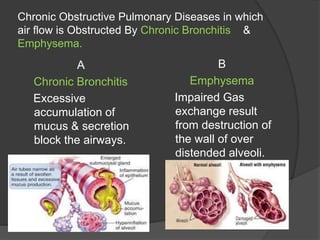
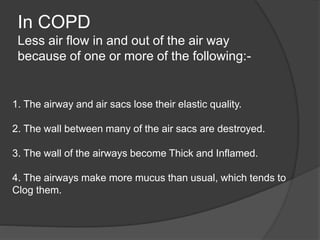
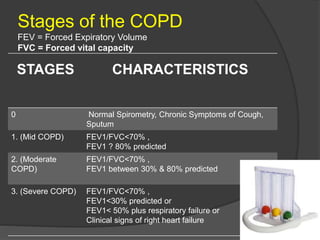
This document provides information on chronic obstructive pulmonary disease (COPD), including other names, definitions, causes, risk factors, stages, symptoms, diagnostic tests, complications, treatment options, nursing assessments, and lifestyle management strategies. COPD is a chronic inflammatory lung disease characterized by obstructed airflow. It involves chronic bronchitis and emphysema and is caused primarily by cigarette smoking. Symptoms include cough, sputum production, shortness of breath, and wheezing. Treatment focuses on reducing symptoms and preventing further lung damage through the use of bronchodilators, anti-inflammatory drugs, oxygen therapy, pulmonary rehabilitation, and smoking cessation.








![1. Norcotine Replacement Therapies:-
* Withdrawal from nicotine may cause have Unpleasant side
effects (1week) such as Anxiety, Irritability, Difficulty
concentrating, Anger , Fatigue, Drowsiness, Depression, Sleep
disturption.
* Nicotine Polacrilex is a chewing gum. {2mg,4mg}
smoking [1 pack/day] = 4mg
smoking [less than 1 pack/day] = 2mg
gradually reduce the amount chewed over the 3 next months.
*](https://image.slidesharecdn.com/copd-221016173611-f1c13d3b/85/Presentation-COPD-pptx-14-320.jpg)










