This document provides information about peripherally inserted central catheters (PICCs):
1. It discusses the benefits, risks, and characteristics of PICCs including catheter types, styles, sizes, and lengths.
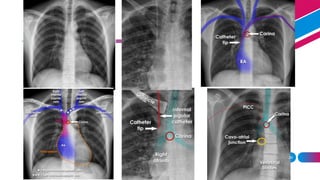
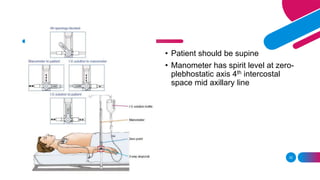
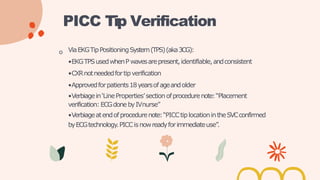
2. It describes the PICC placement procedure and methods for verifying catheter tip location using chest x-ray or EKG tip positioning systems.
3. It outlines considerations for PICC assessment including patient complaints, new cardiac issues, extremity edema, catheter migration, and issues requiring consultation with the IV team.
4. It briefly mentions PICC line care including flushing procedures and discontinuing a PICC which requires a physician/provider order.