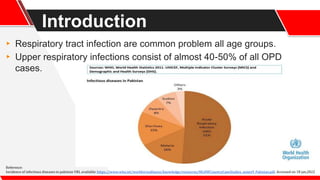
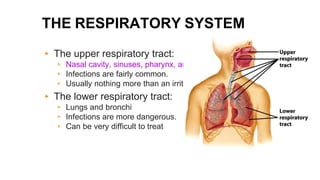
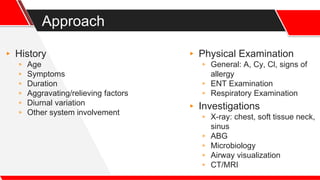
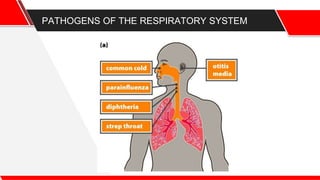
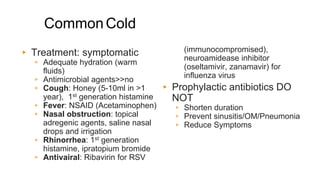
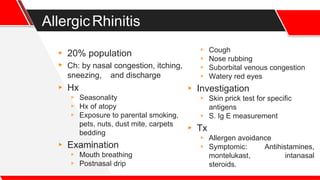
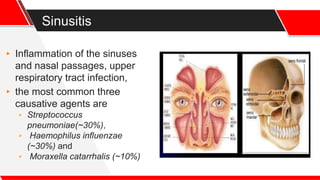
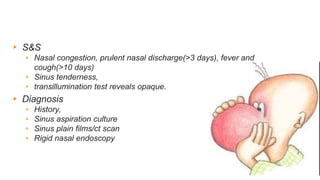
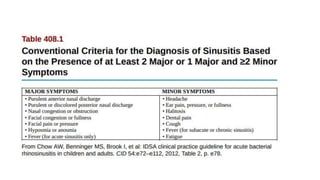
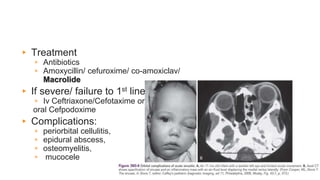
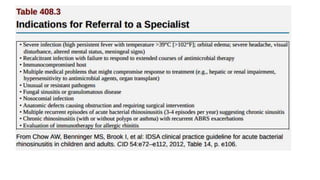
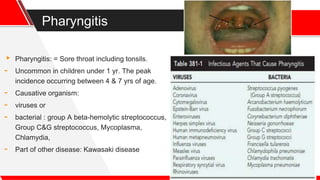
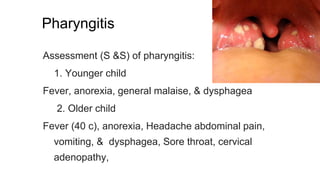
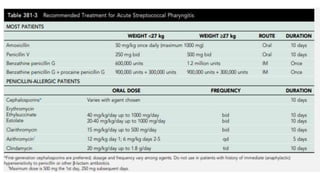
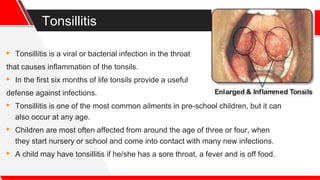
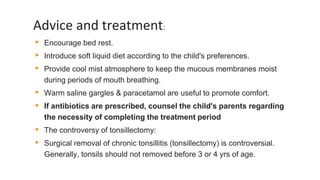
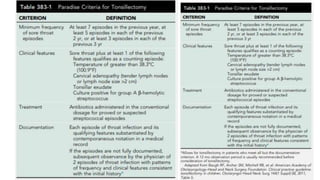
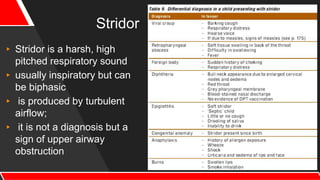
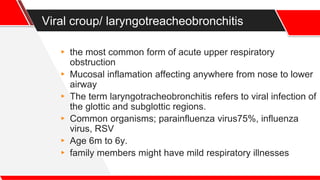
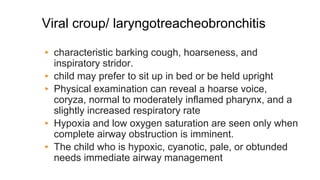
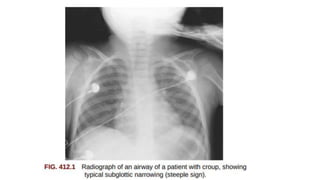
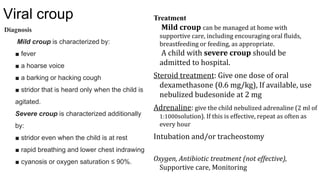
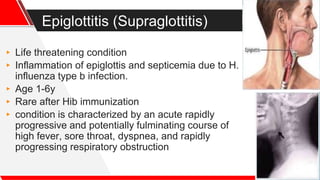
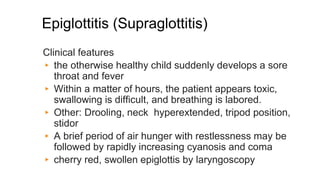
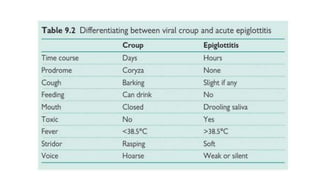
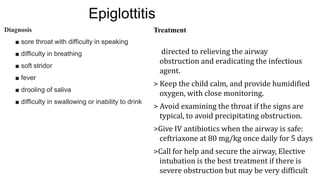
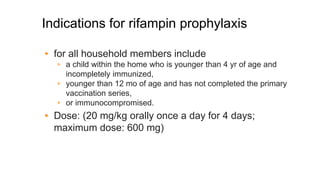
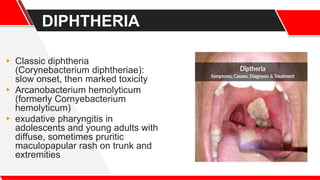
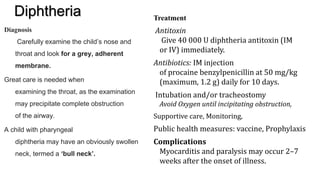
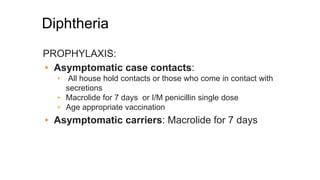
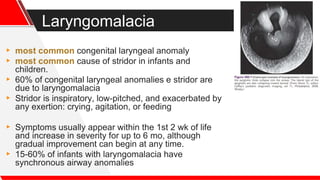
This document discusses the approach to assessing and treating upper respiratory tract infections (URTIs) in children. It begins by introducing URTIs as a common problem, then describes the anatomy of the respiratory tract. It outlines symptoms of URTIs and the approach to taking a history and examining the patient. It discusses common causes of URTIs like the common cold, allergic rhinitis, sinusitis, pharyngitis, and more severe conditions like croup, epiglottitis and diphtheria. For each condition, it covers symptoms, diagnosis, treatment and prevention.