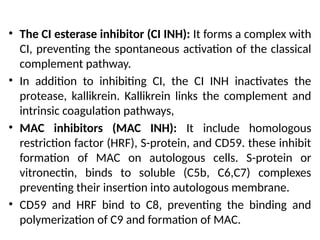
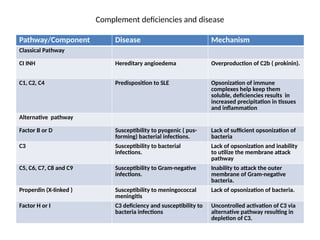
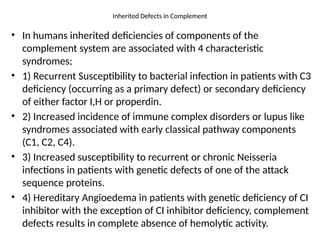
The document discusses the complement system, comprising serum and membrane-bound proteins essential for both acquired and natural immune defense, detailing its activation pathways (classical and alternative) and regulatory mechanisms. It highlights the roles of various complement proteins, their influence on inflammation, opsonization, and cell lysis, as well as the impact of complement deficiencies on susceptibility to infections and immune disorders. Additionally, it addresses hereditary angioedema and other syndromes associated with genetic defects in complement components.