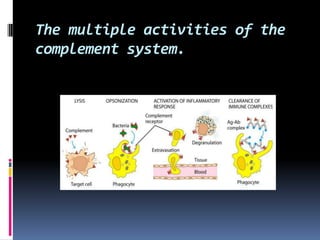
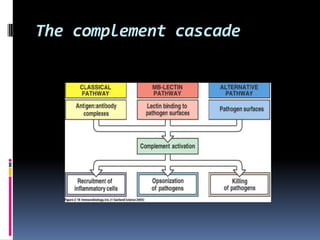
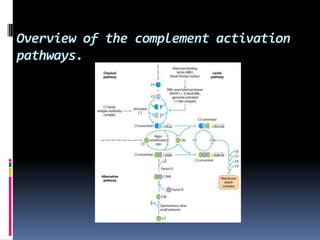
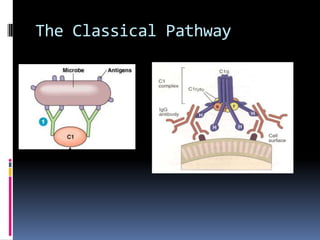
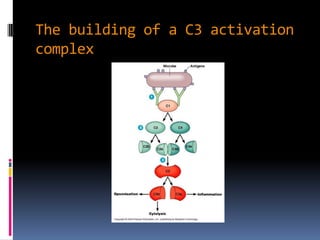
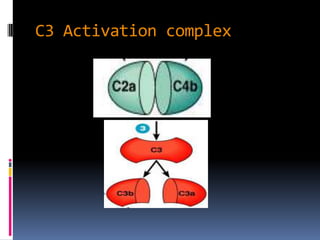
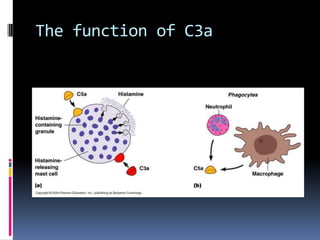
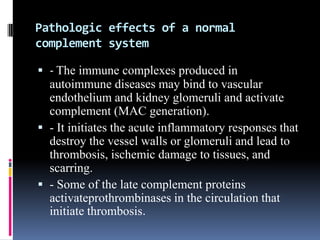
1) The document discusses the complement cascade and its three activation pathways: the classical, lectin, and alternative pathways. It also discusses complement deficiency diseases.
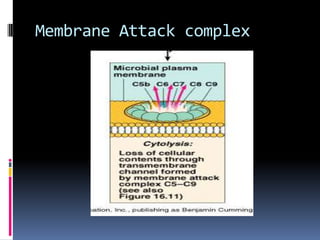
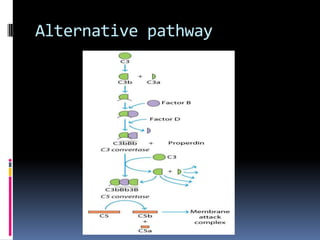
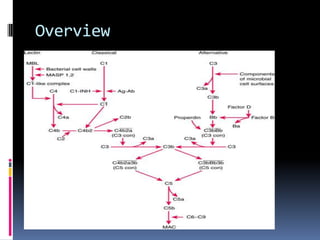
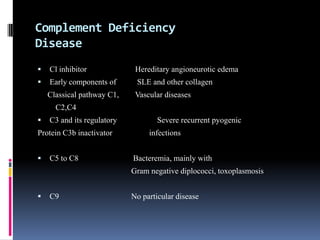
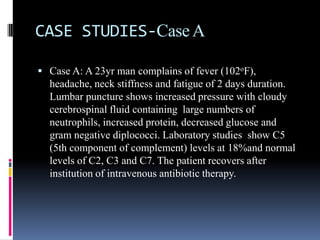
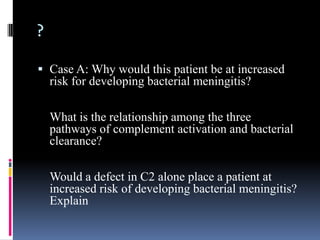
2) Case A is about a man with meningitis whose lab results show low C5 levels. Low C5 would impair the membrane attack complex and increase risk of infection.
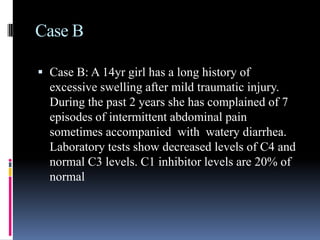
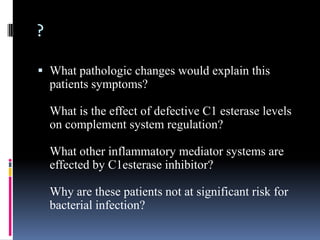
3) Case B is about a girl with swelling and abdominal pain whose labs show low C4 and C1 inhibitor. Low C1 inhibitor causes hereditary angioedema by impairing complement regulation and the kinin system.