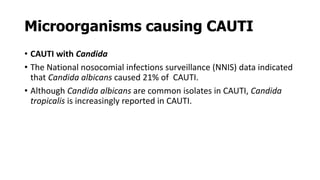
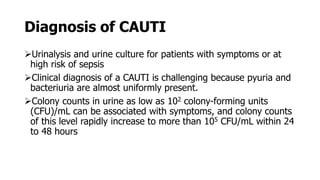
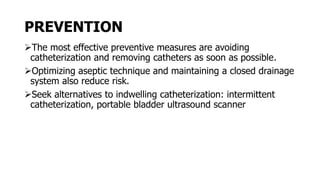
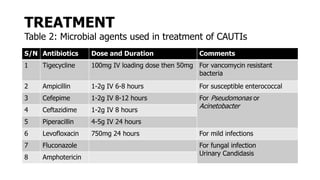
Catheter-associated urinary tract infections (CAUTI) are the most common healthcare-associated infection. Escherichia coli is the primary cause, though other bacteria like Proteus mirabilis and Pseudomonas aeruginosa can also cause CAUTI. Risk factors include the duration of catheterization and non-adherence to aseptic technique during insertion and care. Symptoms can range from urinary issues to more systemic signs. Diagnosis involves urinalysis and culture, with over 102 CFU/mL indicating infection. Prevention focuses on limiting unnecessary catheter use and optimizing aseptic practices, while treatment involves antibiotics targeted to the identified bacteria.