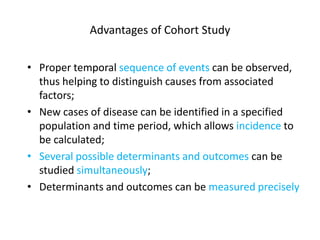
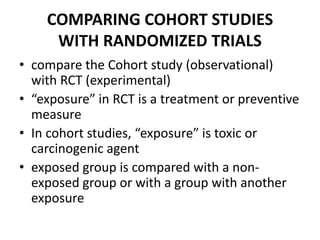
This document describes cohort studies and their use in epidemiological research. It defines a cohort study as one that follows a group of individuals over time to examine exposure to factors and subsequent health outcomes. It notes advantages as allowing observation of temporal relationships but disadvantages as requiring large sample sizes and long follow-up periods. The document outlines the design of cohort studies, including prospective and retrospective approaches. It discusses evaluating disease incidence by comparing exposed and non-exposed groups. Finally, it covers potential biases in cohort studies from selection effects and incomplete information.