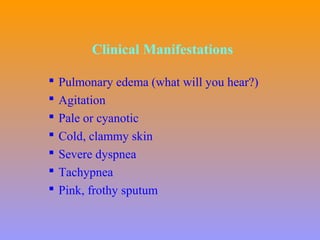
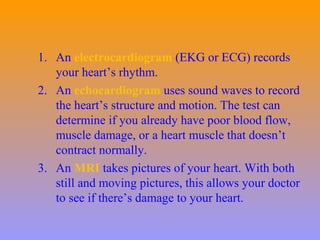
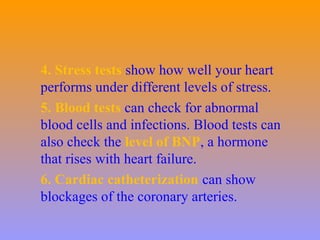
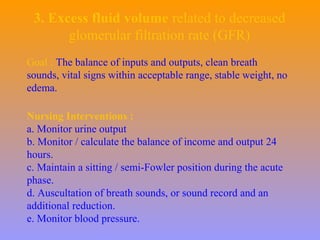
Congestive heart failure (CHF) refers to the stage where fluid builds up around the heart due to weakening of the heart muscles. It can be caused by conditions like high blood pressure, heart attack, and valve disorders. Symptoms include fatigue, shortness of breath, swelling, and weight changes. Diagnostic tests include EKGs, echocardiograms, stress tests, and blood tests. Treatment involves medications to open blood vessels, slow the heart rate, and reduce fluids, as well as potential surgeries like angioplasty or valve repair. Nursing focuses on monitoring cardiac output, managing activity levels and fluids.