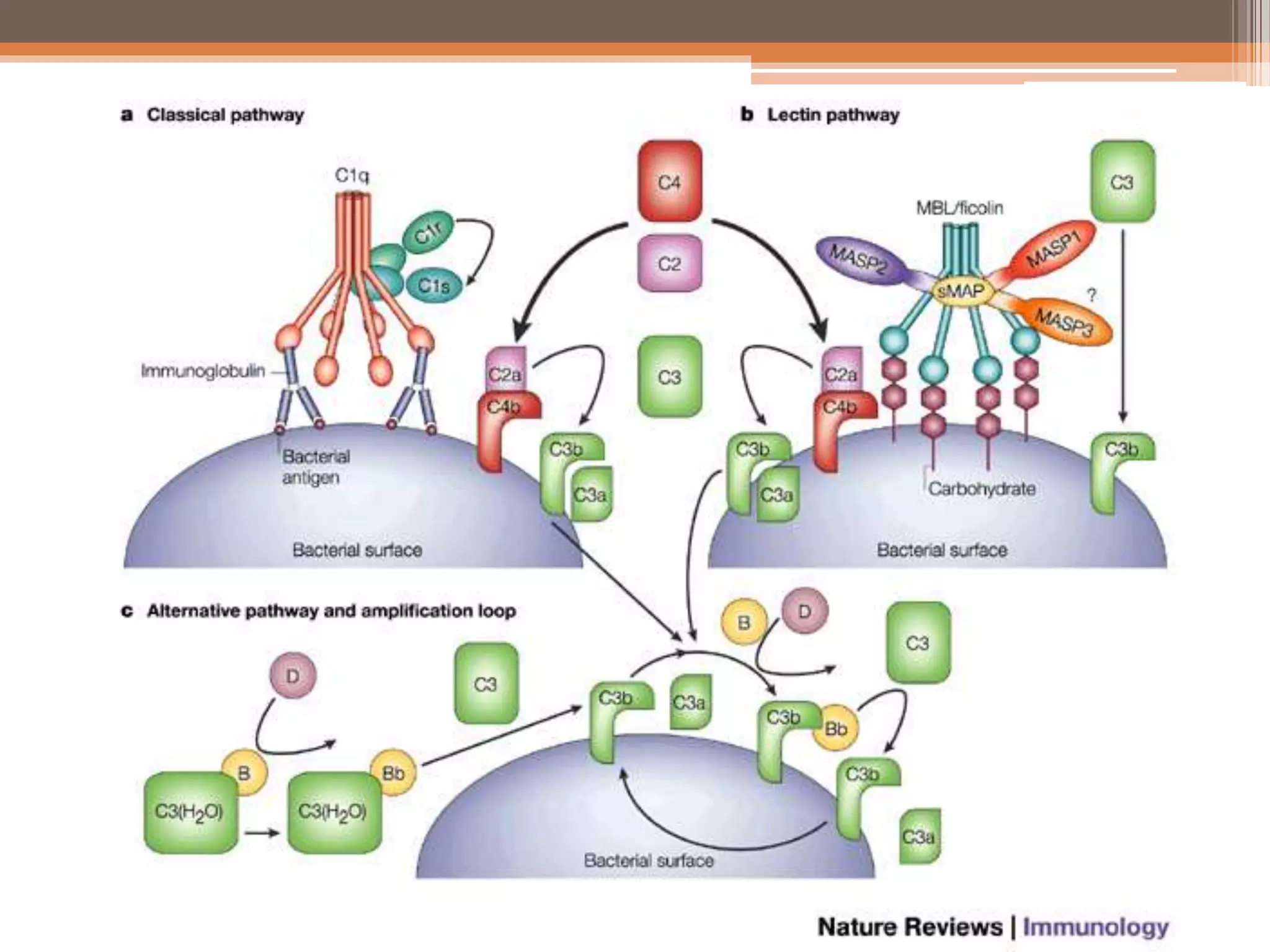
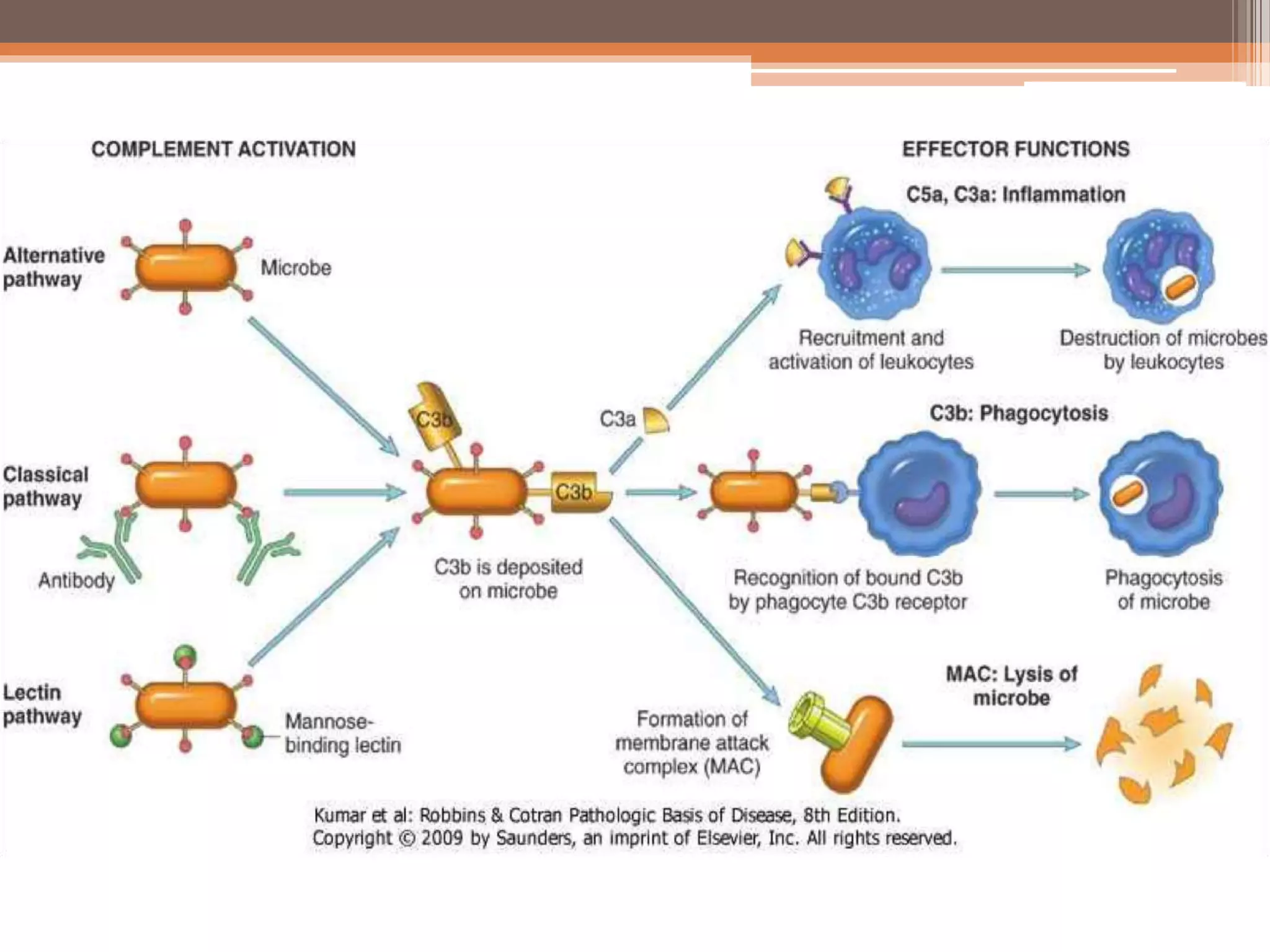
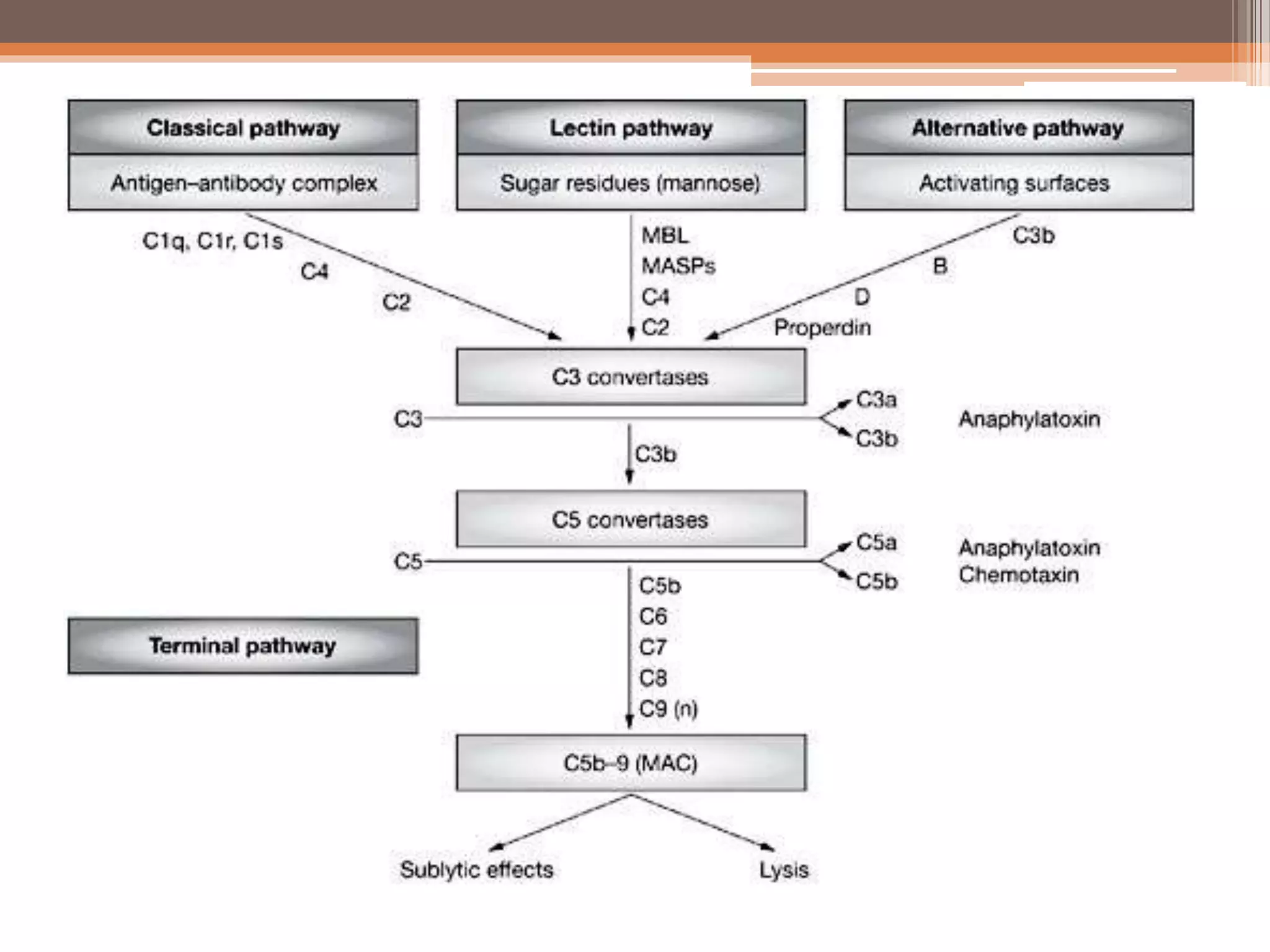
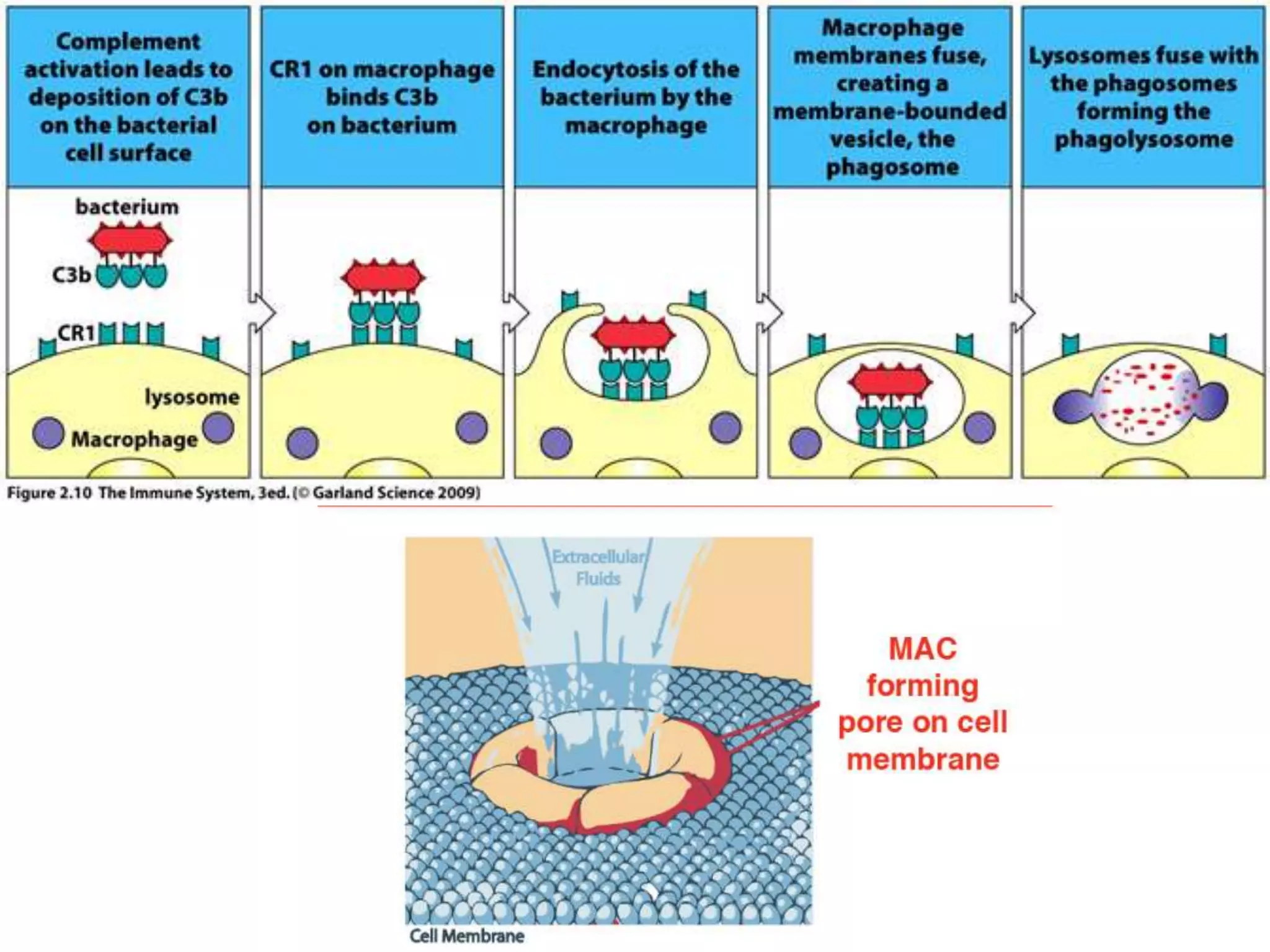
The complement system is a group of soluble proteins that activate inflammation, opsonization, and cell lysis in response to microbial agents. It functions via three pathways - the classical, lectin, and alternative pathways - which involve a sequential activation of complement components from C1 to C9. This leads to the formation of the membrane attack complex (MAC) and results in opsonization, chemotaxis of neutrophils, increased vascular permeability, and cellular lysis. The complement system is regulated by proteins like C1 inhibitor and decay accelerating factors to prevent damage to host cells.