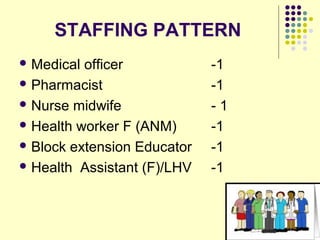
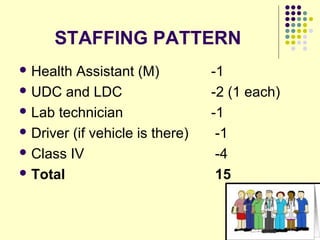
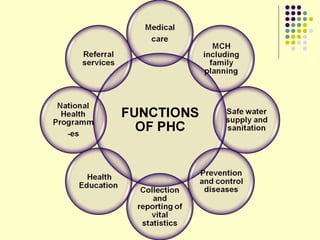
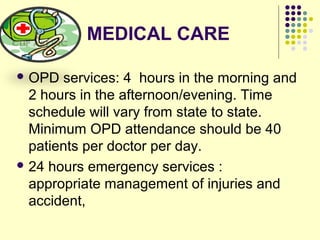
The primary health centre occupies a key position in rural health care as the first point of contact between individuals and the health system. It aims to provide comprehensive and affordable preventive, promotive, and curative services to rural populations of about 30,000 in plains and 20,000 in hilly/tribal areas. Staffing typically includes a medical officer, pharmacist, nurse, and other paramedics. Services include outpatient and inpatient care, maternal and child health services, immunizations, nutrition programs, and monitoring of national health programs.