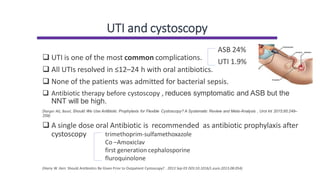
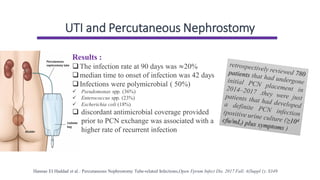
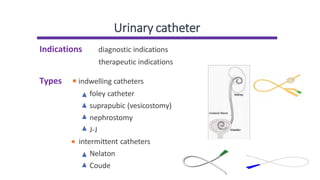
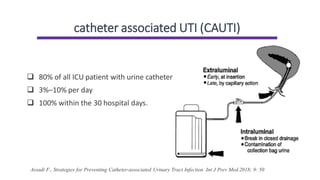
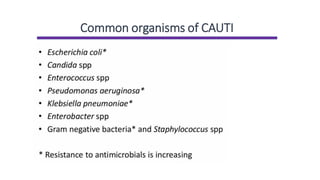
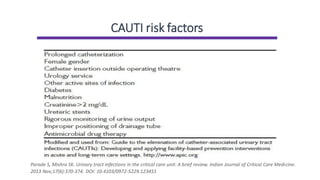
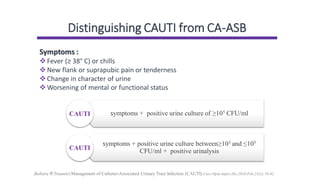
Urinary catheters can lead to complicated UTIs. CAUTIs occur in 3-10% of ICU patients per day and almost all by 30 days. Common organisms include Pseudomonas, Enterococcus, and E. coli. Risk factors include improper handwashing and maintenance. Symptoms with positive urine culture indicate CAUTI. Treatment involves removing the catheter, obtaining a urine sample, and starting antibiotics. Proper hand hygiene and following maintenance procedures can prevent CAUTIs. Antibiotics before procedures like cystoscopy may reduce UTIs but have a high number needed to treat. Vesicostomy and nephrostomy can also lead to UTIs, which are usually treated with oral antibiotics.
![Managing CAUTI
Urinary tract infection (catheter-associated): antimicrobial prescribing
NICE guideline [NG113] Published: 23 November 2018
Be aware :
❑ Give advice about managing symptoms with self-care
❑ Antibiotic treatment is not routinely needed for asymptomatic
bacteriuria in child with a catheter
❑ CAUTI is a symptomatic infection](https://image.slidesharecdn.com/complicateduti-1-211021170007/85/Complicated-uti-6-320.jpg)
![CAUTI treatment
Urinary tract infection (catheter-associated): antimicrobial prescribing
NICE guideline [NG113] Published: 23 November 2018
❑removing or changing the catheter as soon as possible
❑obtain a urine sample before antibiotics are taken
❑start antibiotic therapy
❑Reassess the child after 48 hr.](https://image.slidesharecdn.com/complicateduti-1-211021170007/85/Complicated-uti-8-320.jpg)
![CAUTI antibiotic therapy
Urinary tract infection (catheter-associated): antimicrobial prescribing
NICE guideline [NG113] Published: 23 November 2018](https://image.slidesharecdn.com/complicateduti-1-211021170007/85/Complicated-uti-9-320.jpg)