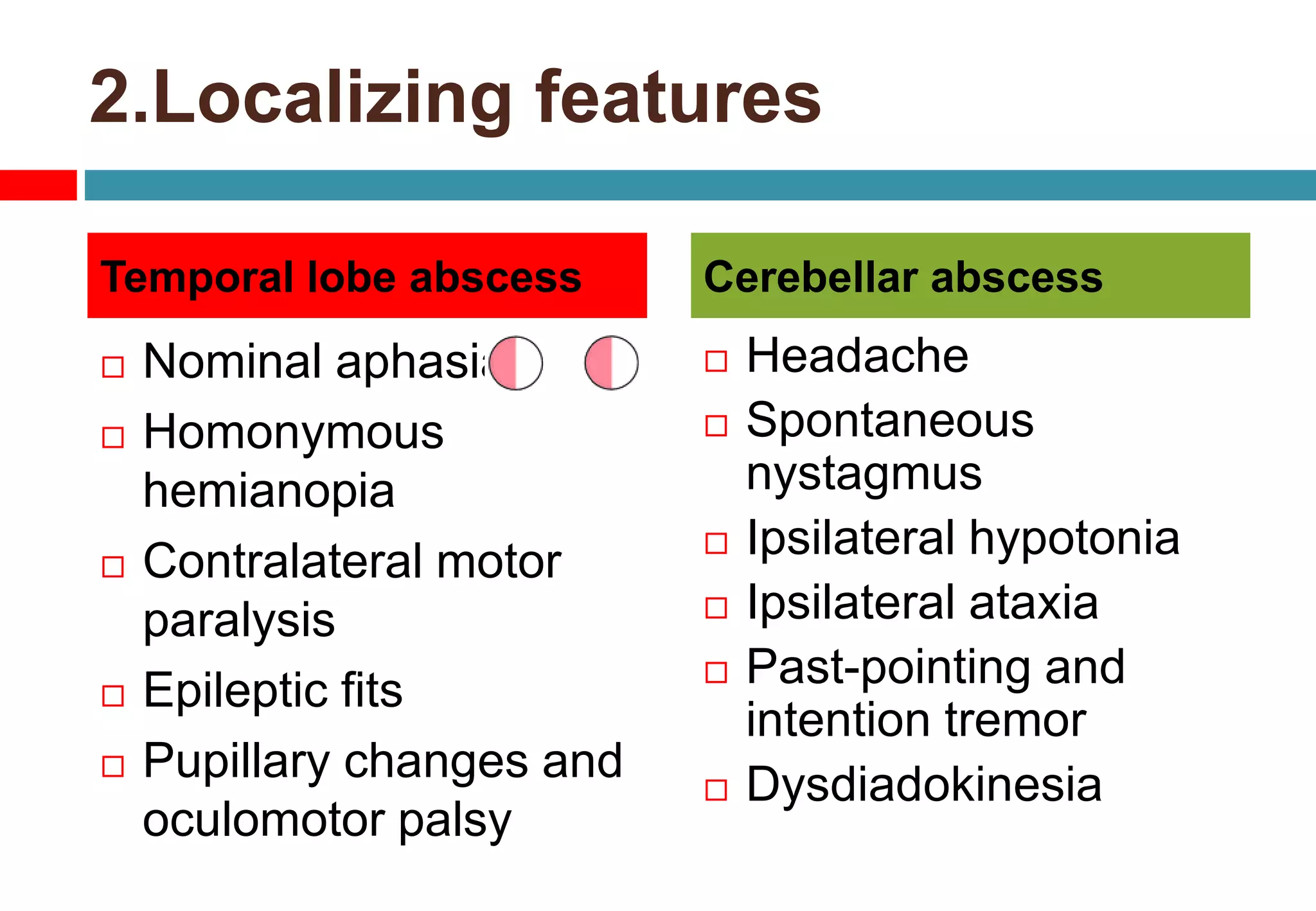
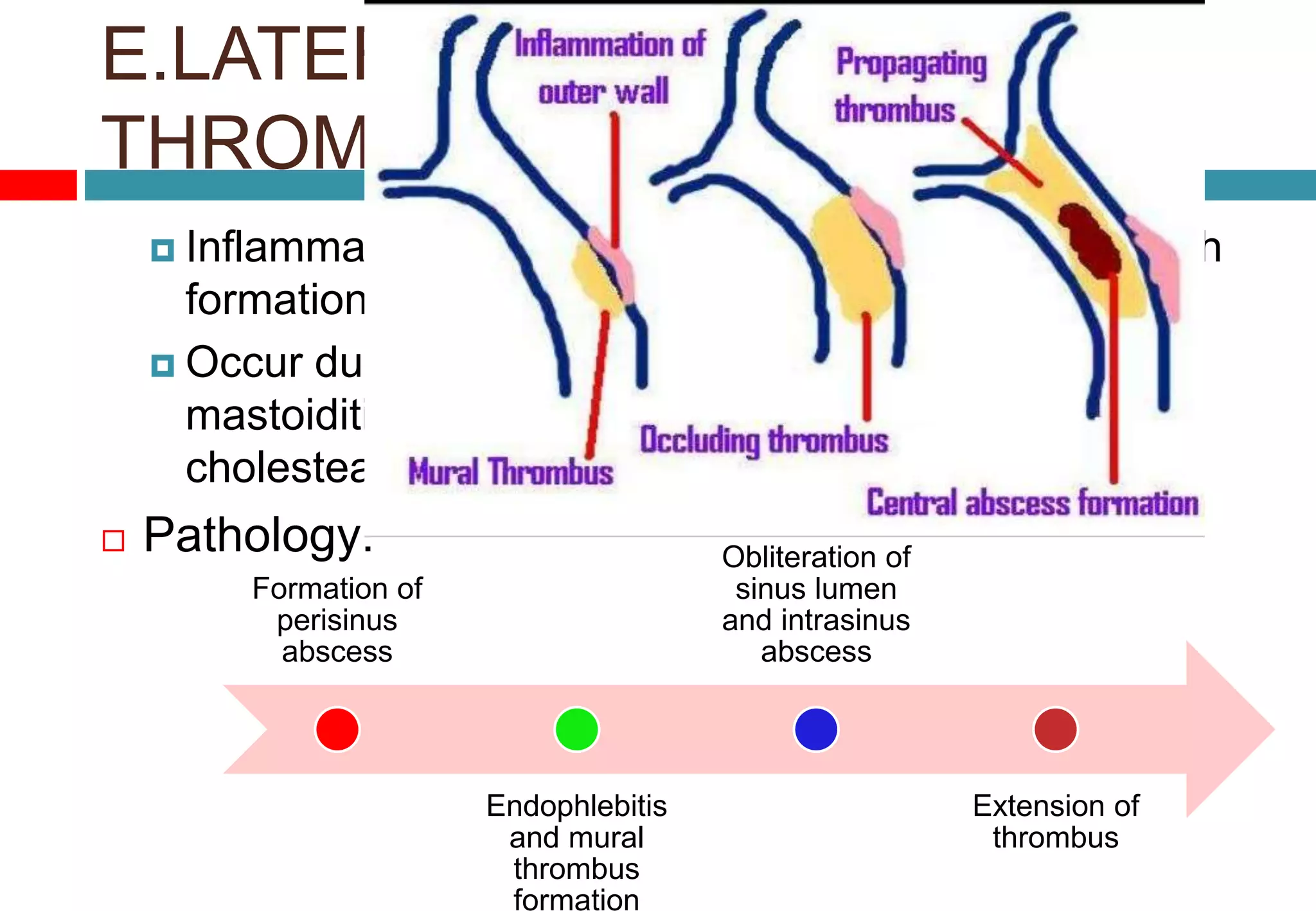
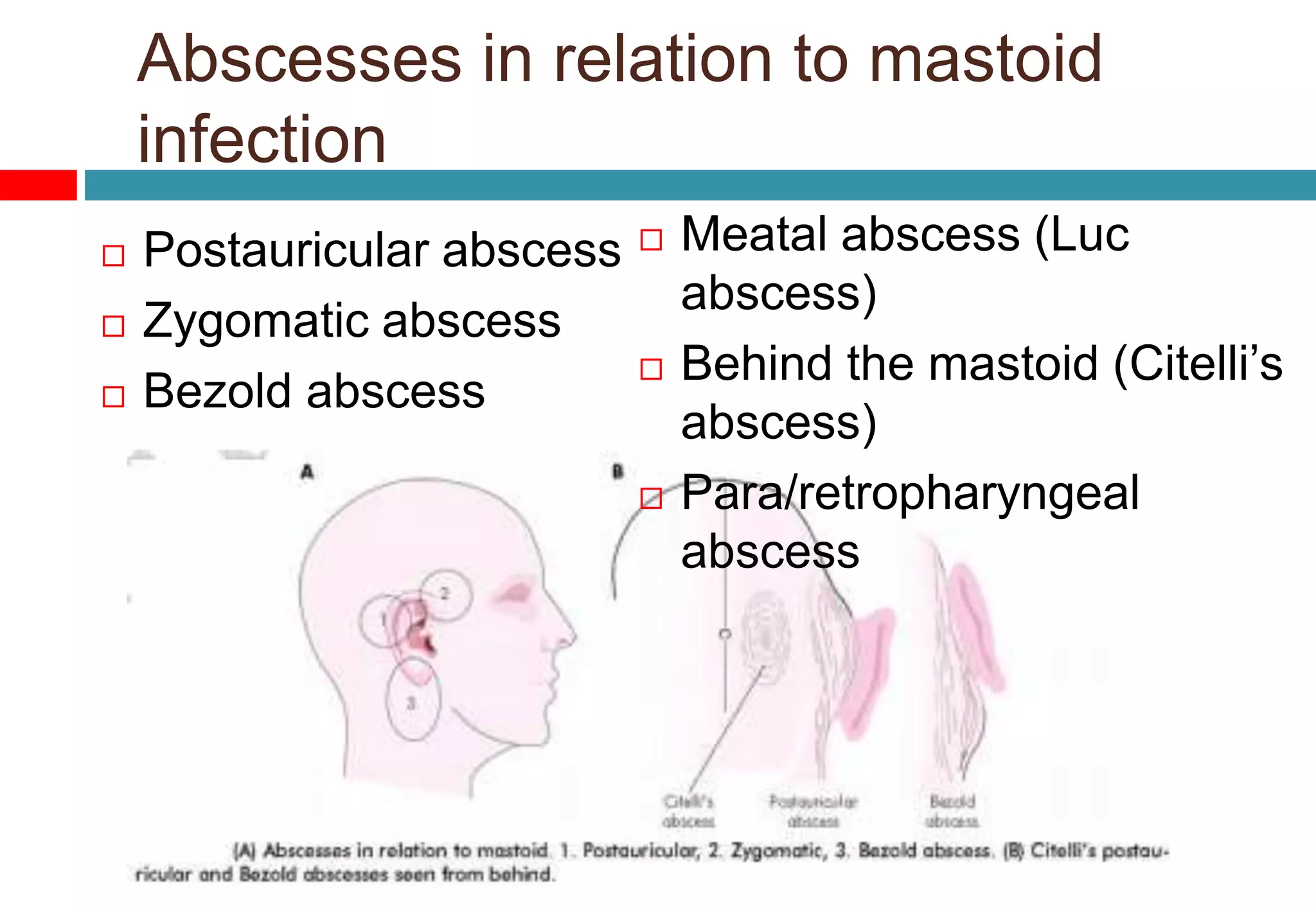
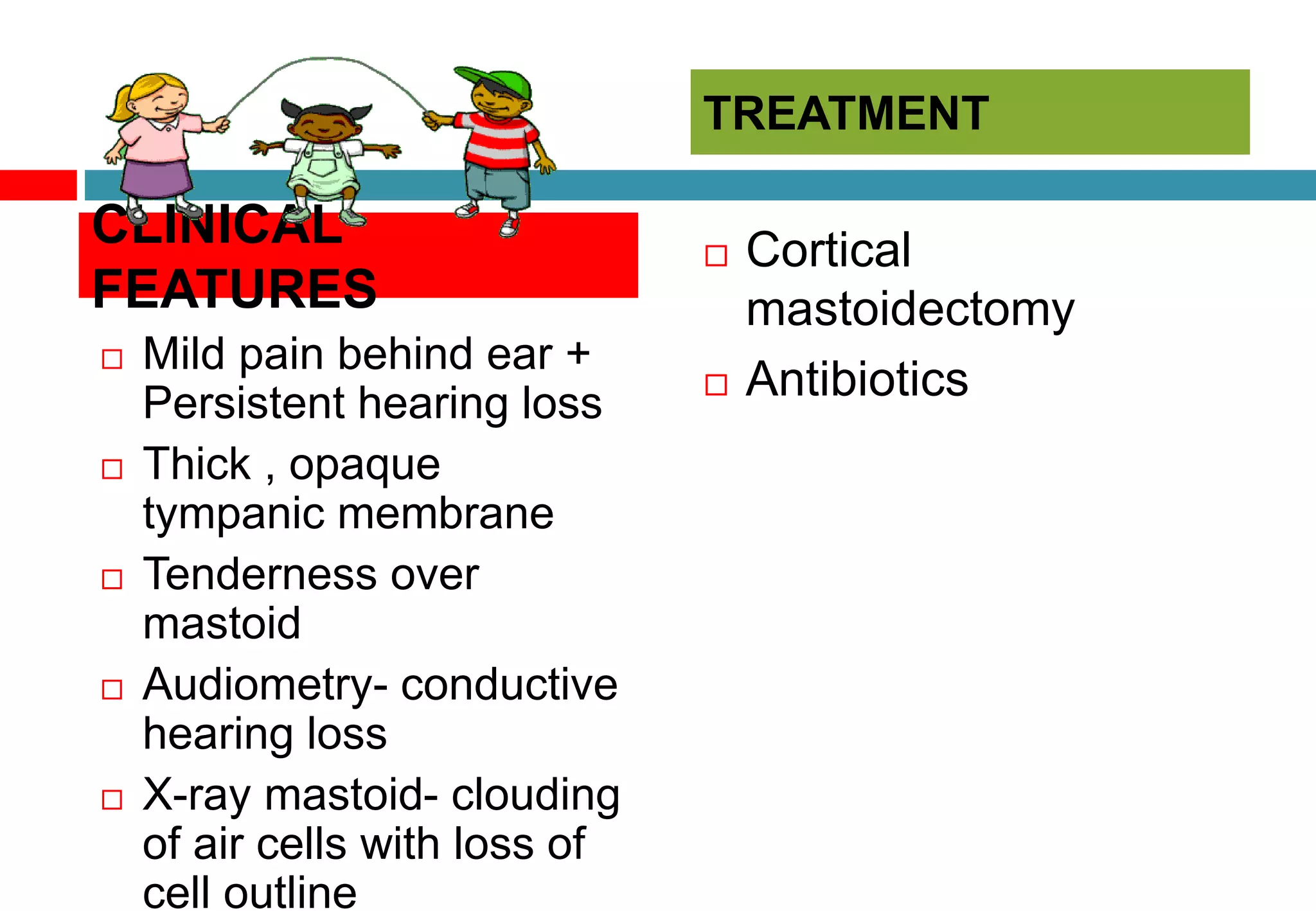
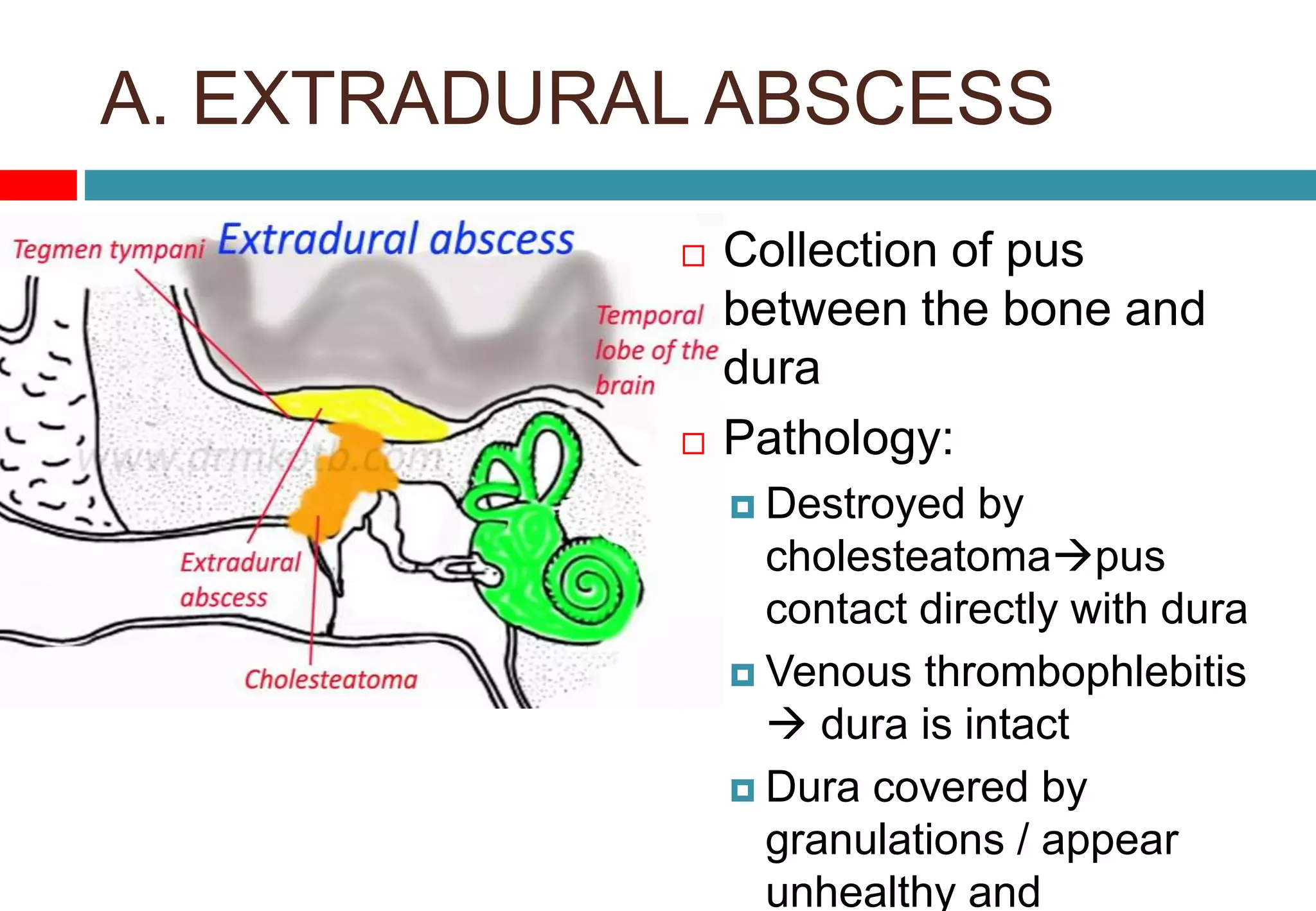
This document discusses chronic suppurative otitis media, including factors that contribute to it, classifications, potential complications, and treatments. It covers both intratemporal complications like mastoiditis, petrositis, and facial paralysis, as well as intracranial complications such as extradural abscess, subdural abscess, meningitis, and brain abscess. For each complication, it discusses the pathology, clinical features, investigations, differential diagnosis, and treatment approaches.





![A. [i] ACUTE MASTOIDITIS
Inflammation of
mucosal lining
of antrum and
mastoid air cell
system
mucosa bony
walls](https://image.slidesharecdn.com/melssyr4entcomplicationofcsom-160310165027/75/Melss-yr4-ent-complication-of-cs-om-9-2048.jpg)
![Accompanies / follow
ASOM
1. Virulence of organism
2. Lowered resistance
3. Children
1. Production of pus
under tension
Production > drainage
2. Hyperaemic
decalcification and
osteoclastic resorption
of bony wall
Destruction,
coalescence of
mastoid air cell
[empyema of mastoid]
subperiosteal
Aetiology PATHOLOGY](https://image.slidesharecdn.com/melssyr4entcomplicationofcsom-160310165027/75/Melss-yr4-ent-complication-of-cs-om-10-2048.jpg)

![Treatment
Hospitalization
Antibiotics
Myringotomy
Cortical
mastoidectomy
[Subperiosteal abscess,
positive resevoir sign, no
change despite medical
treatment for 48hours]](https://image.slidesharecdn.com/melssyr4entcomplicationofcsom-160310165027/75/Melss-yr4-ent-complication-of-cs-om-14-2048.jpg)








![B. SUBDURAL ABSCESS
Pus between dura and
archnoid
Pathology
Spreads by erosion of
bone and dura
/thrombophlebitic
process subdural
space and comes to lie
against the convex
surface of cerebral
hemisphere
Clinical features
Meningeal irritation [
headache, fever, neck
rigidity, Kernig’s sign]
Cortical venous
thrombophlebitis [
aphasia, hemiplegia]
Raised ICP [
papilledema, ptosis,
dilated pupil ]
Treatment:
burr holes /craniotomy
for drainage +IV
antibiotics](https://image.slidesharecdn.com/melssyr4entcomplicationofcsom-160310165027/75/Melss-yr4-ent-complication-of-cs-om-30-2048.jpg)


![D. OTOGENIC BRAIN ABSCESS
Adult ( 50%) : CSOM with
cholesteatoma
Child ( 25%) : acute otitis media
Route of infection:
Cerebral : direct extension through
tegmen /retrograde thrombophlebitis
Cerebellar : direct extension through
Trautmann’s triangle / retrograde
thrombophlebitis
Bacteriology:
aerobic [ SP, PM, EC,]
Anaerobic [ BF, HI]](https://image.slidesharecdn.com/melssyr4entcomplicationofcsom-160310165027/75/Melss-yr4-ent-complication-of-cs-om-33-2048.jpg)