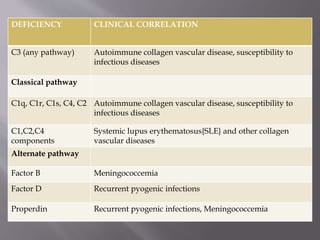
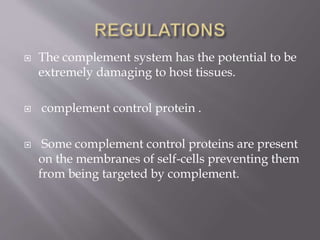
The document summarizes the complement system, including its regulation, biological effects, and deficiencies. It describes the key regulatory proteins that control complement activation and protect host cells. Deficiencies in complement proteins can increase susceptibility to infections and autoimmune diseases. The complement system helps eliminate pathogens through mechanisms like opsonization, chemotaxis, and cell lysis.

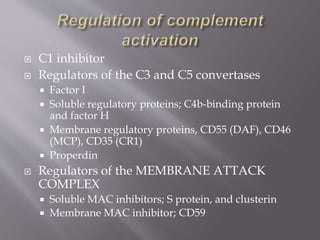
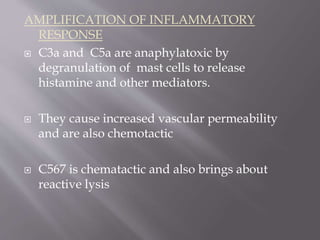
![ Regulatory proteins promotes or inhibits
complementary activity and protect self cell
lysis.
Decay acceleration factor[DAC] accelerates
break down of C3 convertase.
Homologous restriction factor[HRF]prevents
insertion of C8 and C9 into membranes.](https://image.slidesharecdn.com/complementsystem-150722045023-lva1-app6892/85/Complement-system-6-320.jpg)
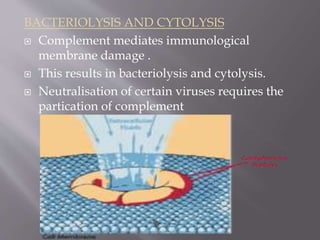
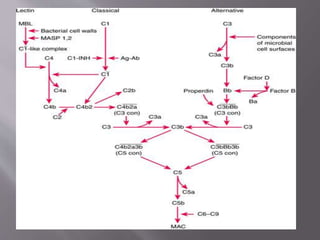
![HYPERSENSITIVITY REACTIONS
Complement participates in type 2 [cytotoxic]
and type 3[immune complex] hypersensity
reactions.](https://image.slidesharecdn.com/complementsystem-150722045023-lva1-app6892/85/Complement-system-12-320.jpg)