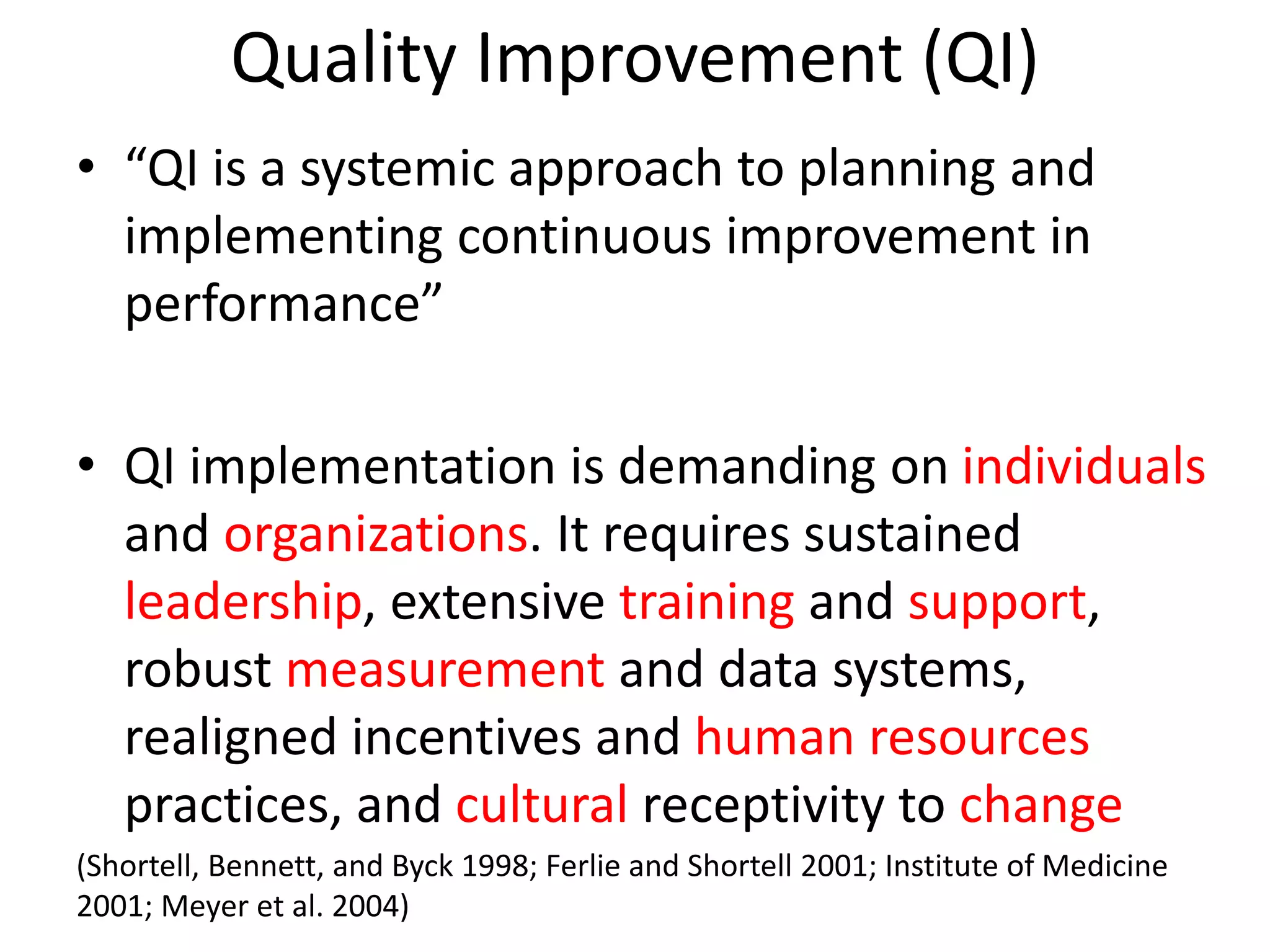
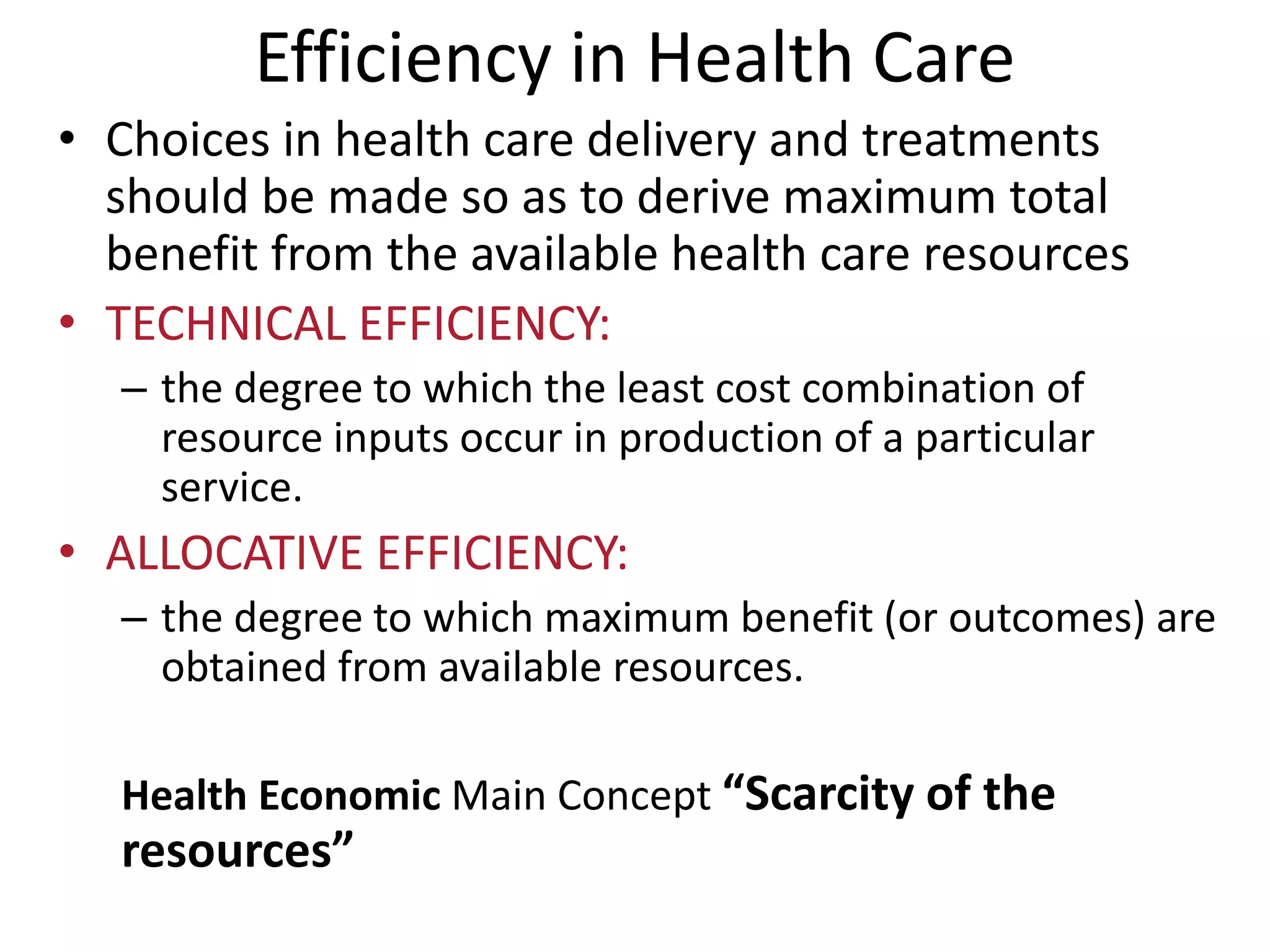
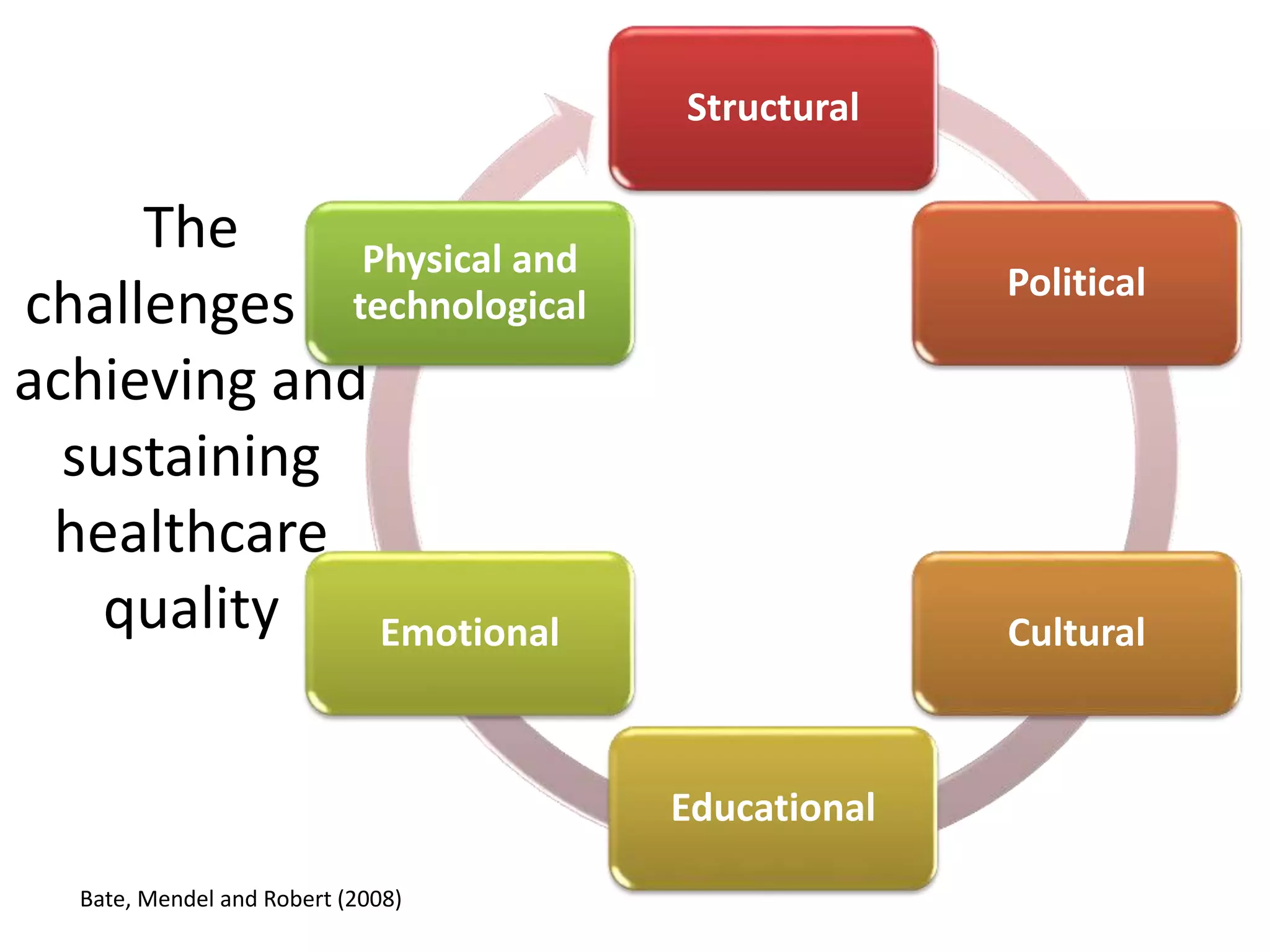
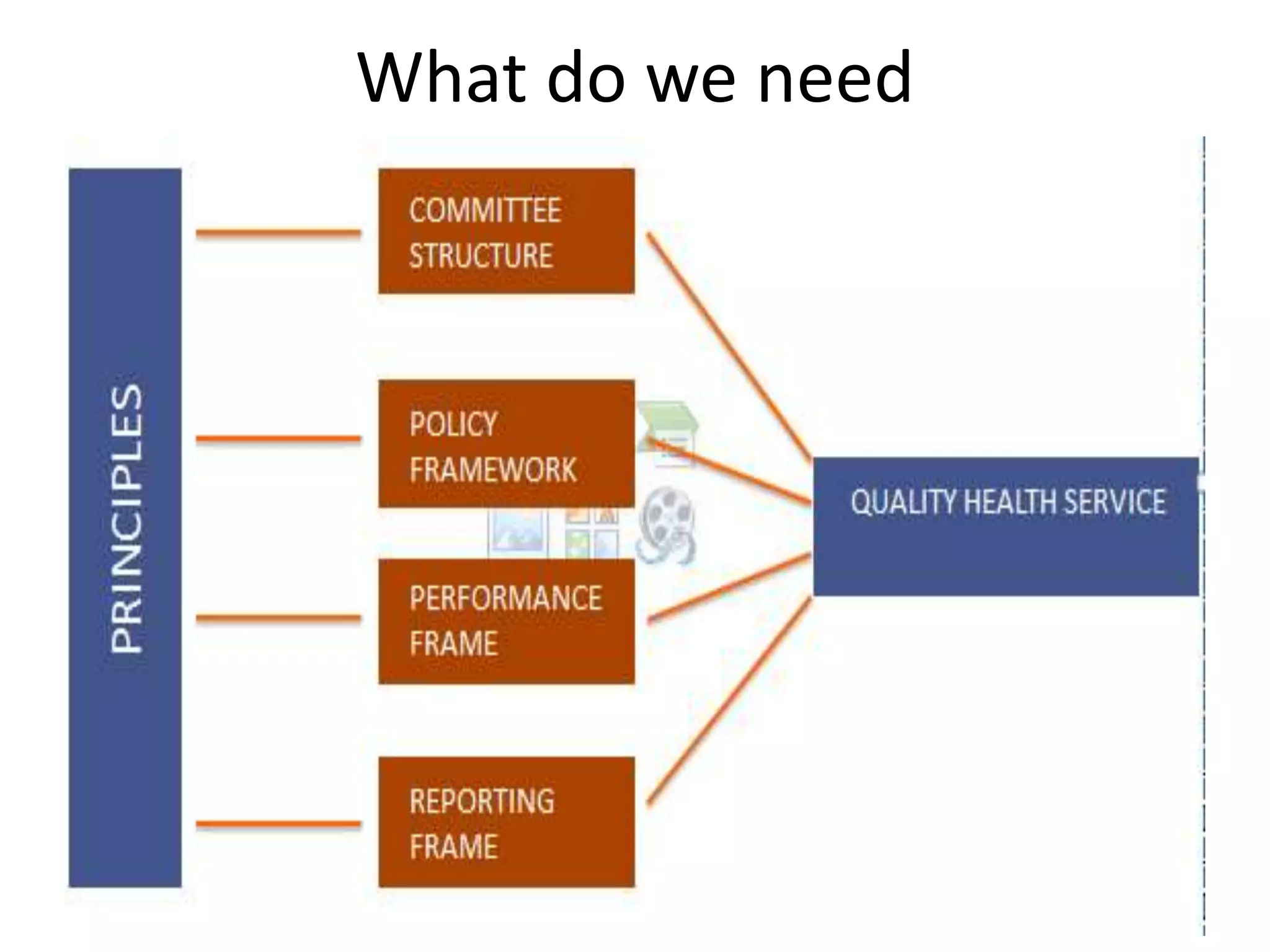
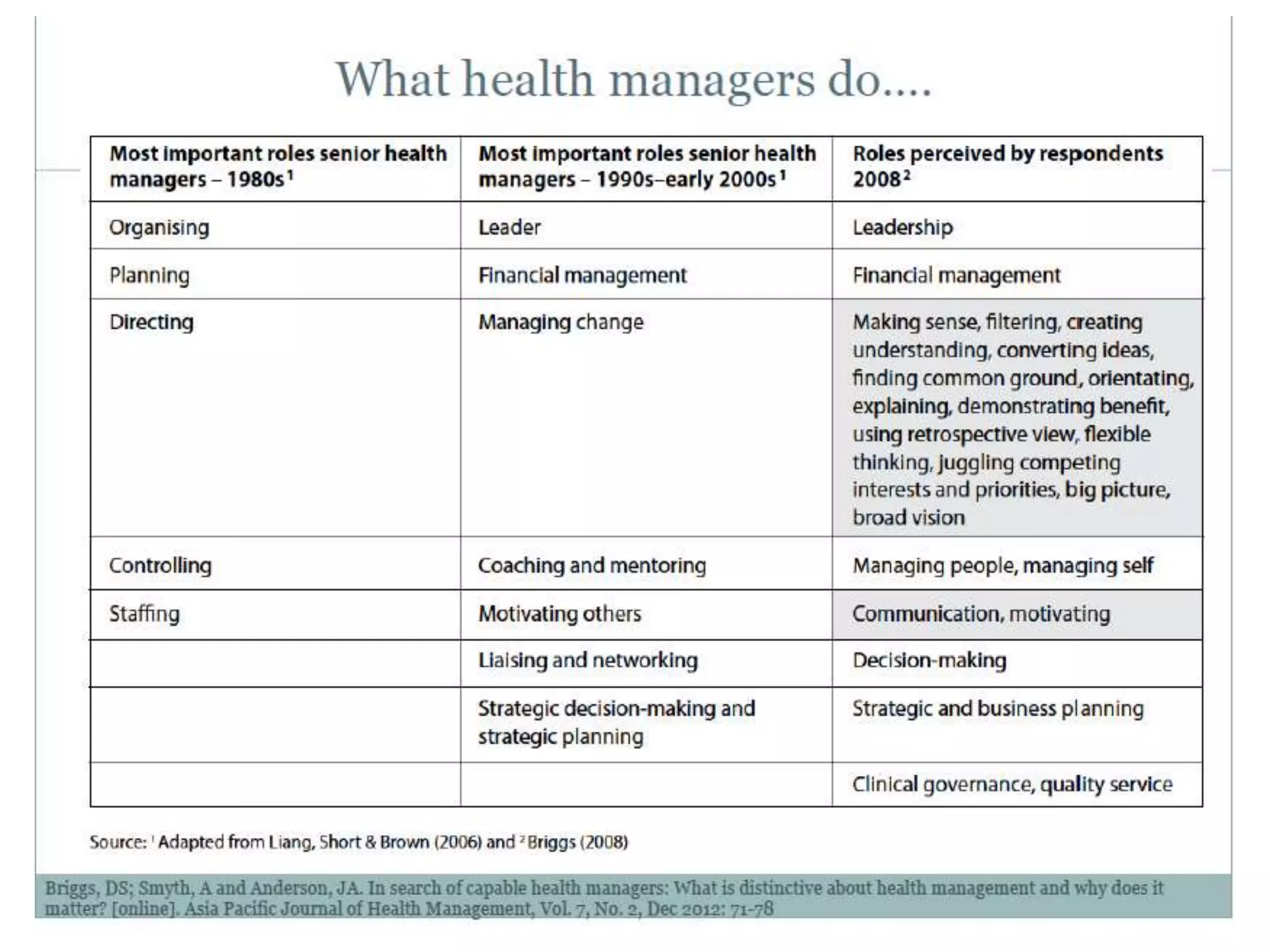
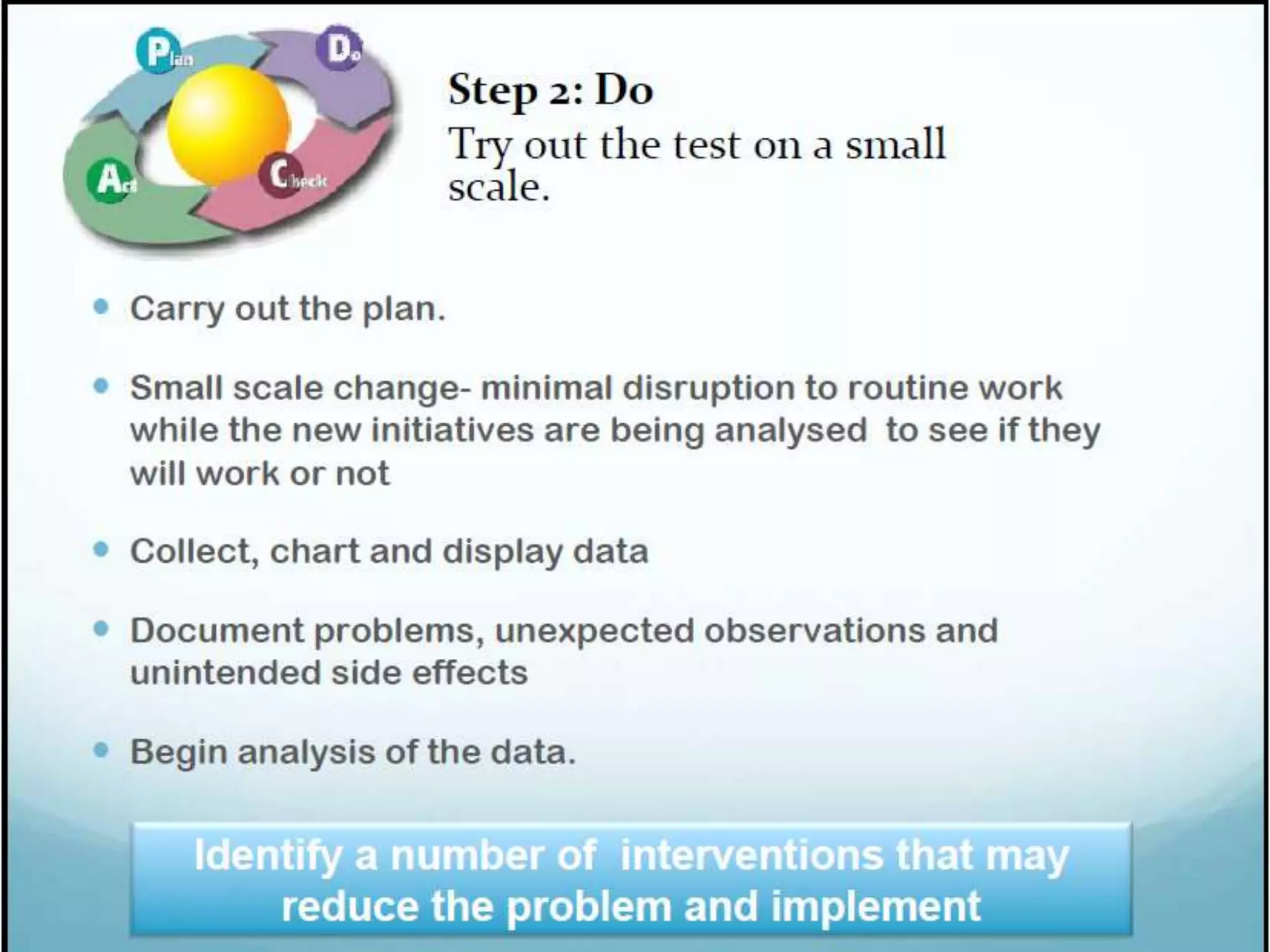
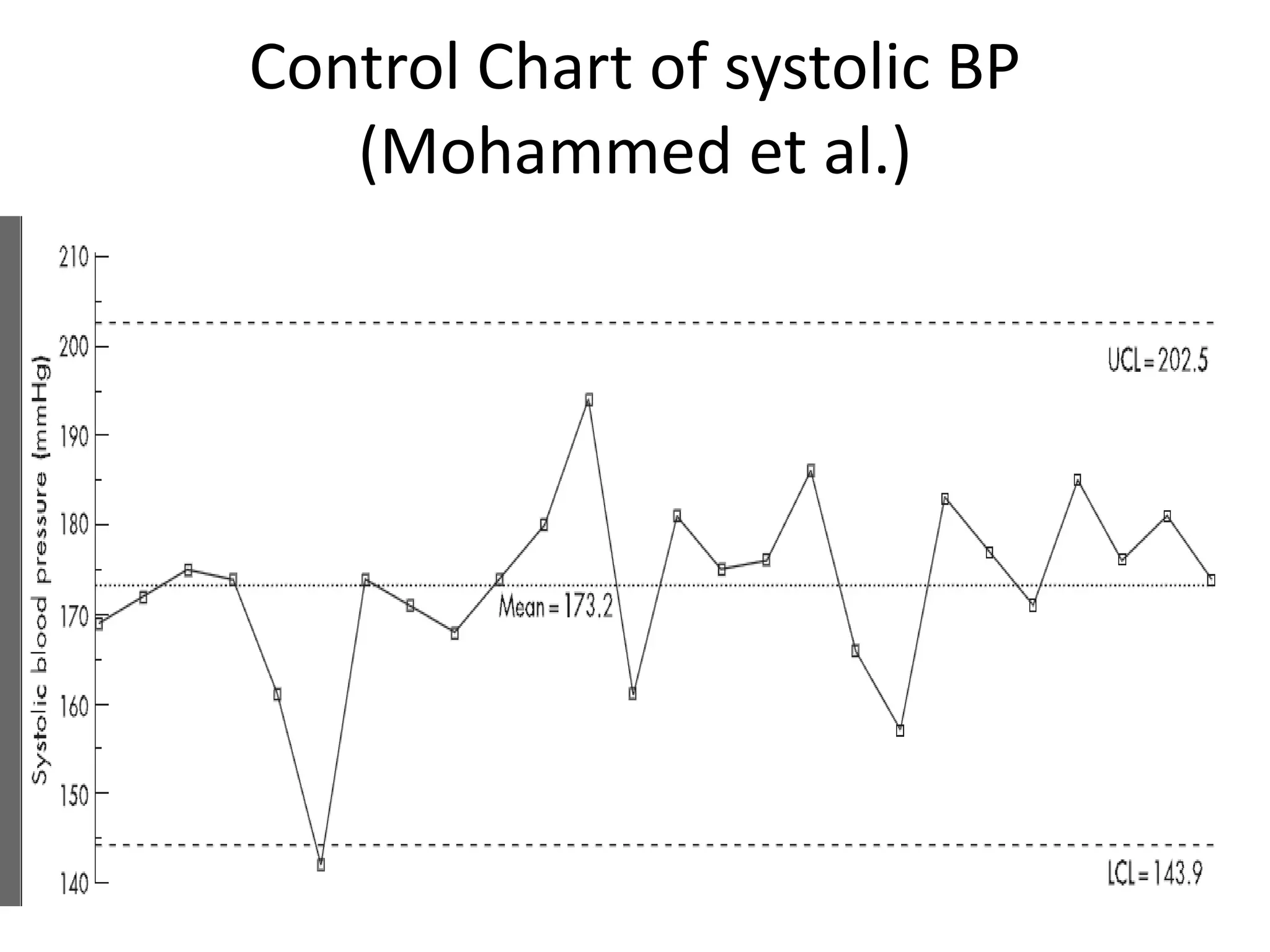
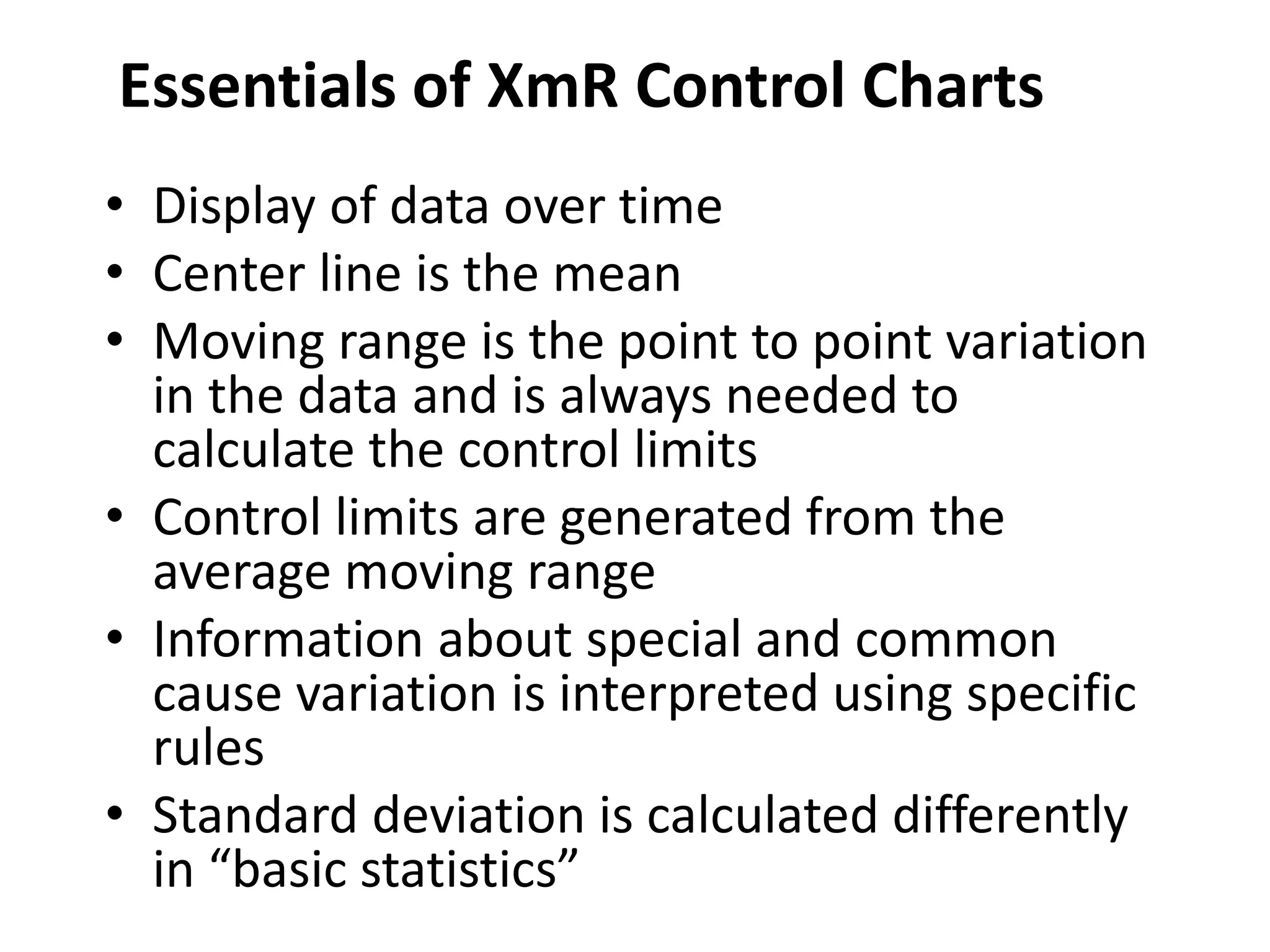
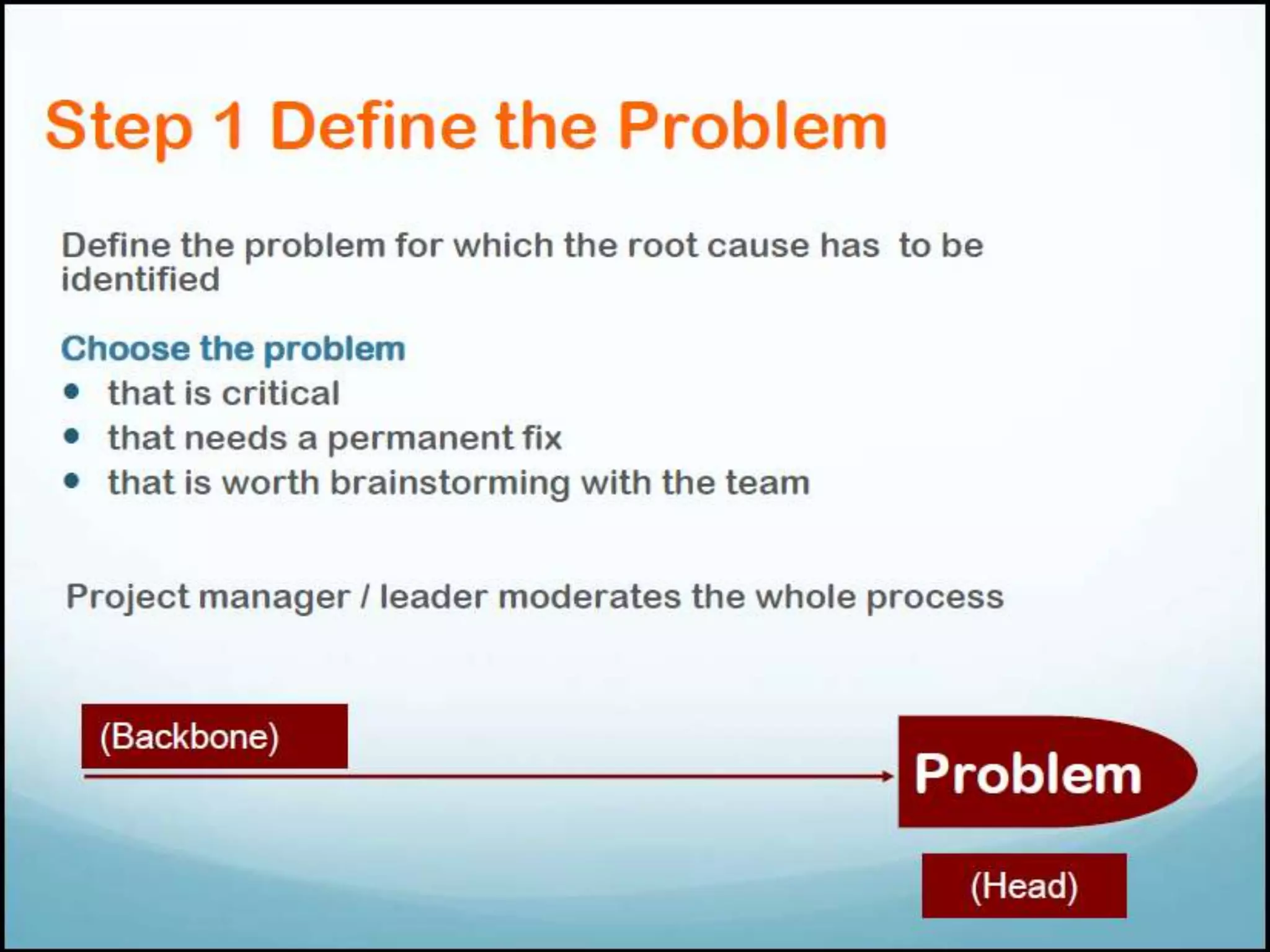
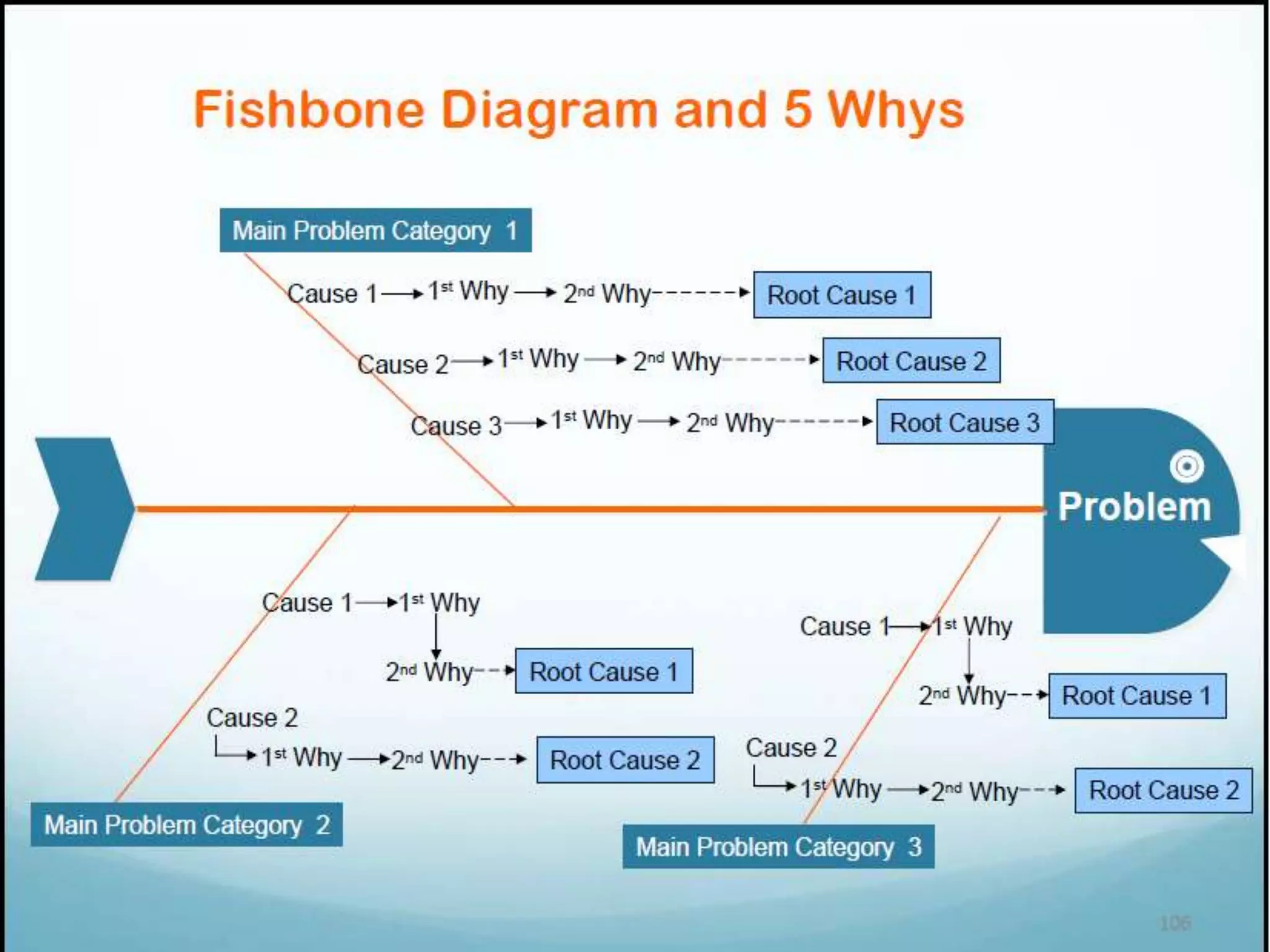
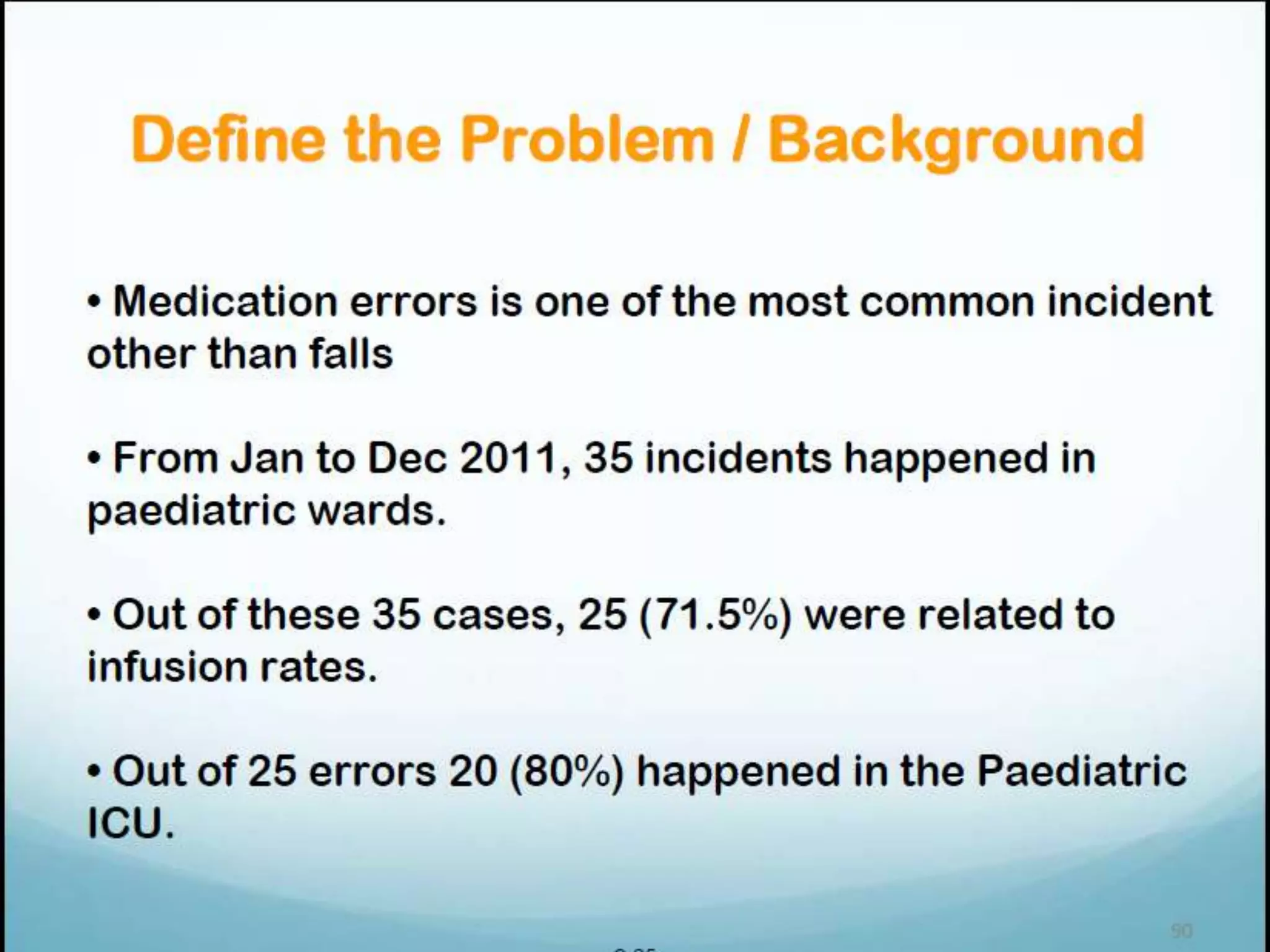
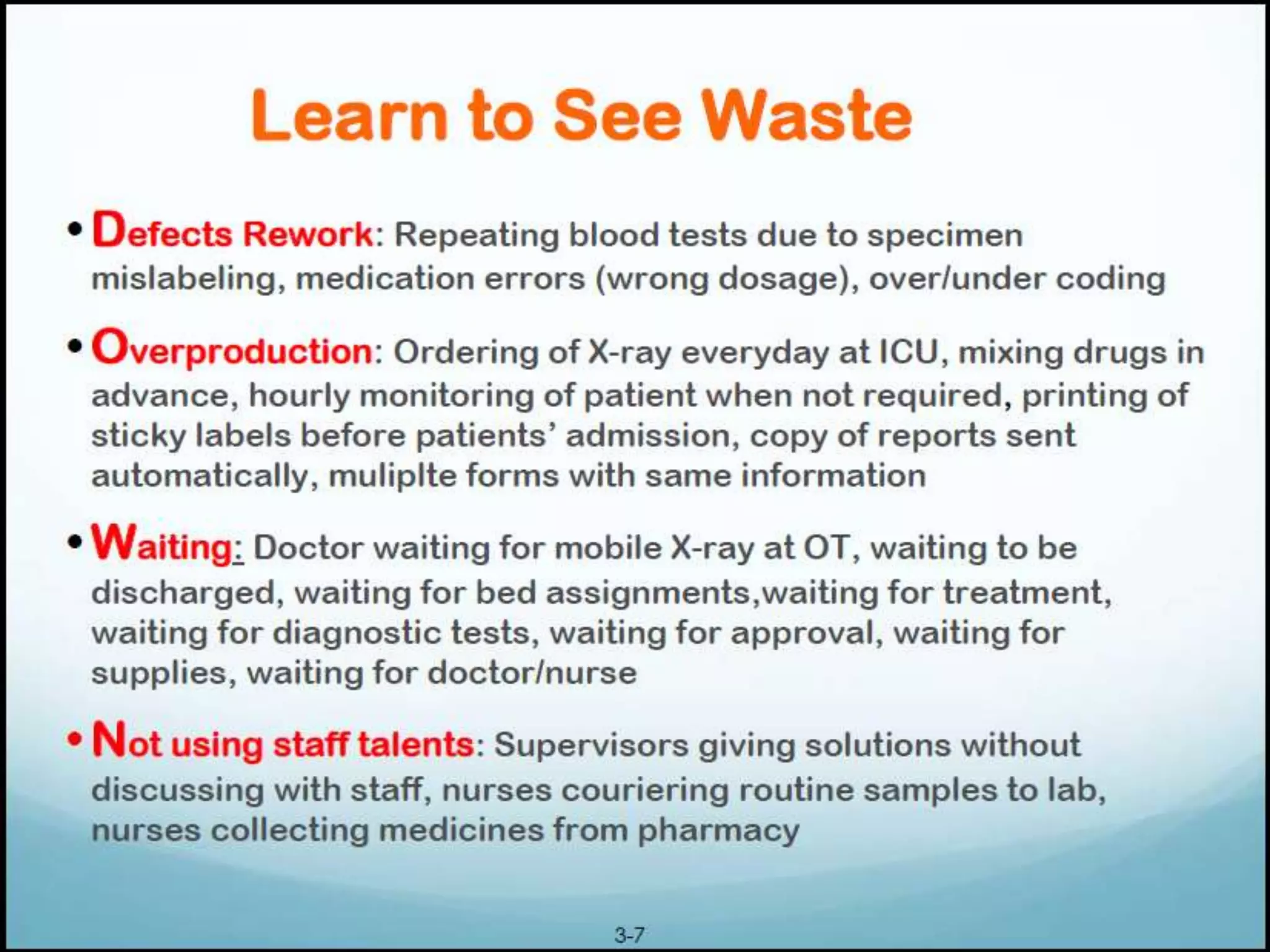
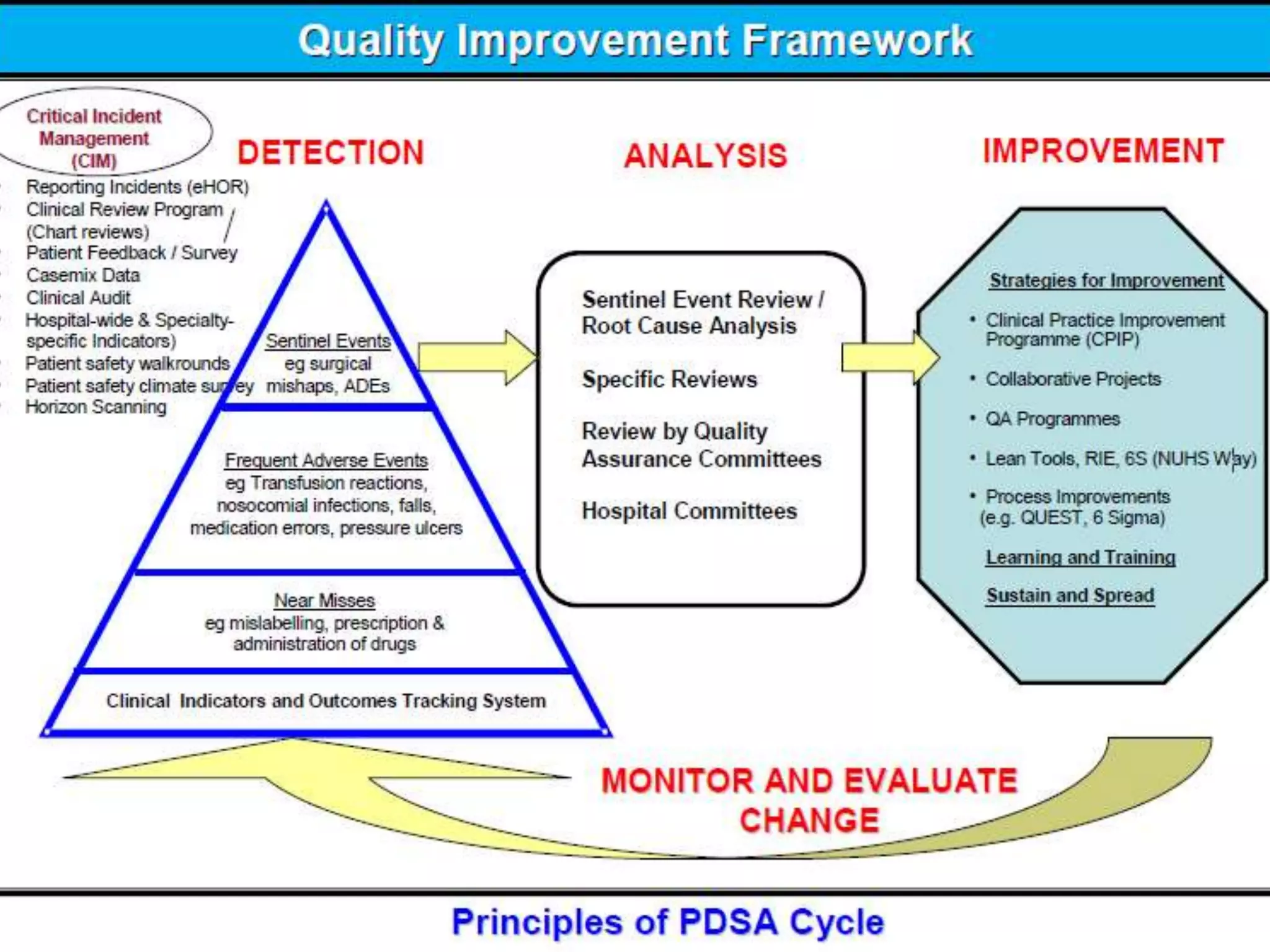
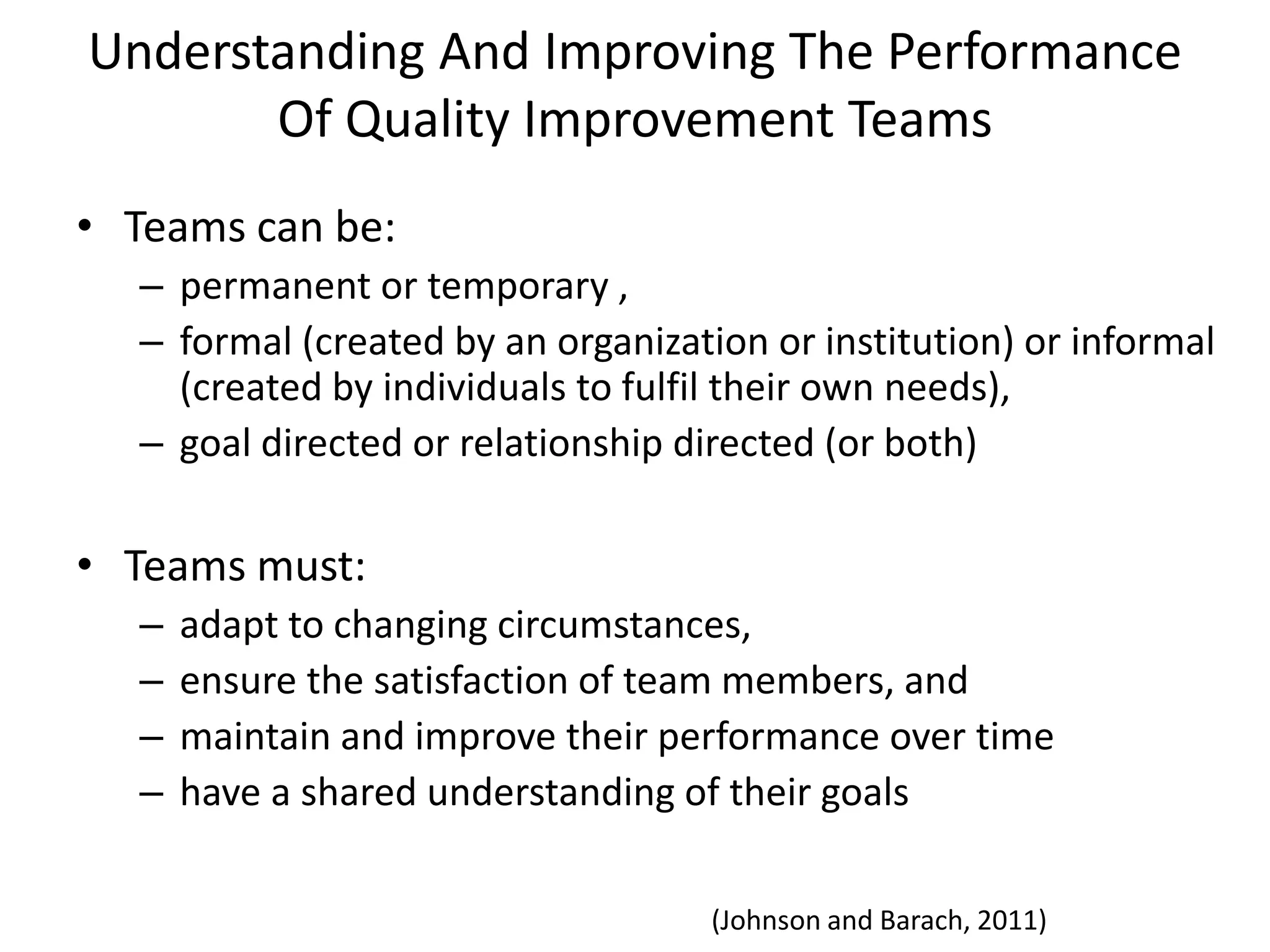
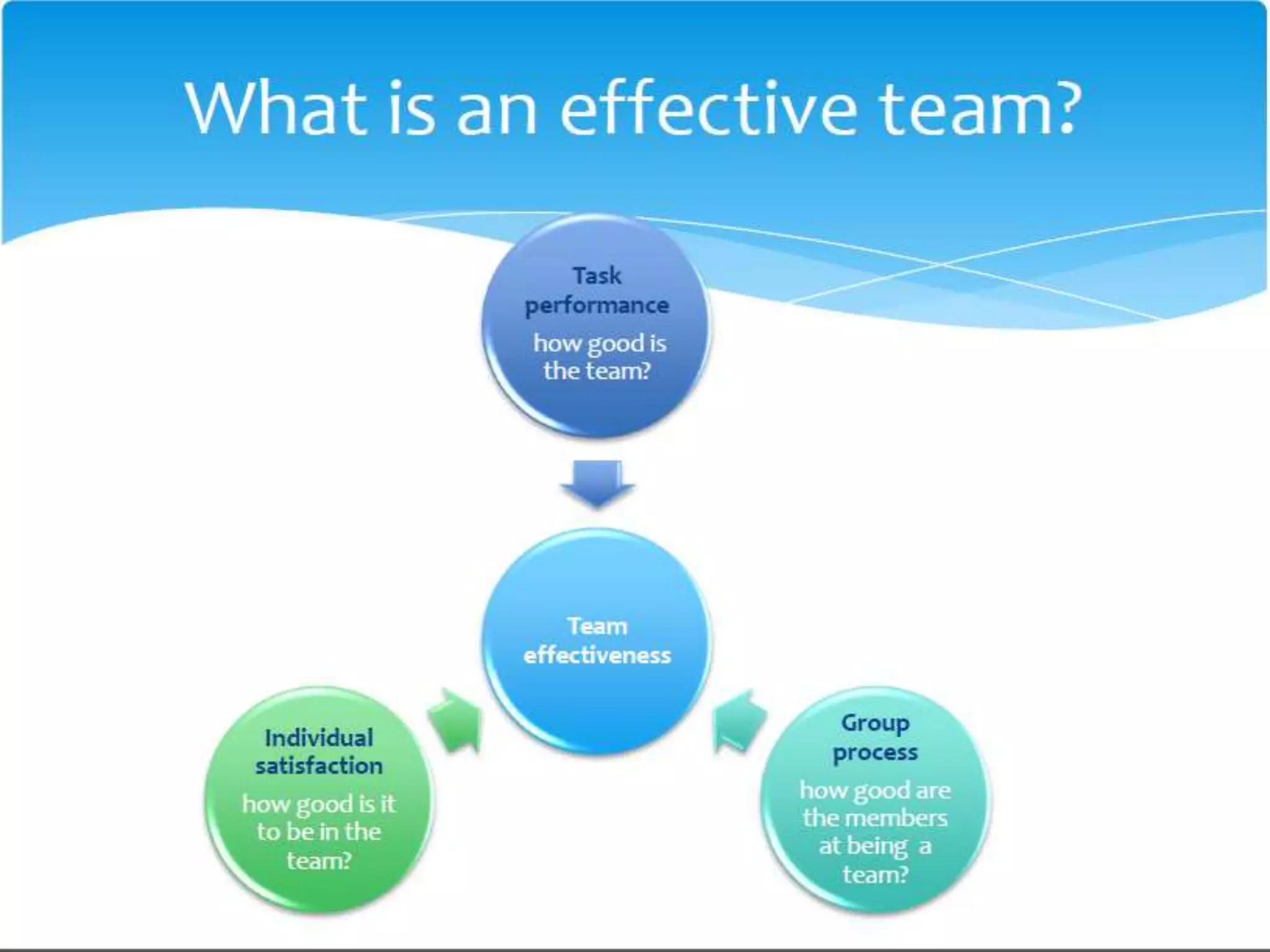
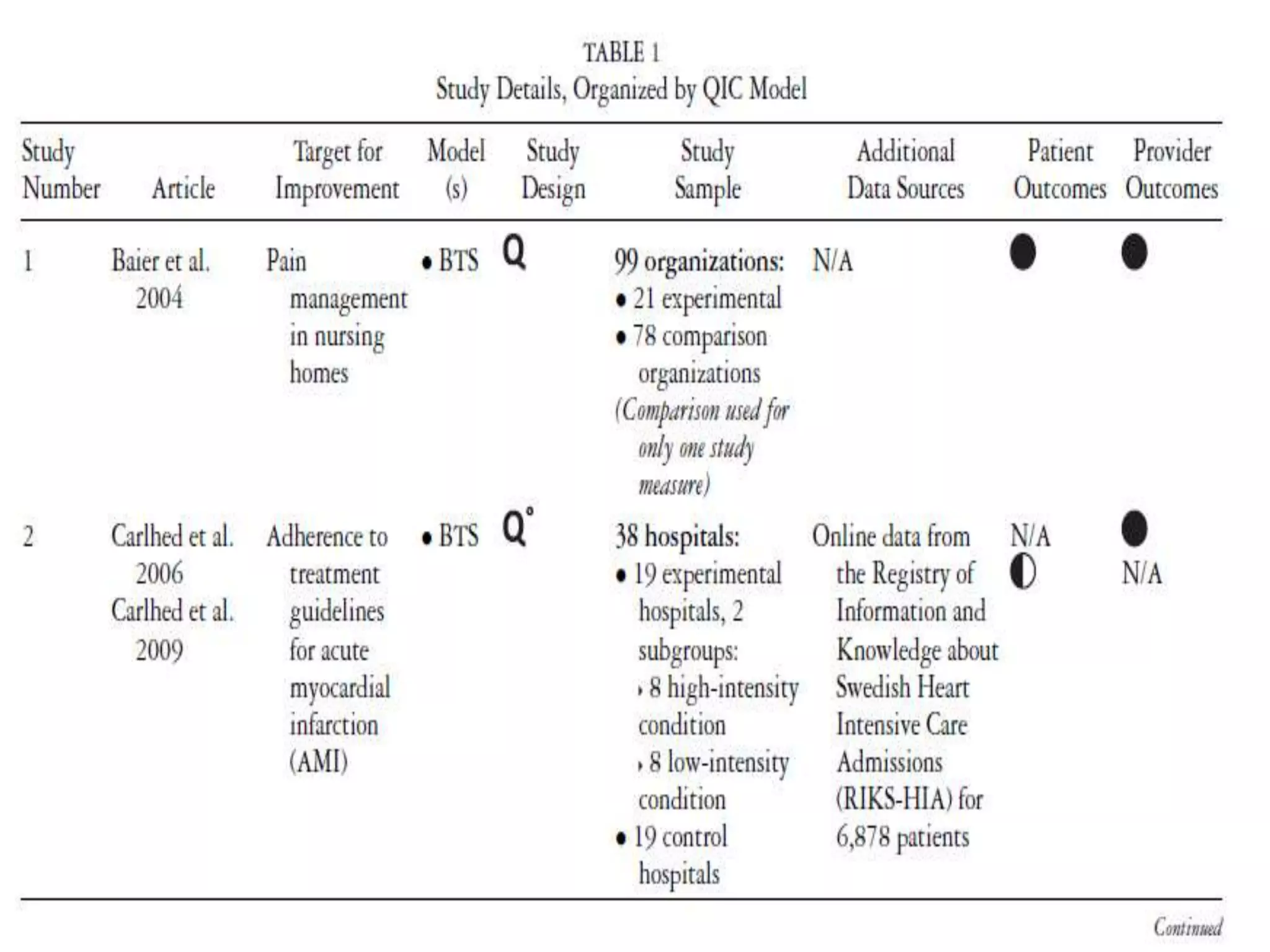
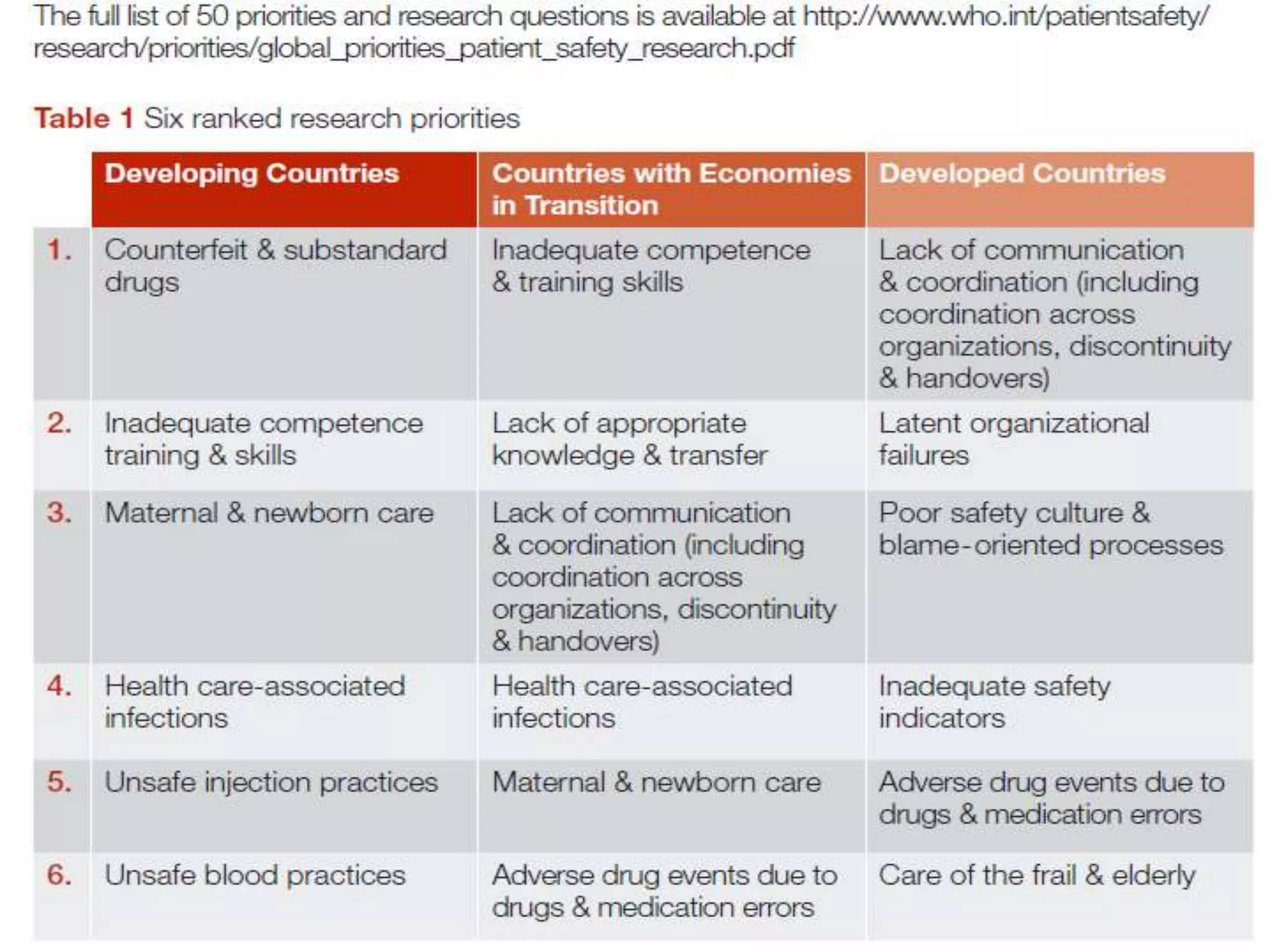
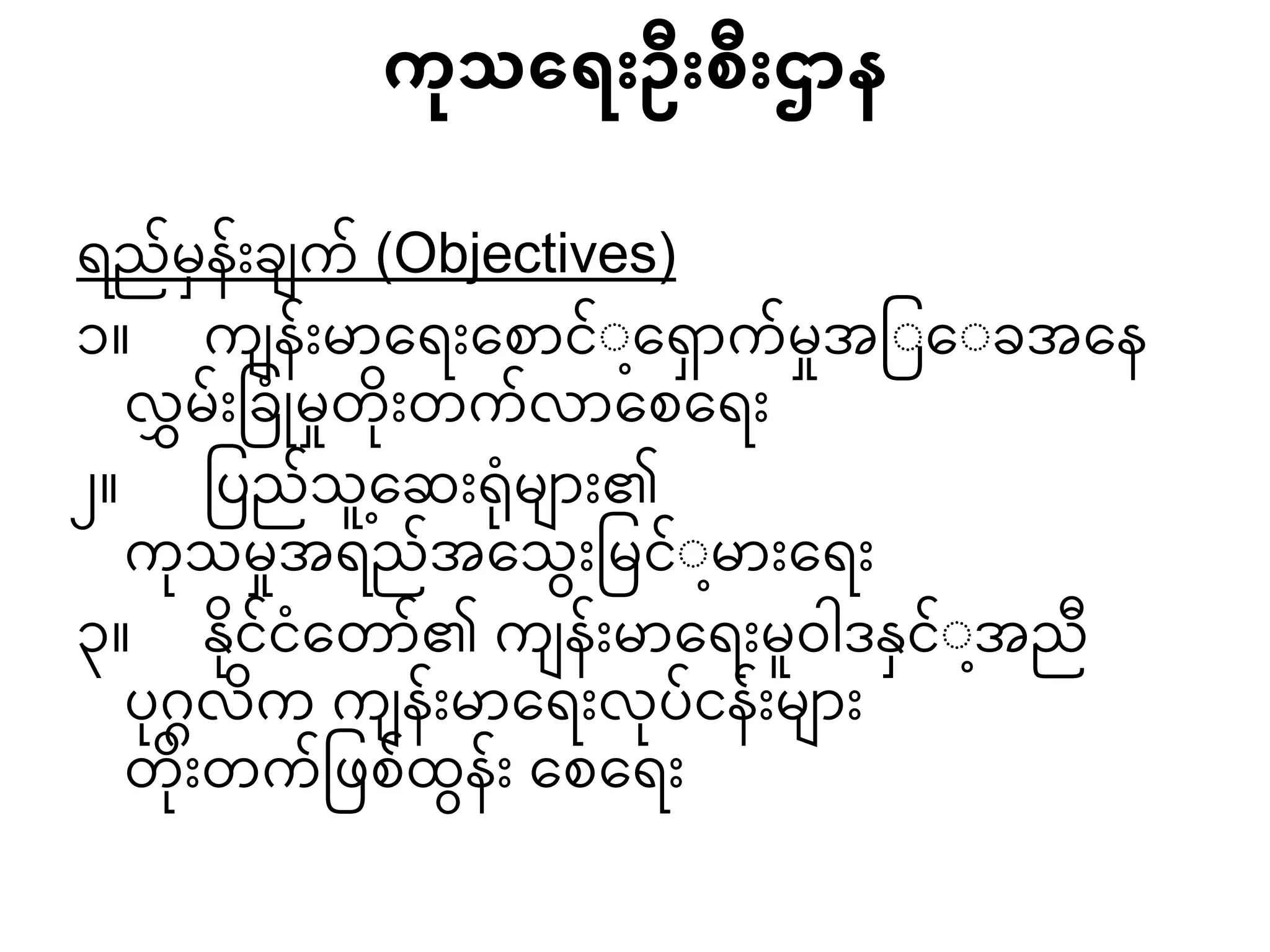
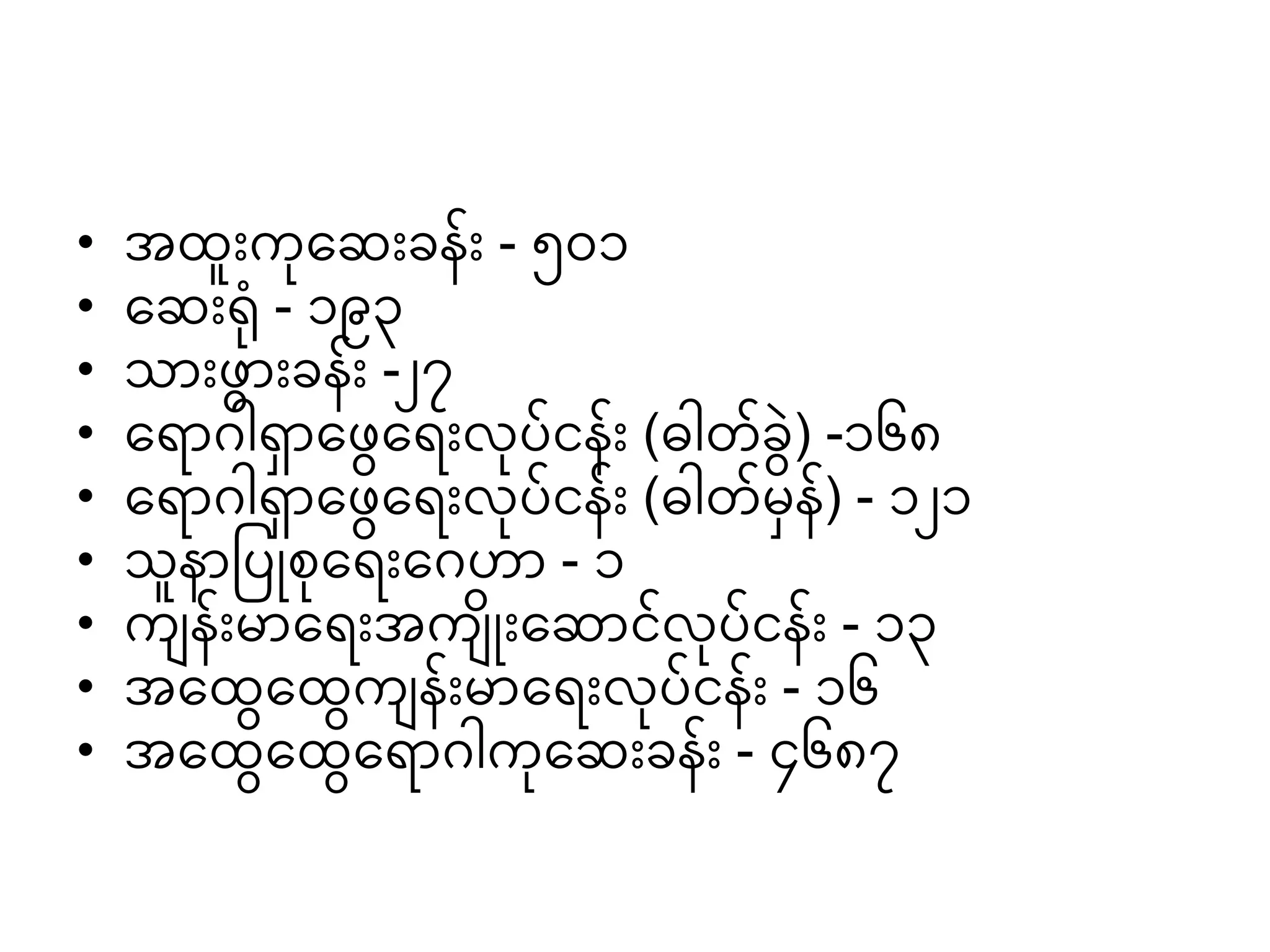
The document discusses quality improvement in hospitals. It notes that quality improvement (QI) requires sustained leadership, extensive training, robust measurement systems, and a culture receptive to change. It outlines six dimensions of healthcare quality: safety, effectiveness, appropriateness, access, patient satisfaction, and efficiency. Efficiency in healthcare involves deriving maximum benefit from available resources through technical and allocative efficiency. Common causes of medical errors include communication problems, inadequate information flow, human factors, and organizational issues. Many methods can be used to detect adverse events, both passive and active surveillance. Improvement starts with identifying an area for improvement through asking questions. Models for quality improvement include PDCA, Lean, Six Sigma, and change management. Measurement is key to