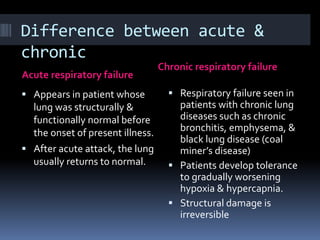
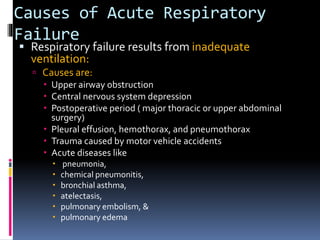
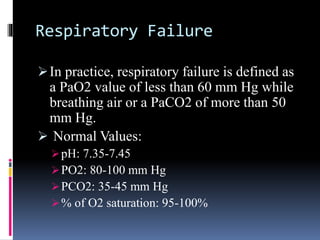
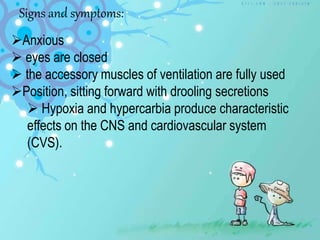
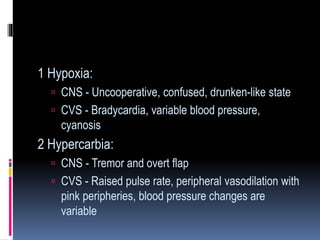
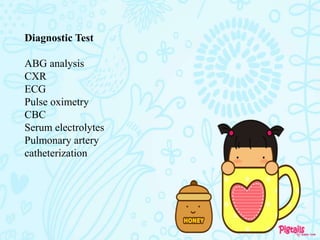
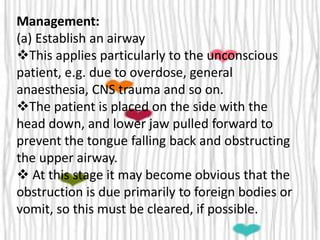
Respiratory failure occurs when the lungs cannot effectively exchange oxygen and carbon dioxide, resulting in hypoxemia (low blood oxygen) and hypercapnia (high blood carbon dioxide). Acute respiratory failure develops suddenly in patients without preexisting lung disease, while chronic respiratory failure is caused by conditions like COPD. Treatment involves oxygen therapy, ventilation if needed, treating the underlying cause, and monitoring vital signs.