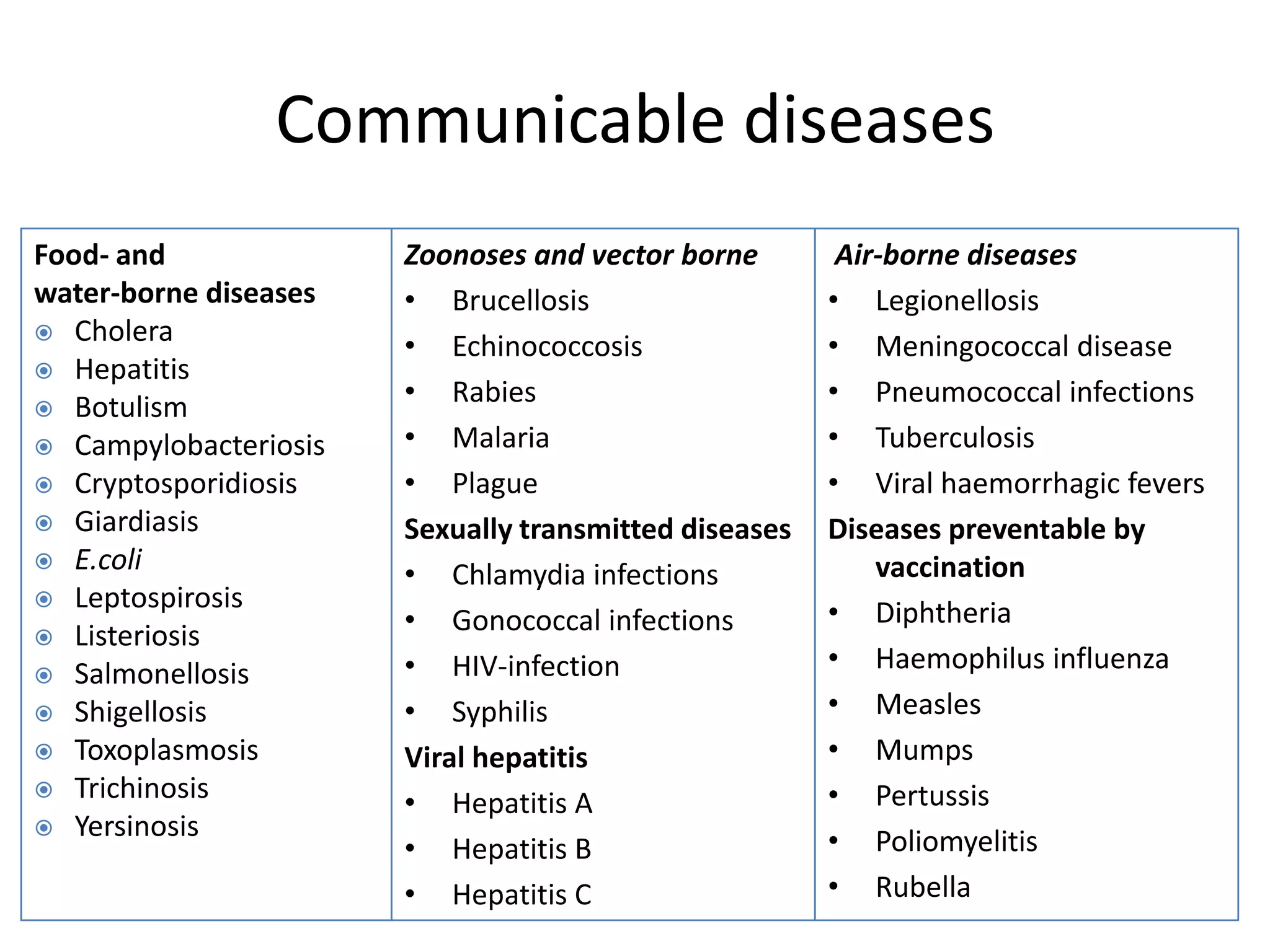
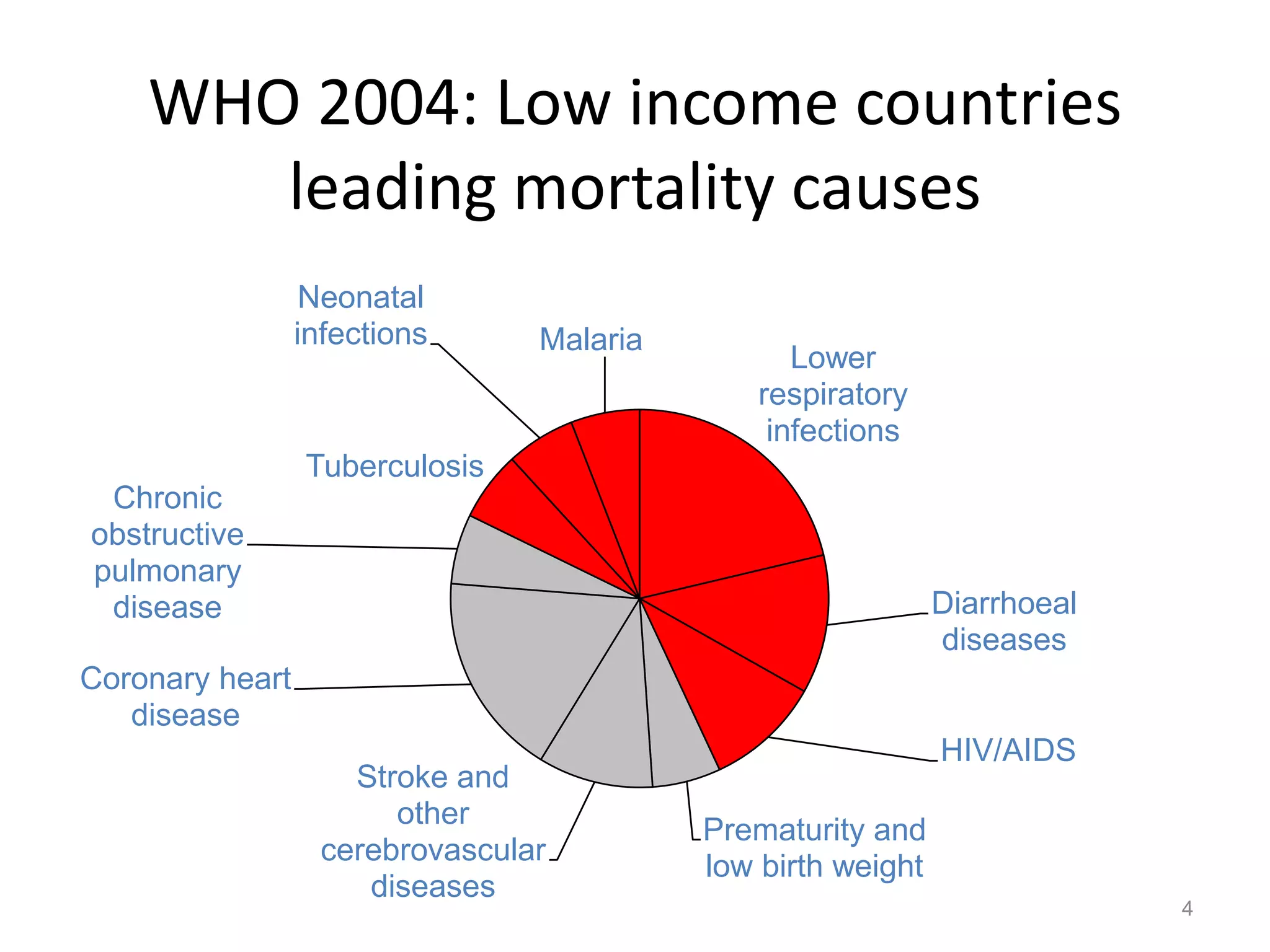
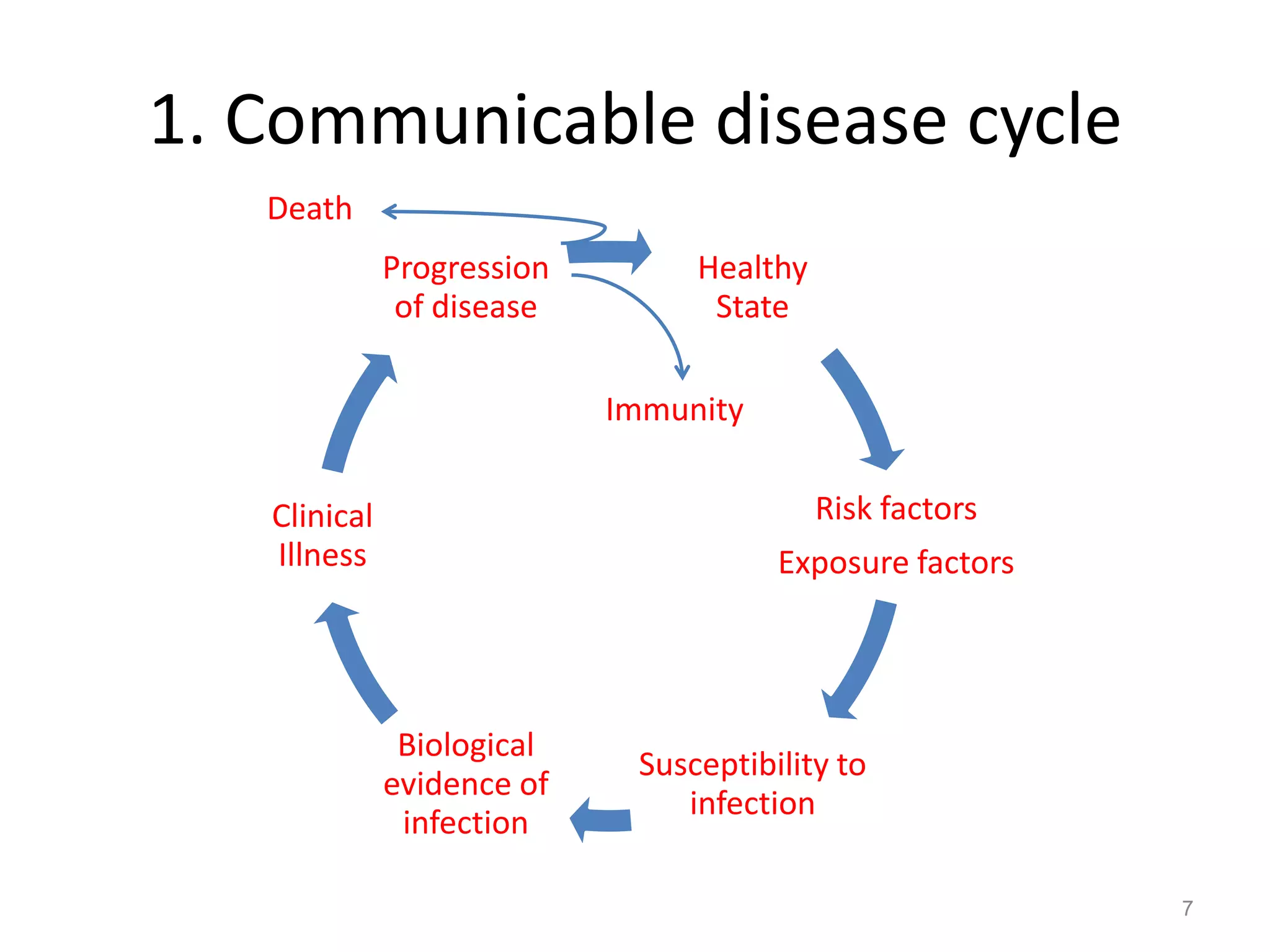
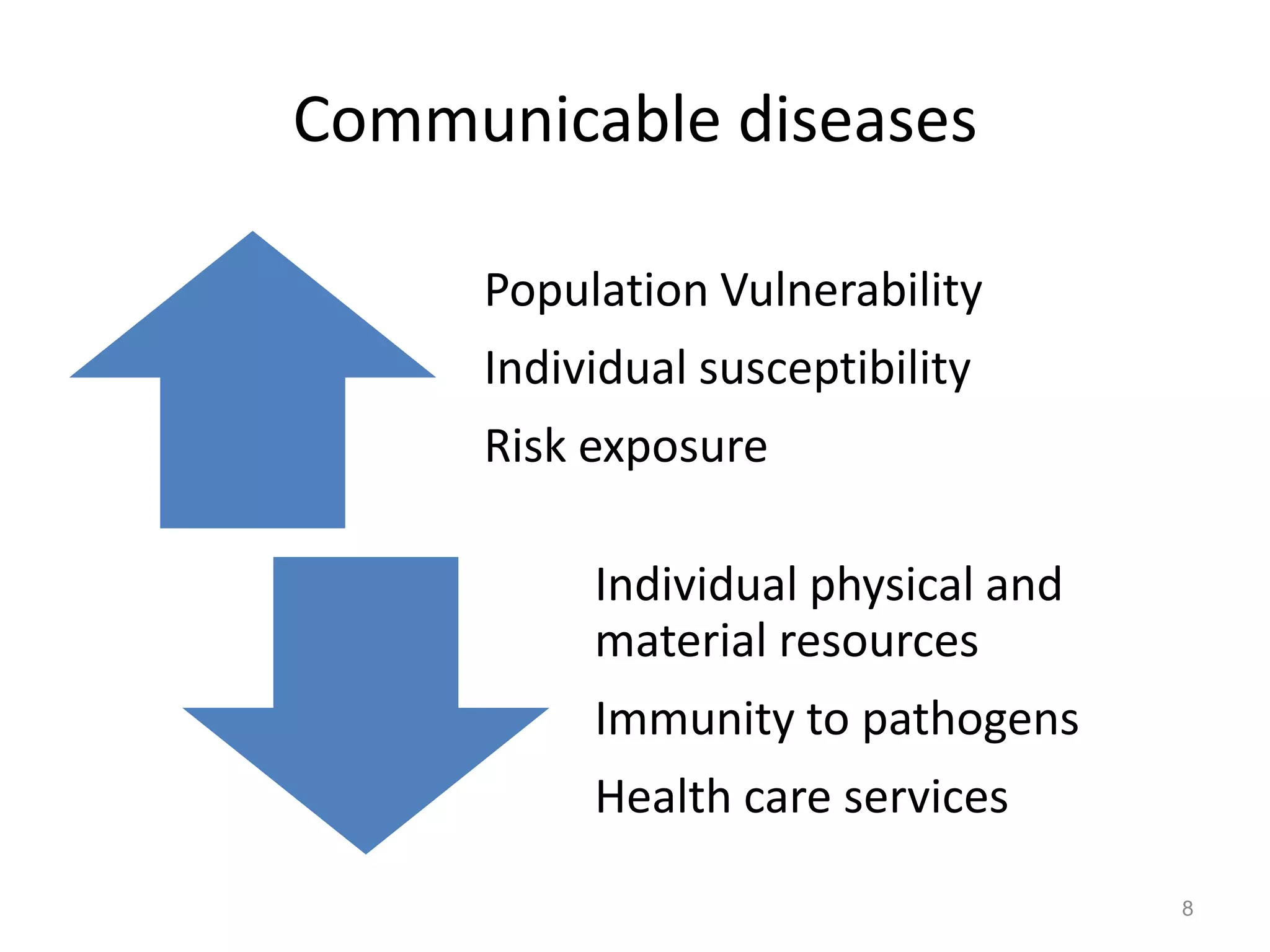
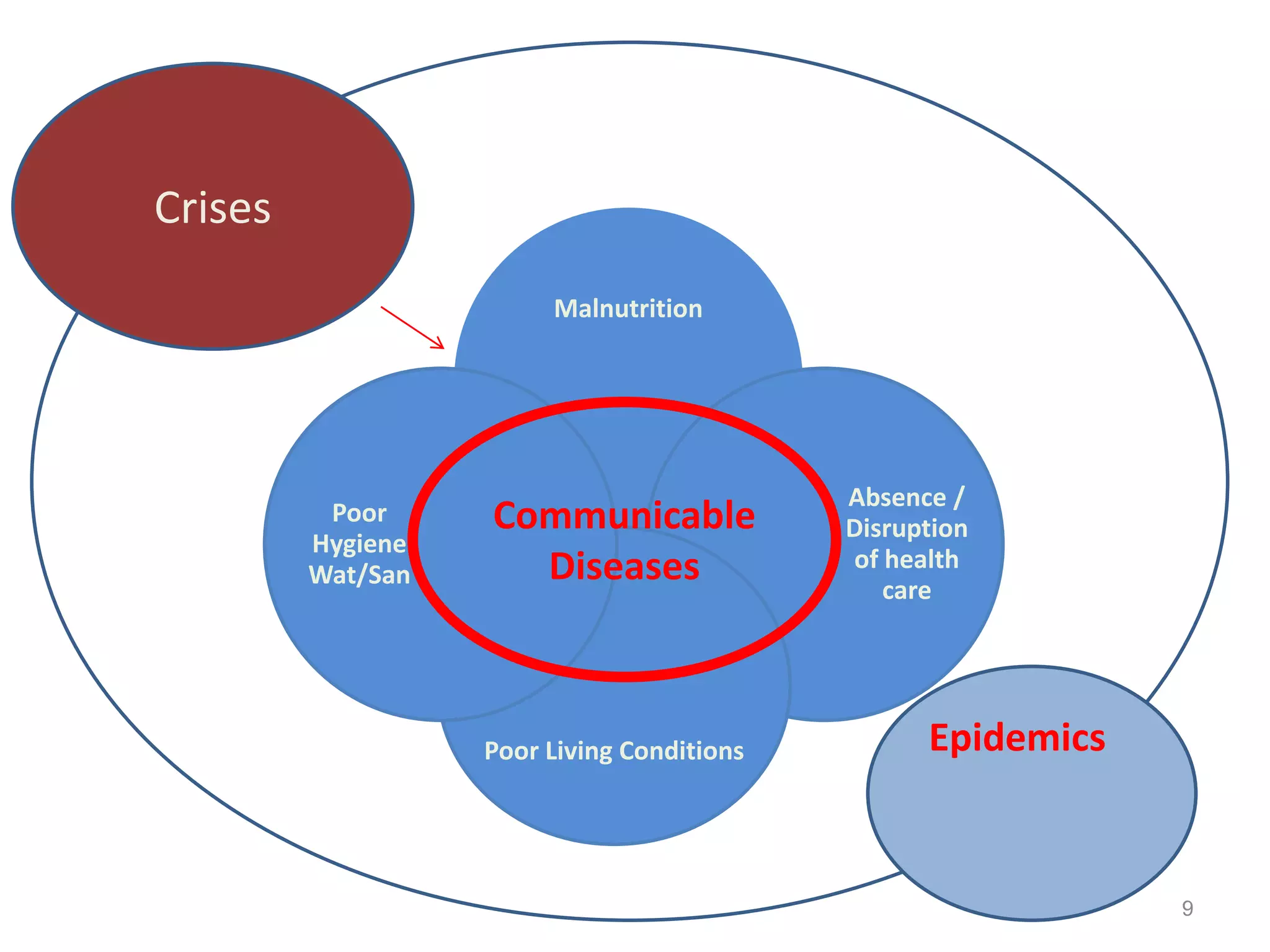
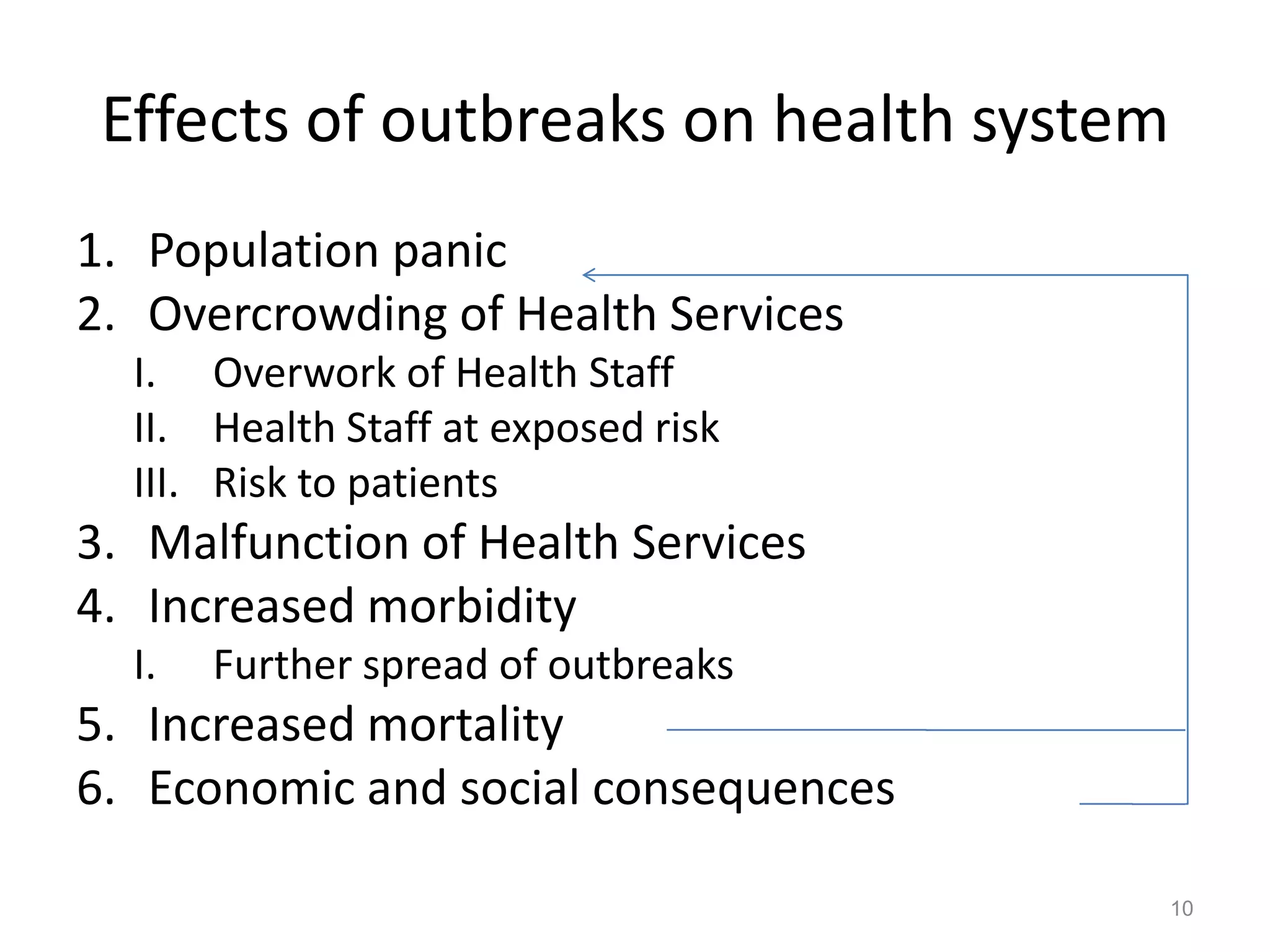
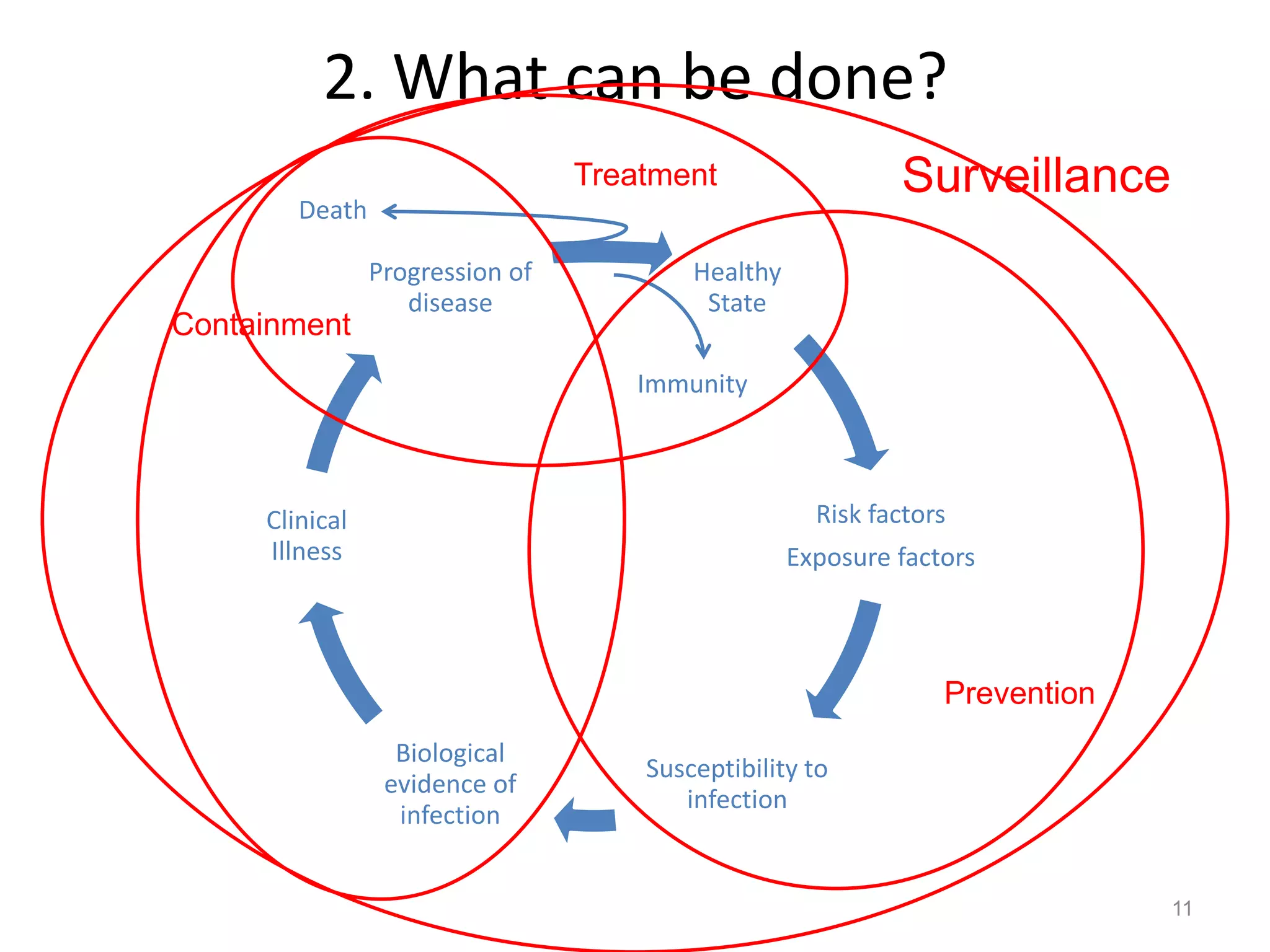
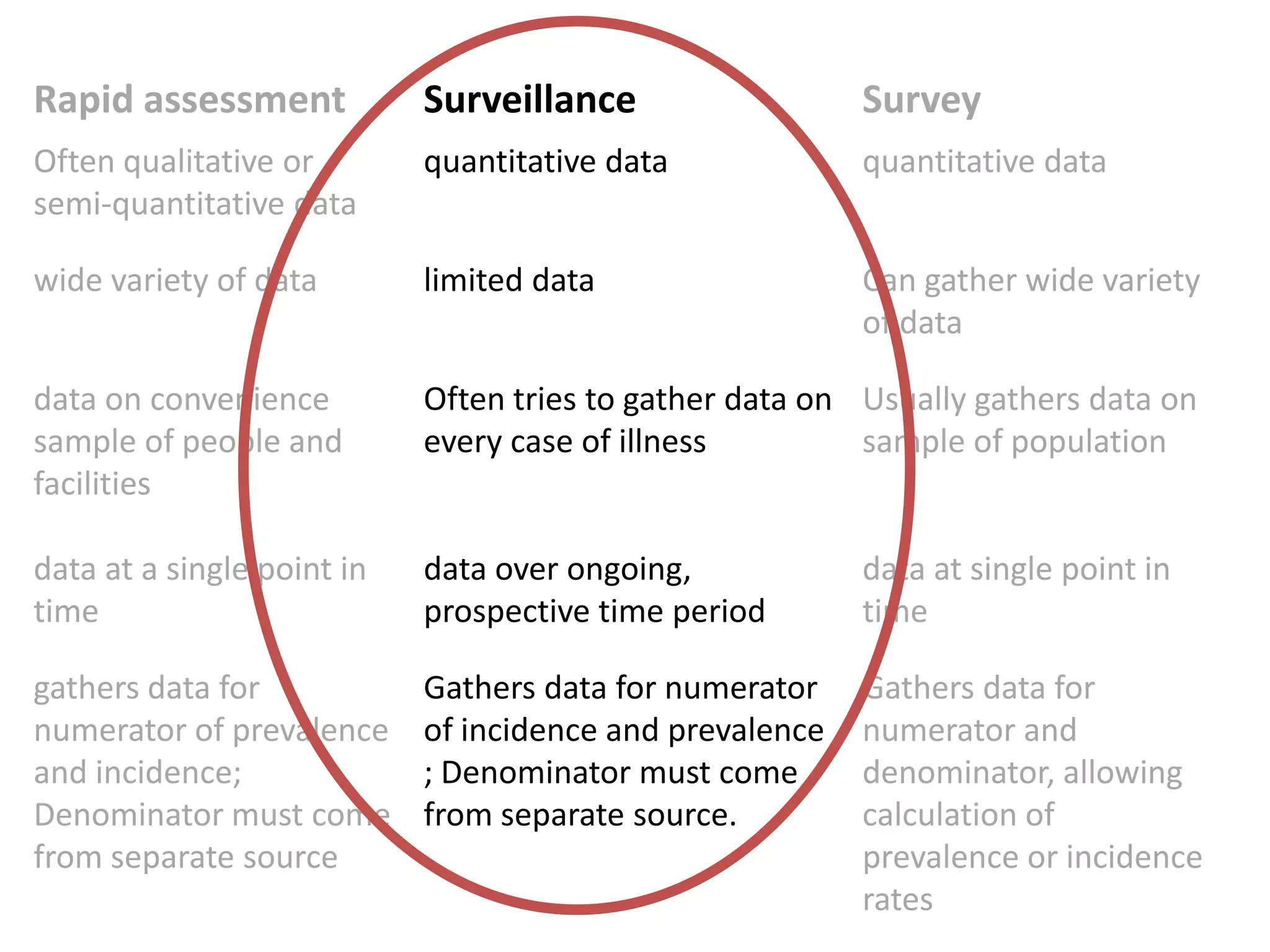
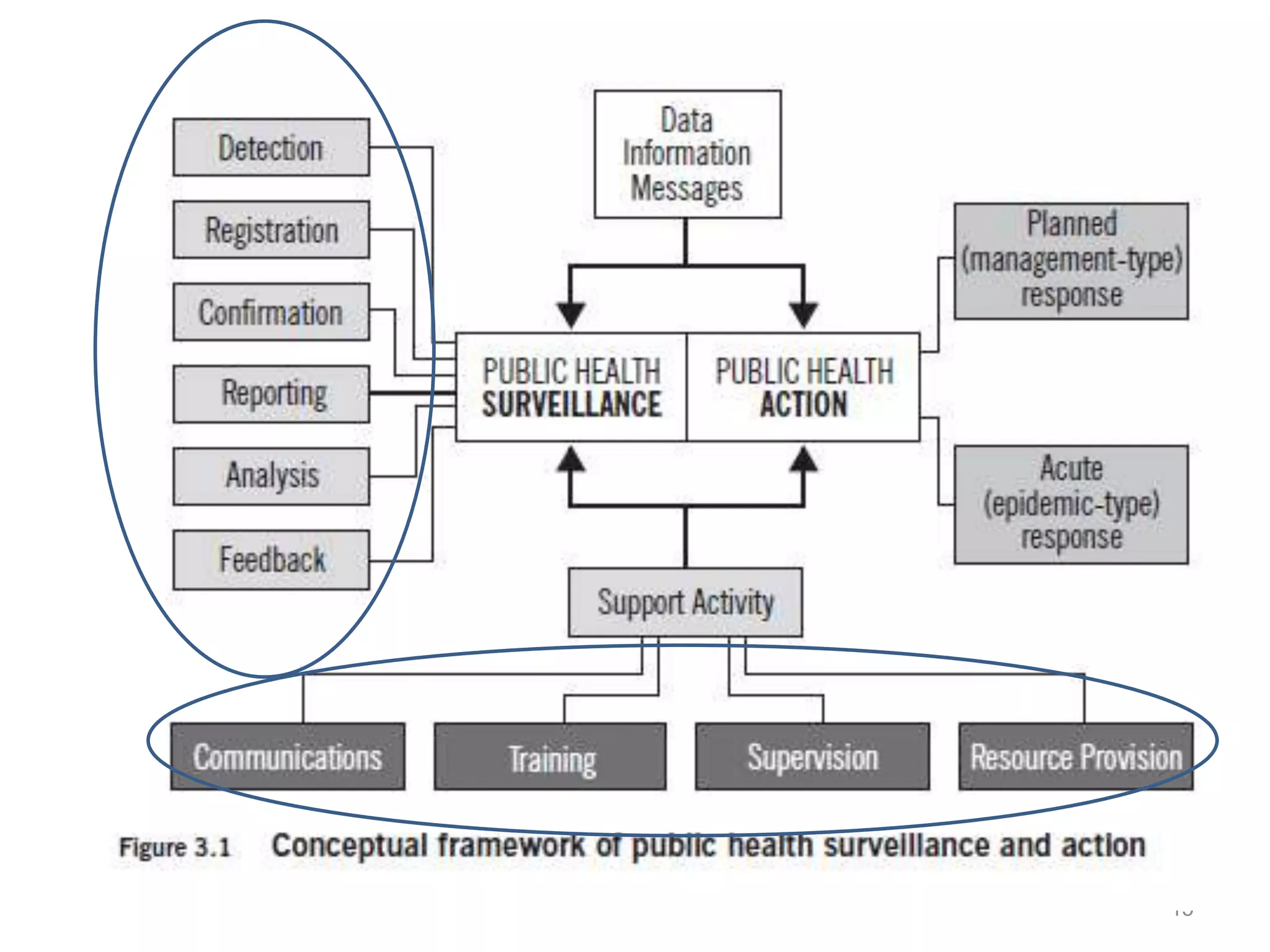
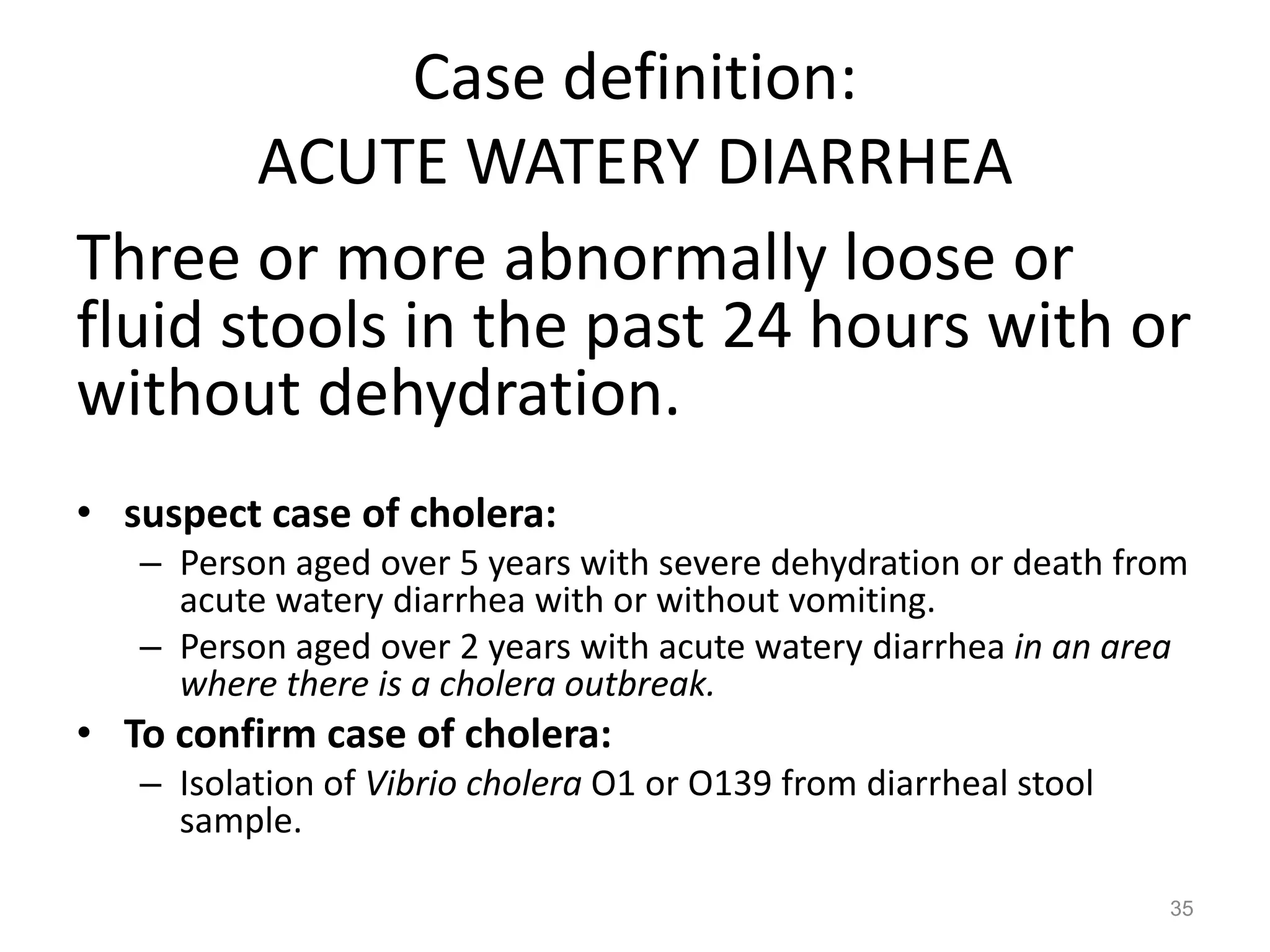
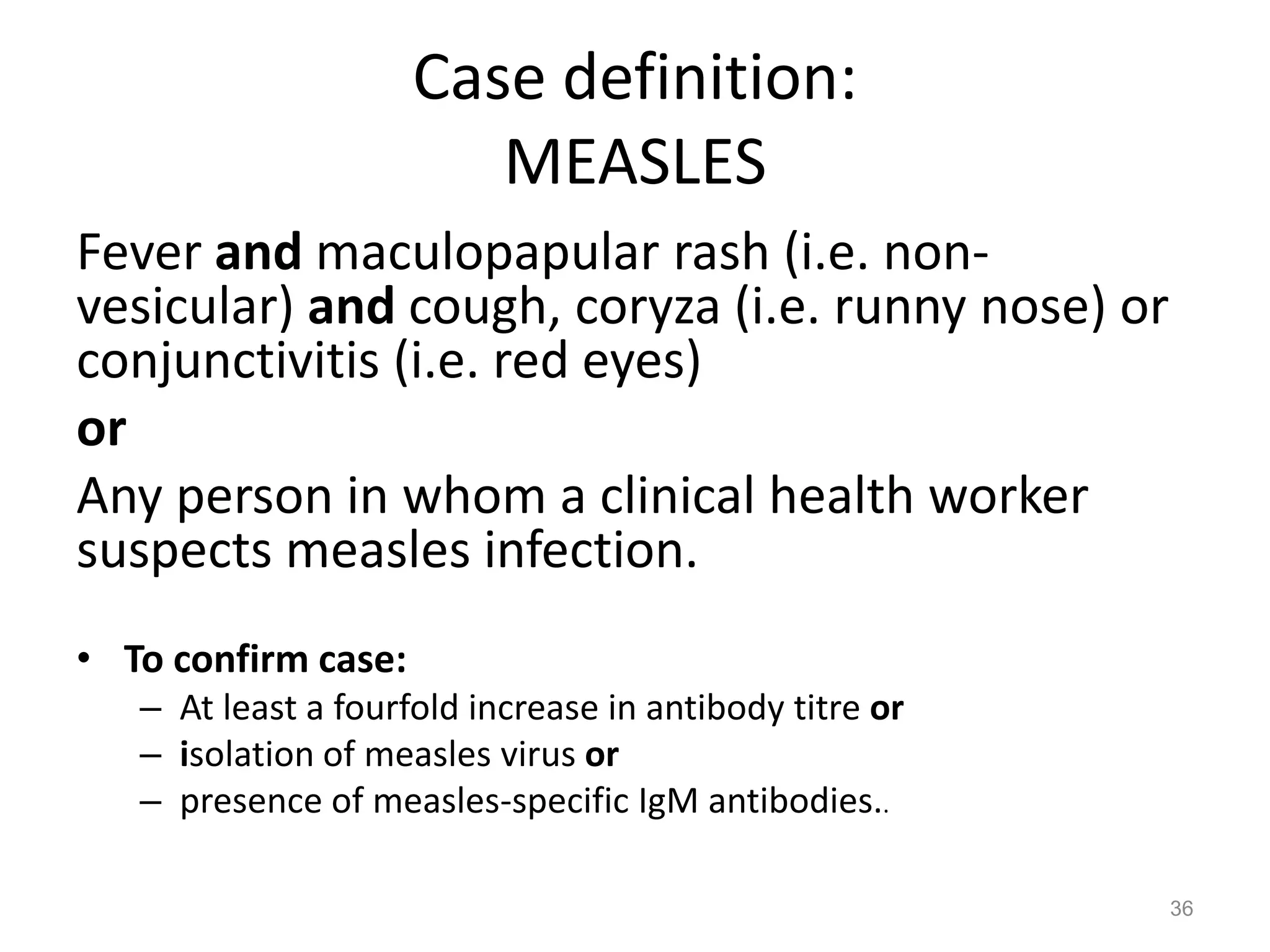
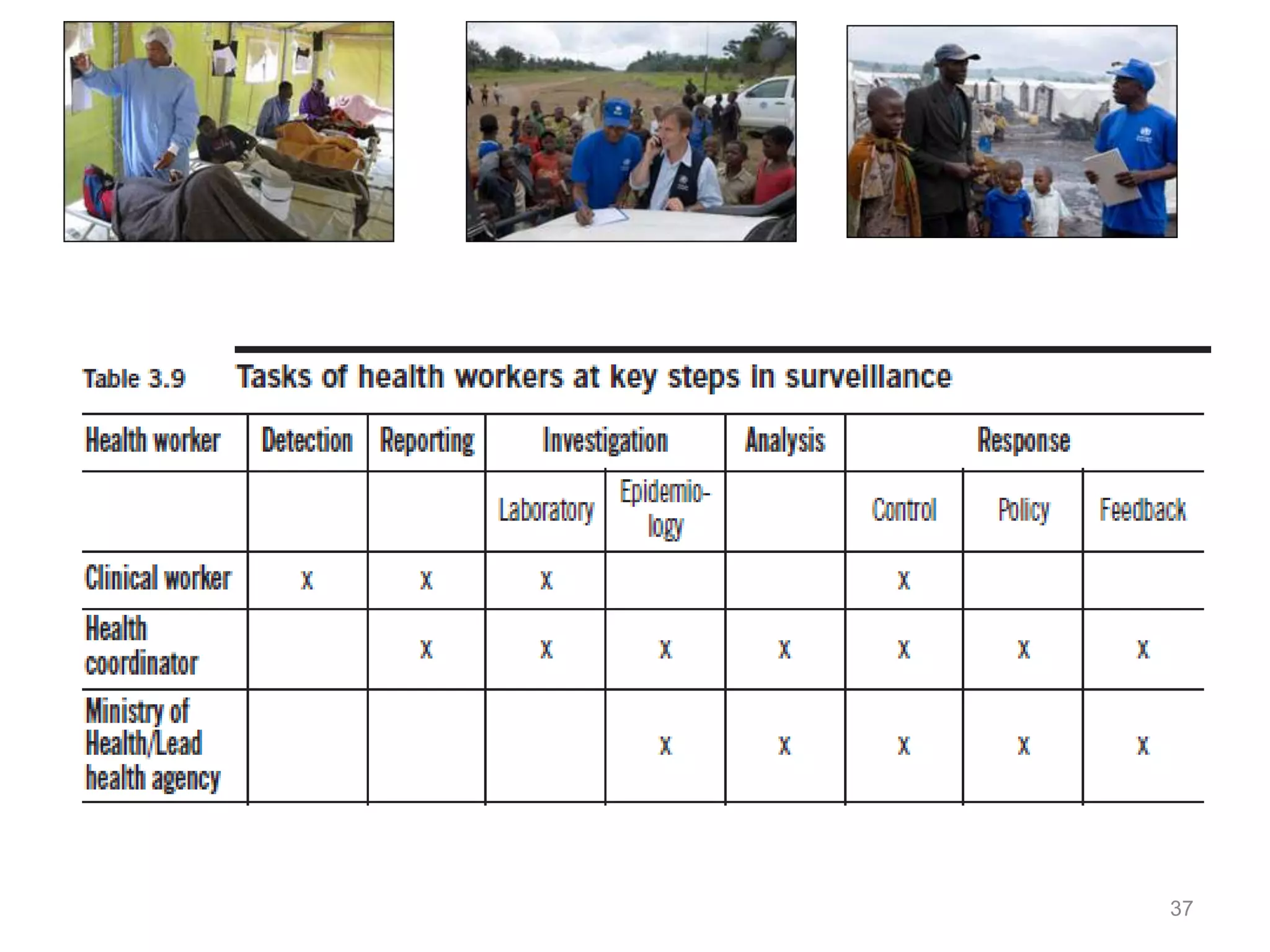
This document discusses communicable diseases in humanitarian settings. It defines communicable diseases and lists examples of food- and water-borne diseases, zoonoses and vector-borne diseases, air-borne diseases, sexually transmitted diseases, and vaccine-preventable diseases. It also discusses the disease burden in low-income countries and the MDG targets related to HIV/AIDS, malaria and other diseases. Finally, it covers topics such as the disease cycle, surveillance, prevention and control measures for communicable diseases in humanitarian crises."