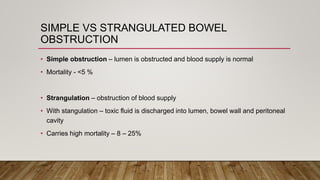
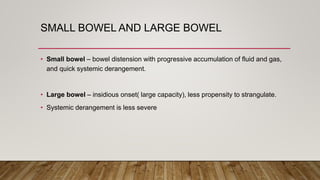
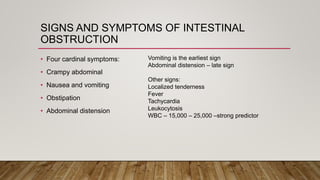
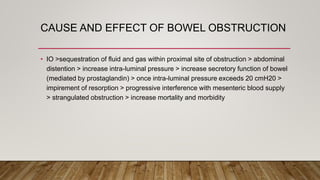
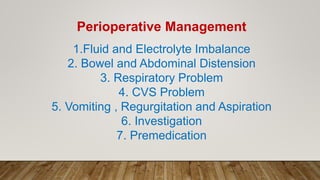
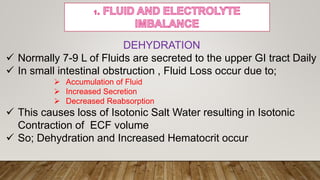
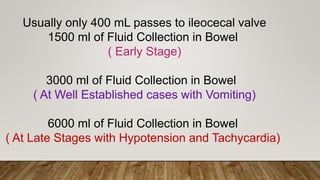
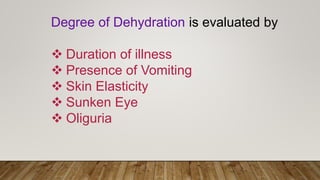
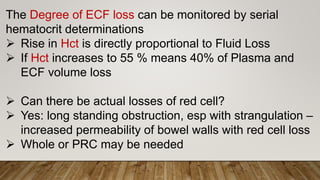
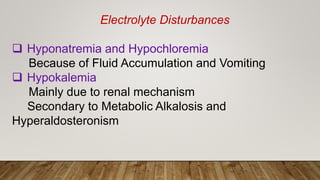
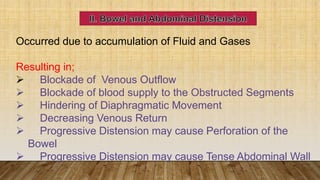
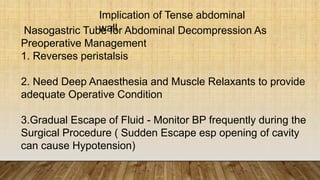
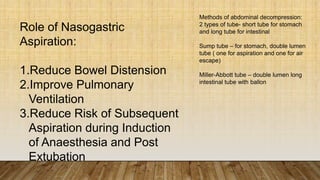
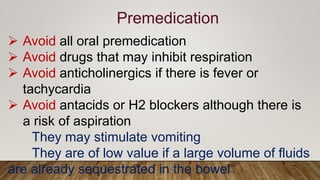
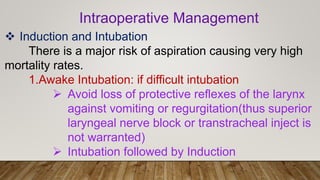
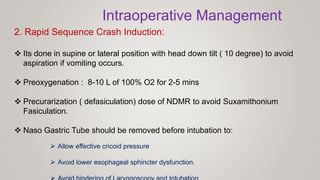
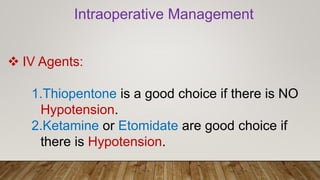
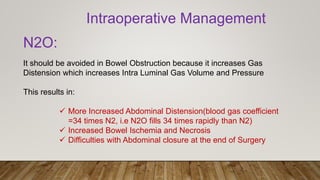
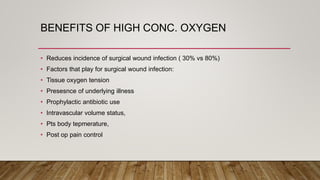
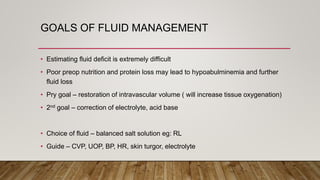
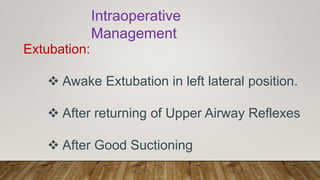
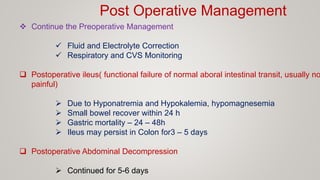
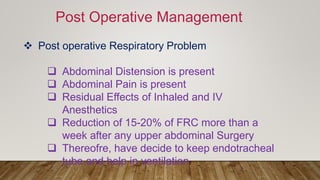
The document discusses anaesthesia management for intestinal obstruction, distinguishing between simple and strangulated bowel obstructions, the symptoms, and the associated risks of mortality. It outlines the perioperative management of fluid and electrolyte imbalances, respiratory issues, and the importance of careful monitoring during induction and extubation. Additionally, it emphasizes the need for both preoperative and postoperative care to mitigate complications, including managing abdominal distension and ensuring effective ventilation.