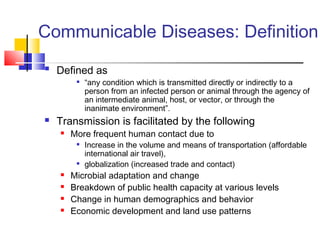
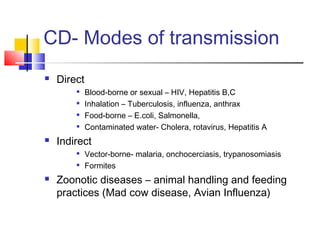
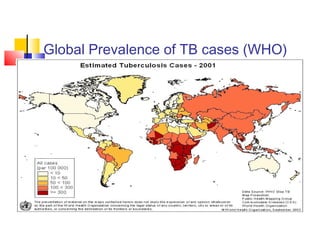
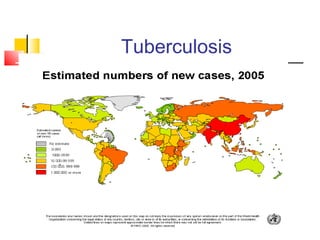
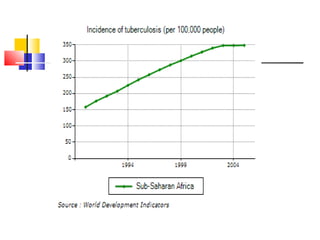
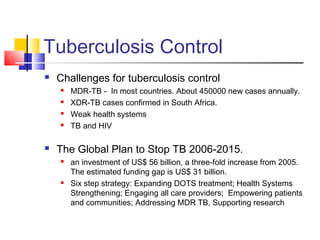
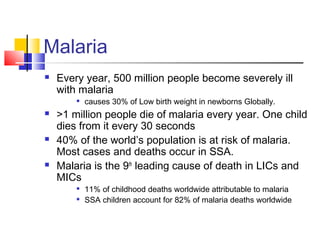
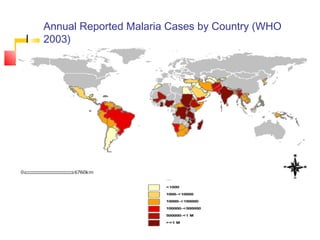
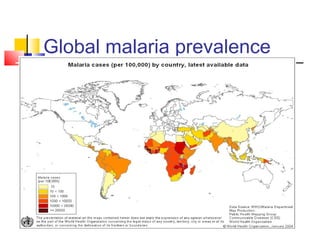
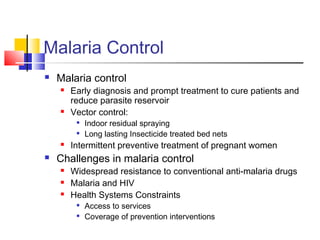
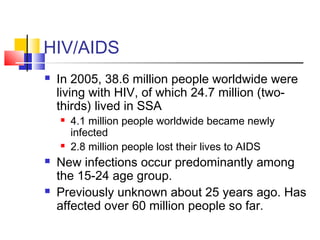
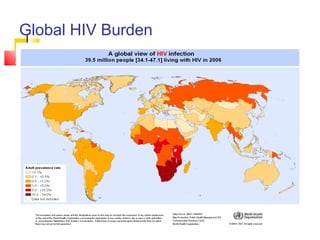
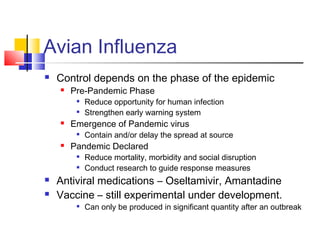
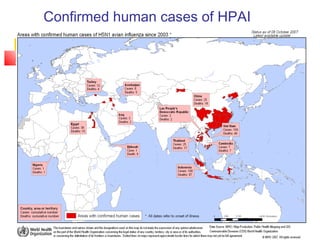
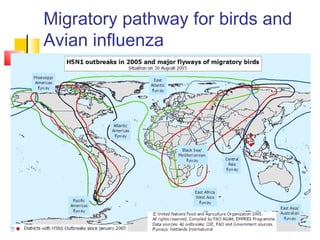
This document provides an overview of communicable diseases and their impact on human security. It defines communicable diseases as conditions transmitted directly or indirectly from infected people or animals. Selected diseases discussed include tuberculosis, malaria, HIV/AIDS, and avian influenza. These diseases place a significant burden on low and middle income countries and can have social, economic, and security impacts. Approaches to control discussed include personal responsibility, public health interventions, regulations and laws, and partnerships. Effective response requires a global approach as communicable diseases respect no borders in an increasingly interconnected world.