This document provides information about culdocentesis, including:
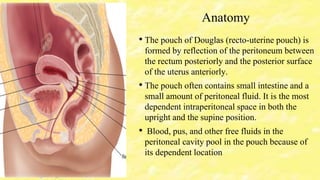
1. Culdocentesis is a procedure to obtain peritoneal fluid from the pouch of Douglas in the female pelvis for diagnostic purposes.
2. The pouch of Douglas is located between the rectum and posterior uterus and often contains small amounts of peritoneal fluid.
3. Culdocentesis may be used to diagnose conditions like ectopic pregnancy, ruptured ovarian cysts, and pelvic inflammatory disease.






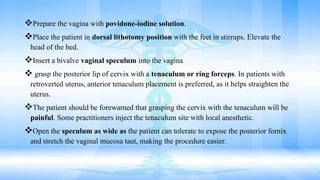
![Equipments
• Bivalve vaginal speculum (Graves or Pederson)
• Tenaculum or Allis clamp
• Ring forceps
• Spinal needle, 18 gauge (ga)
• Monsel solution (ferric subsulfate) for hemostasis
• Butterfly needle, 19 ga
• Needle, 25 ga, 1 inch
• Antiseptic (eg, povidone-iodine solution [Betadine])
• Lidocaine (1-2%) with epinephrine
• Specimen container
• Light source](https://image.slidesharecdn.com/pavanculdocentesis-180517073307/85/Culdocentesis-8-320.jpg)