the cause and treatment options, including pharmacotherapy, surgery, and radiotherapy. Initial management involves medications like metyrapone and ketoconazole, with further treatment tailored to the specific etiology.