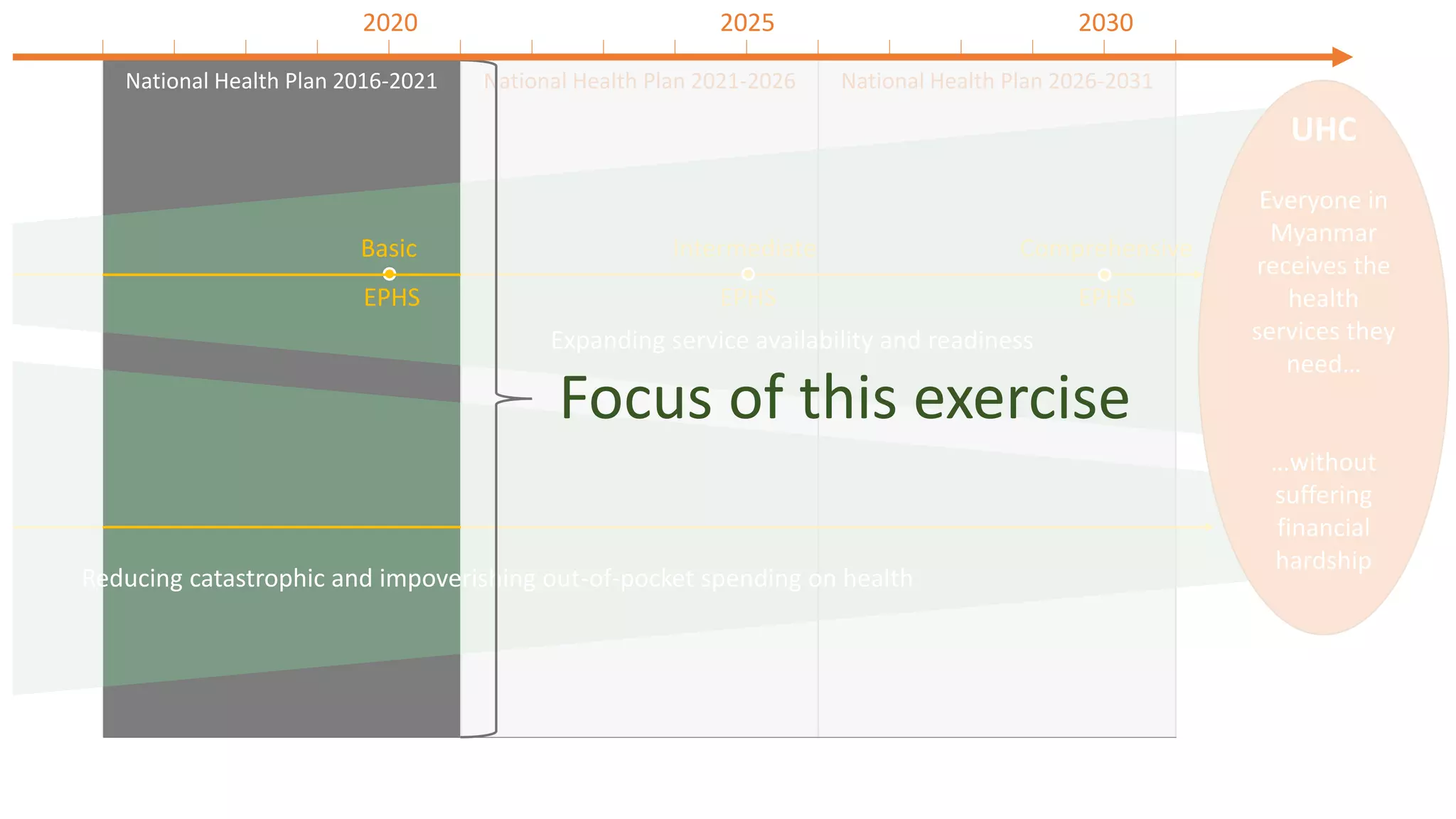
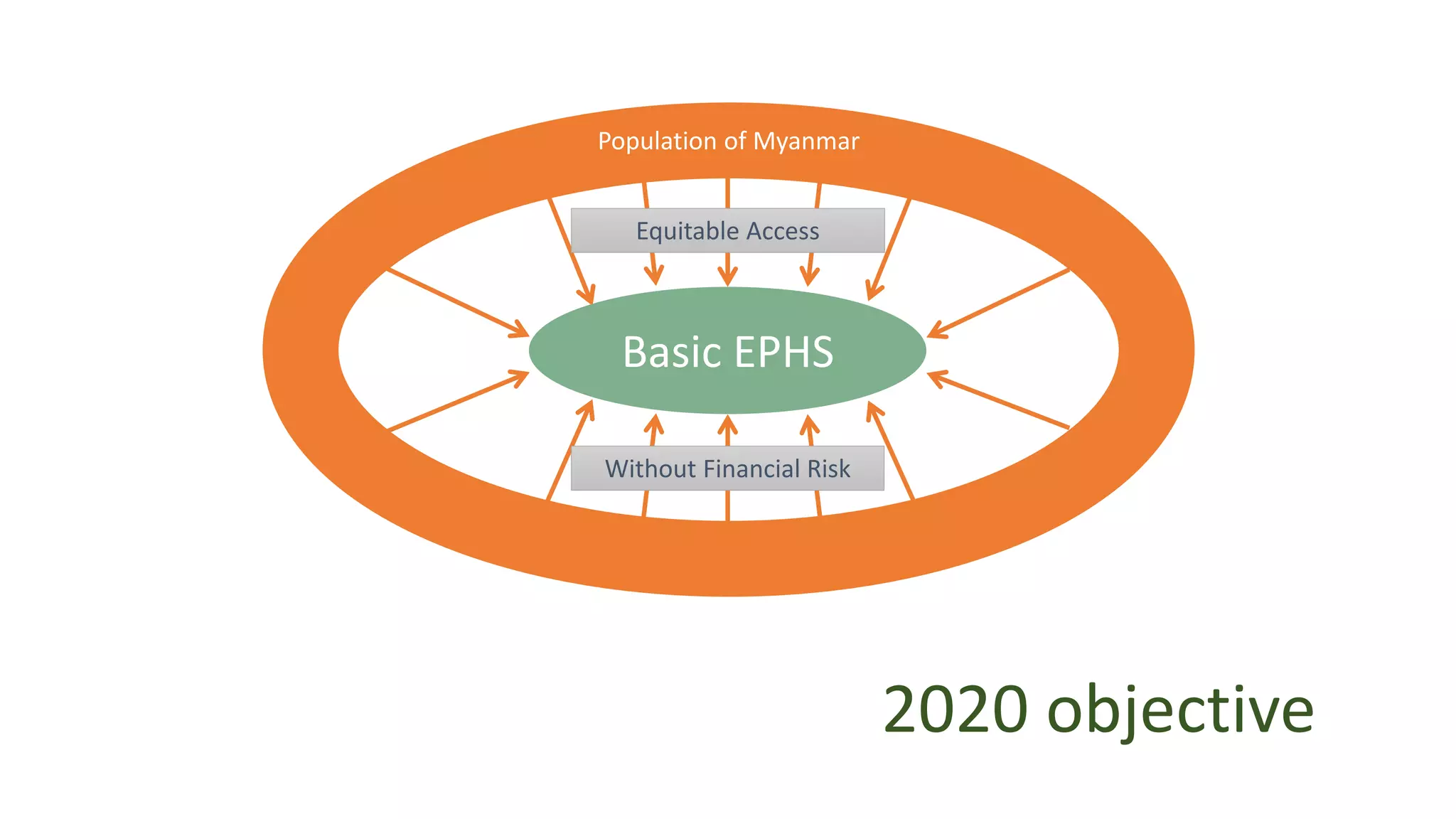
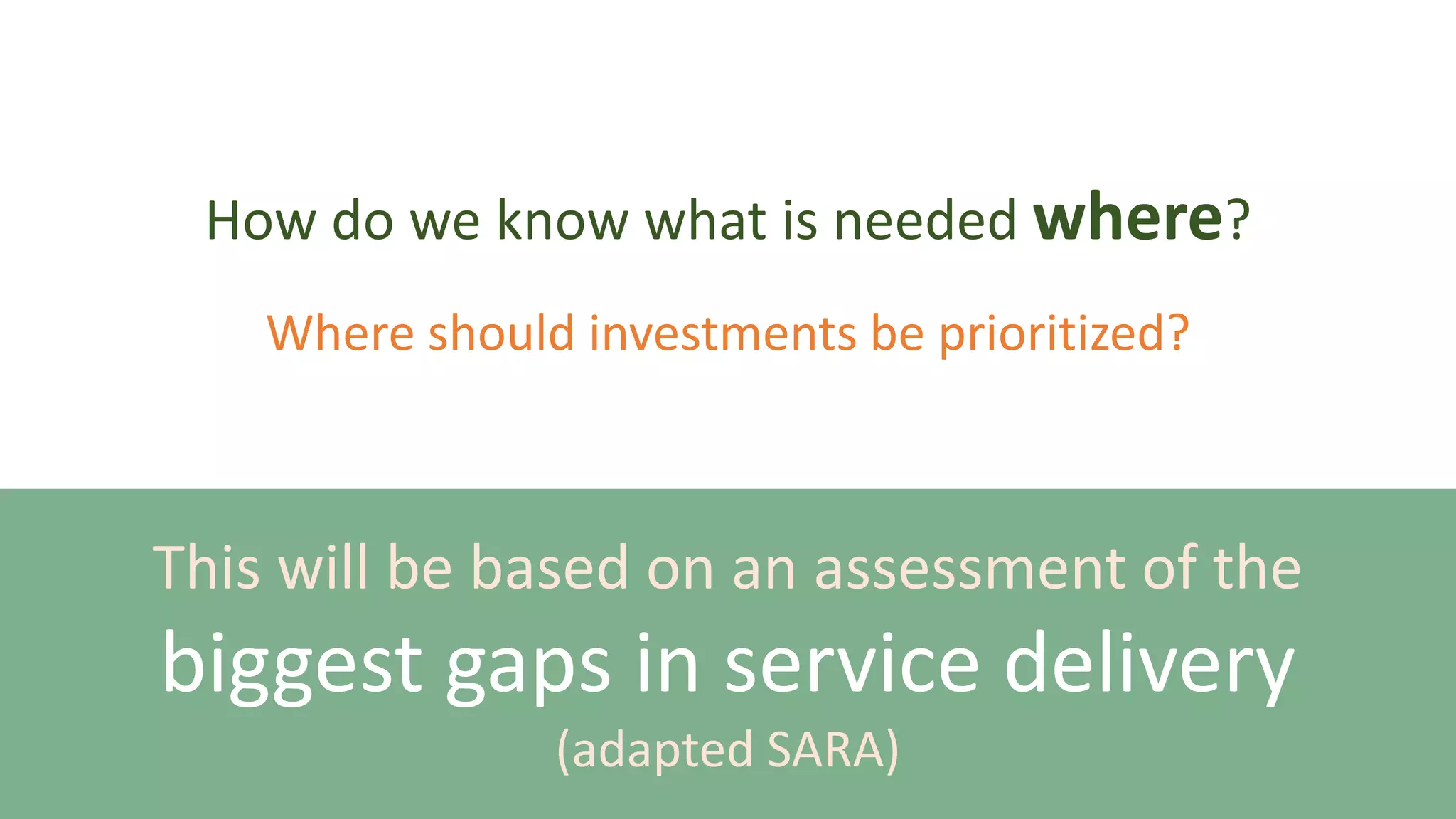
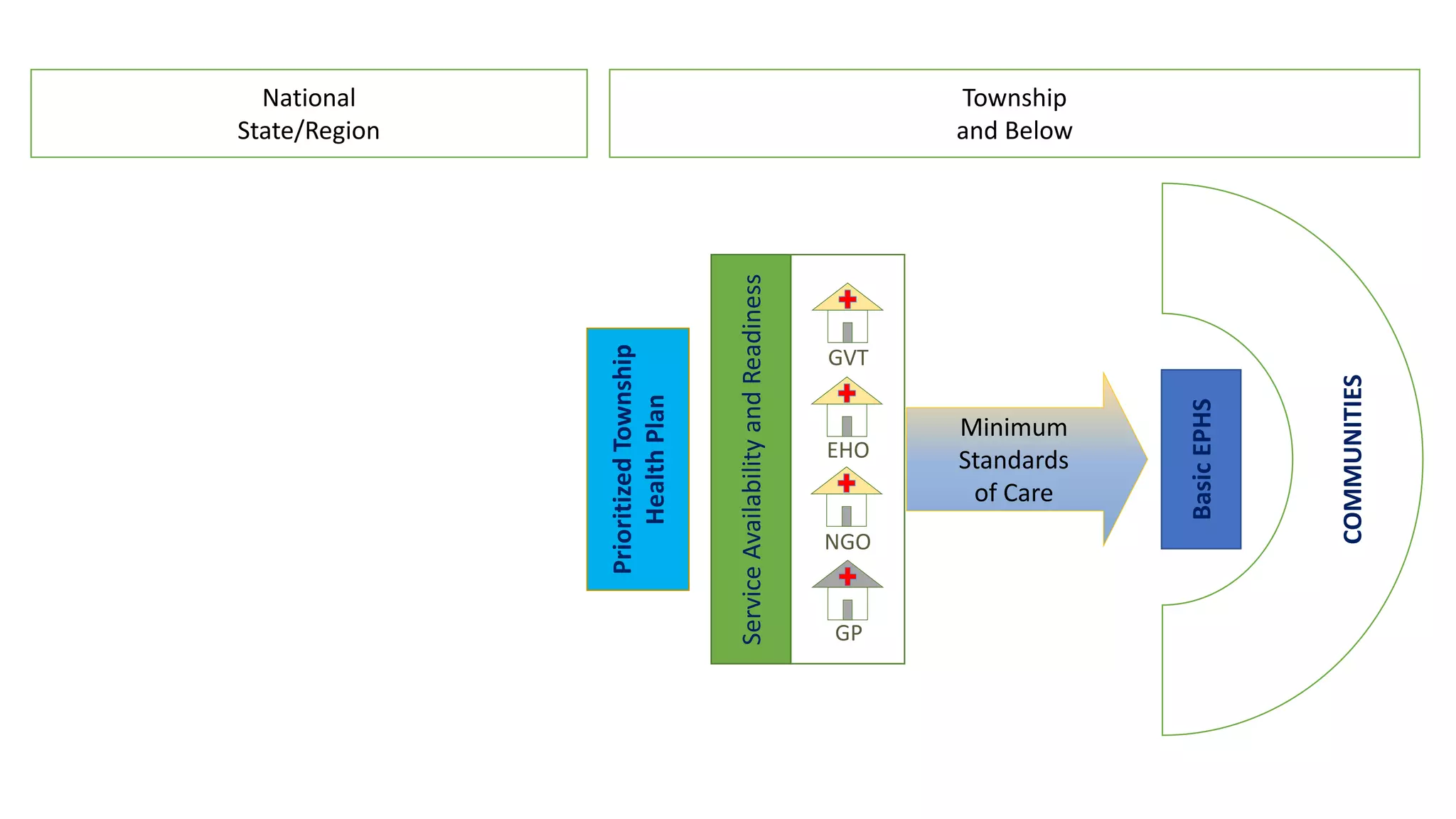
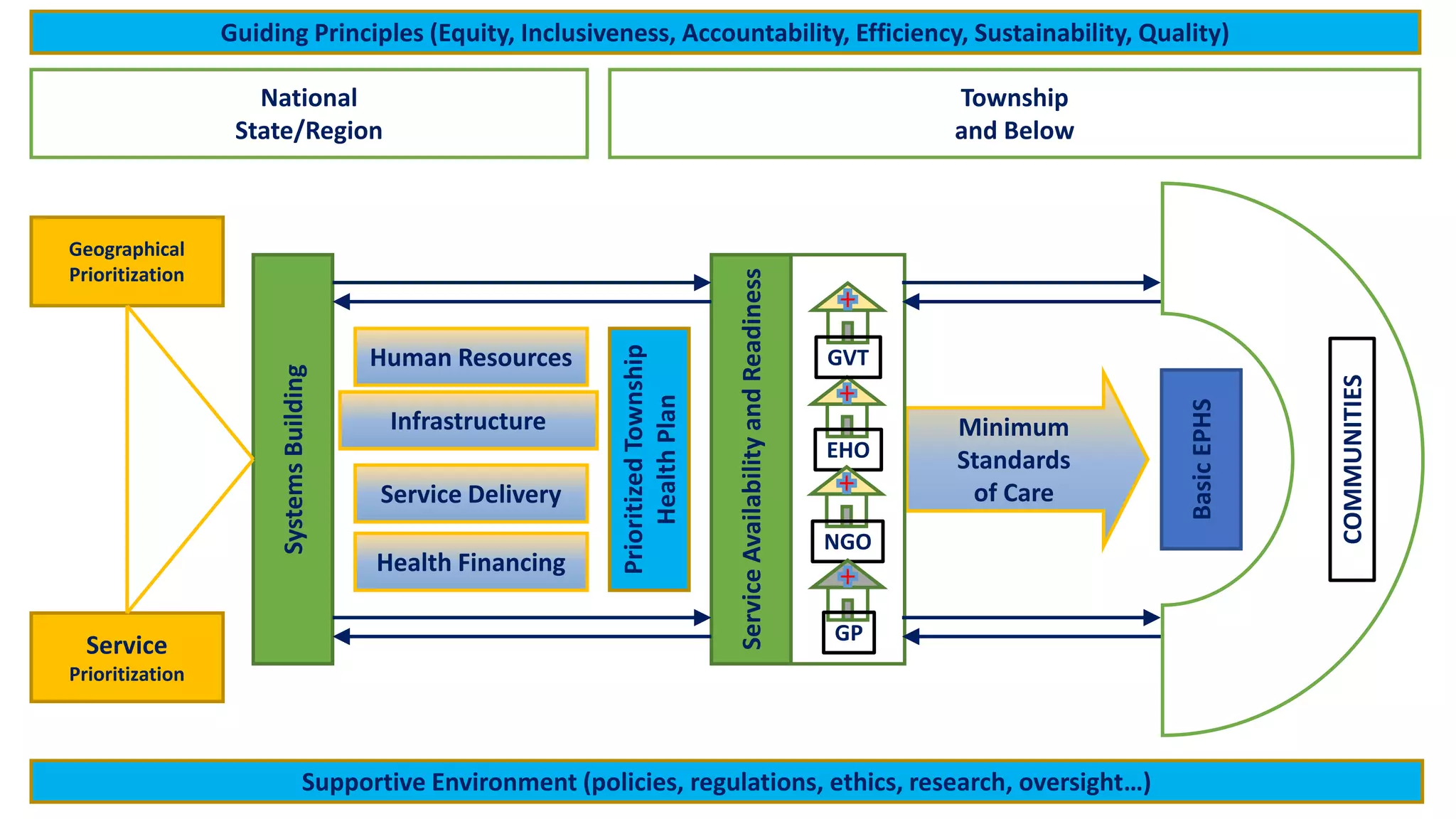
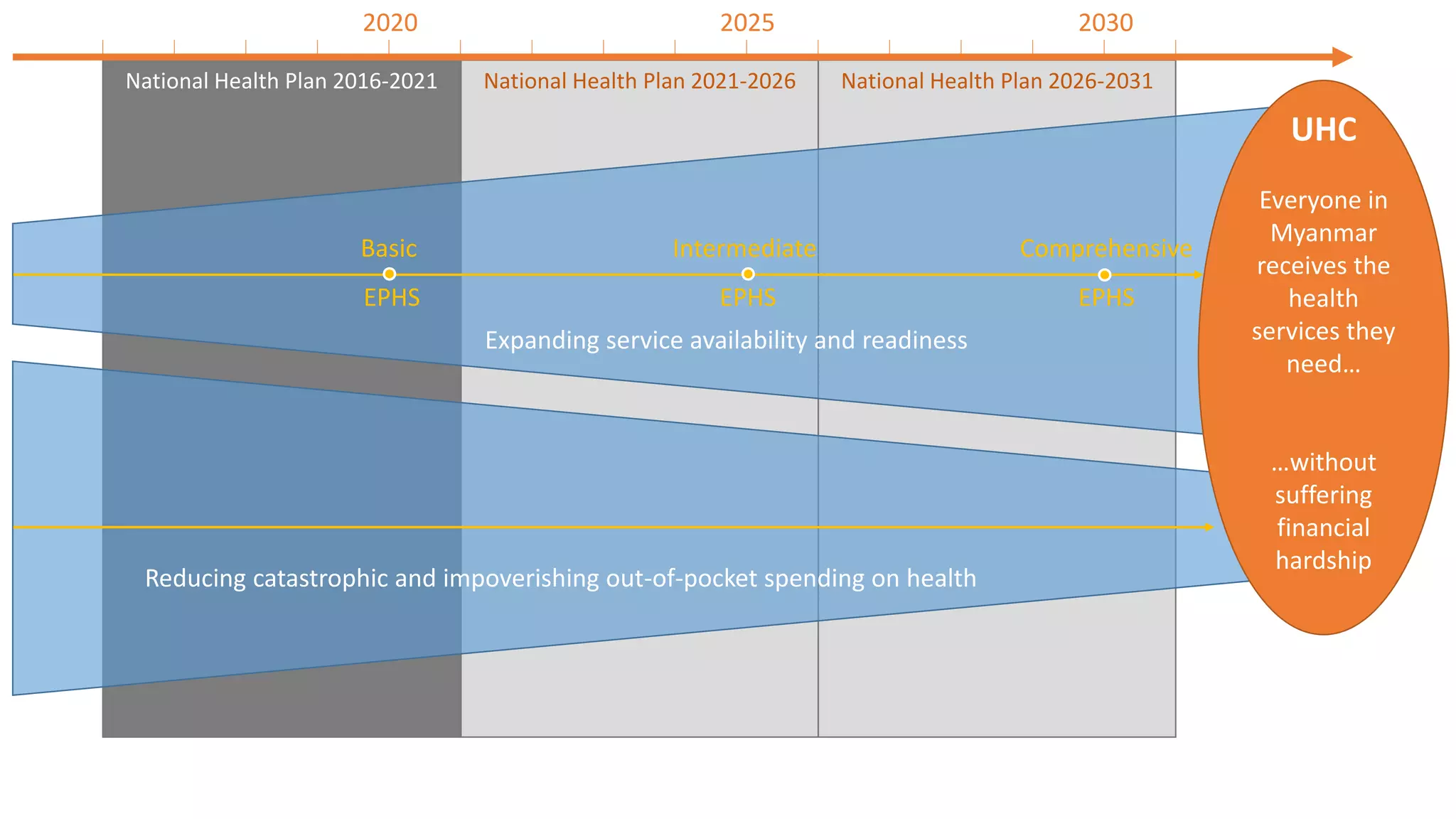
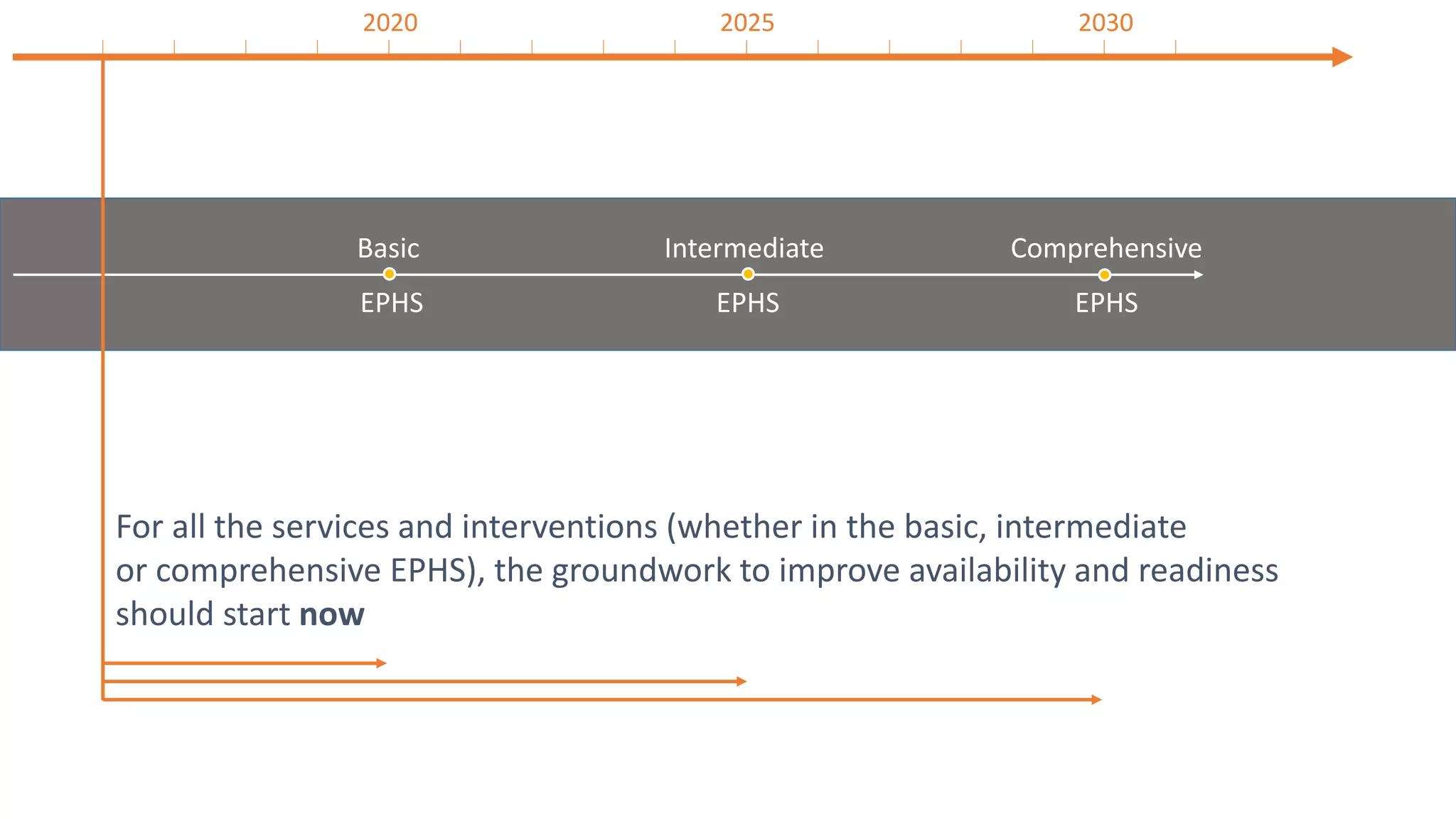
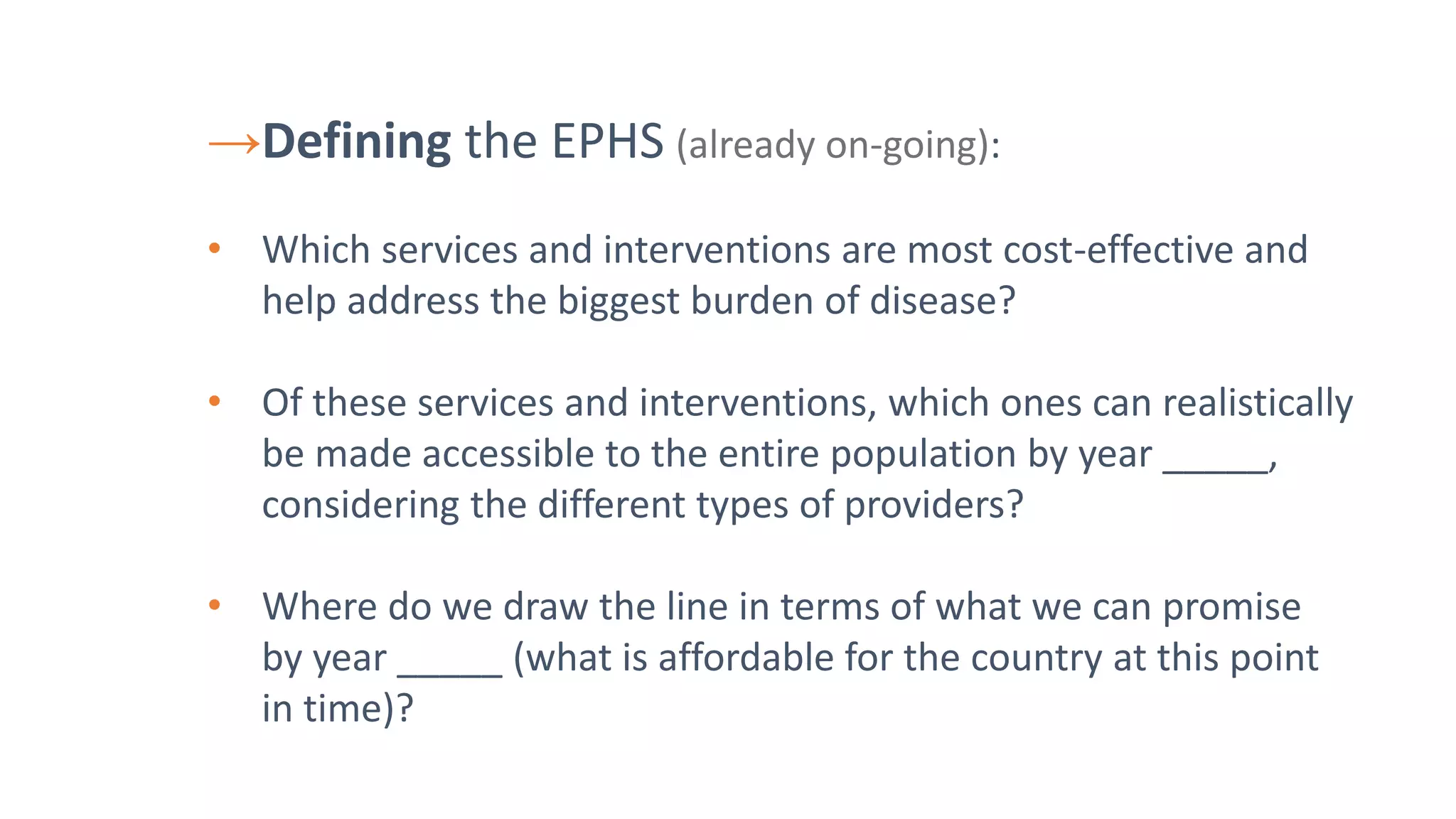
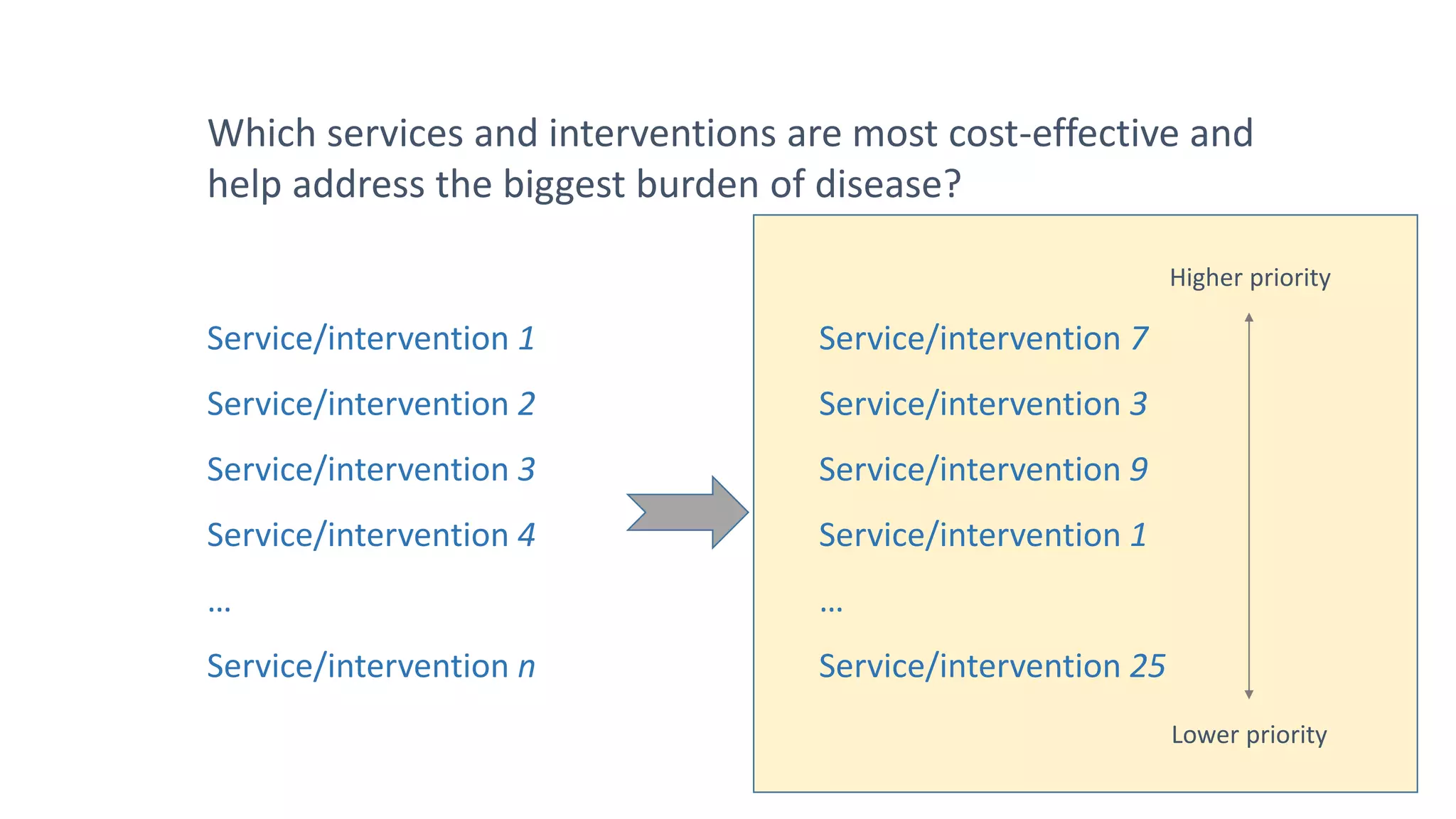
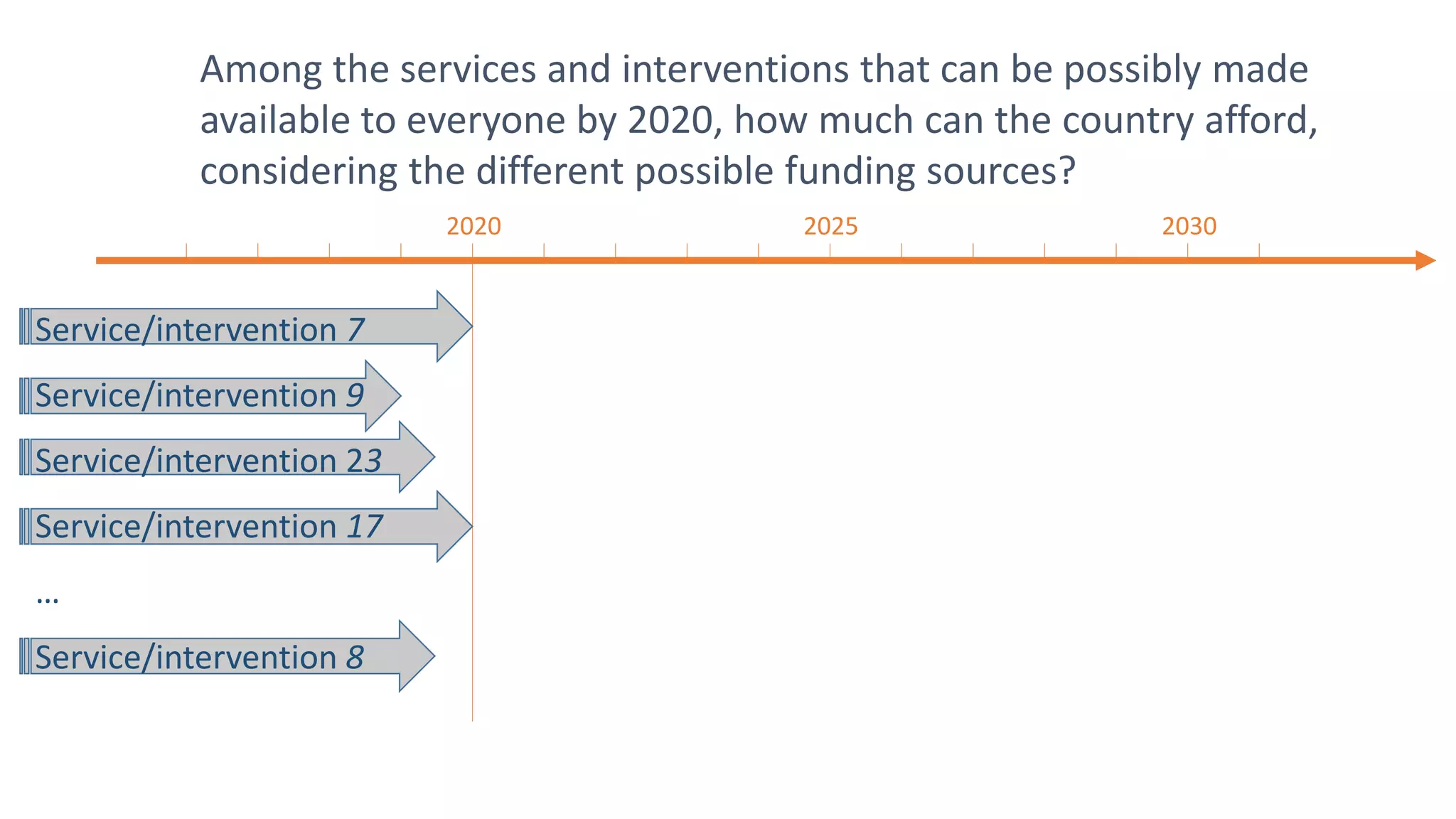
The document discusses the importance of defining an essential package of health services (EPHS) for a country with limited resources. The EPHS should include the most cost-effective interventions that address the largest disease burden and can realistically be made available to the entire population by a target year, while staying within the country's budget constraints. Over time, the EPHS will expand from a basic to an intermediate to a comprehensive package as availability and affordability increase. National health plans should focus on expanding service availability, reducing out-of-pocket costs, and achieving universal health coverage through successive EPHS.



![Why an Essential Package of Health Services?
• To ensure the limited resources are spent wisely
• To improve equity
Not having a package is like an empty promise
[it implies that everything should be available,
while we very well know that is not possible]](https://image.slidesharecdn.com/ephsandnhp-170626083352/75/Ephs-and-nhp-4-2048.jpg)
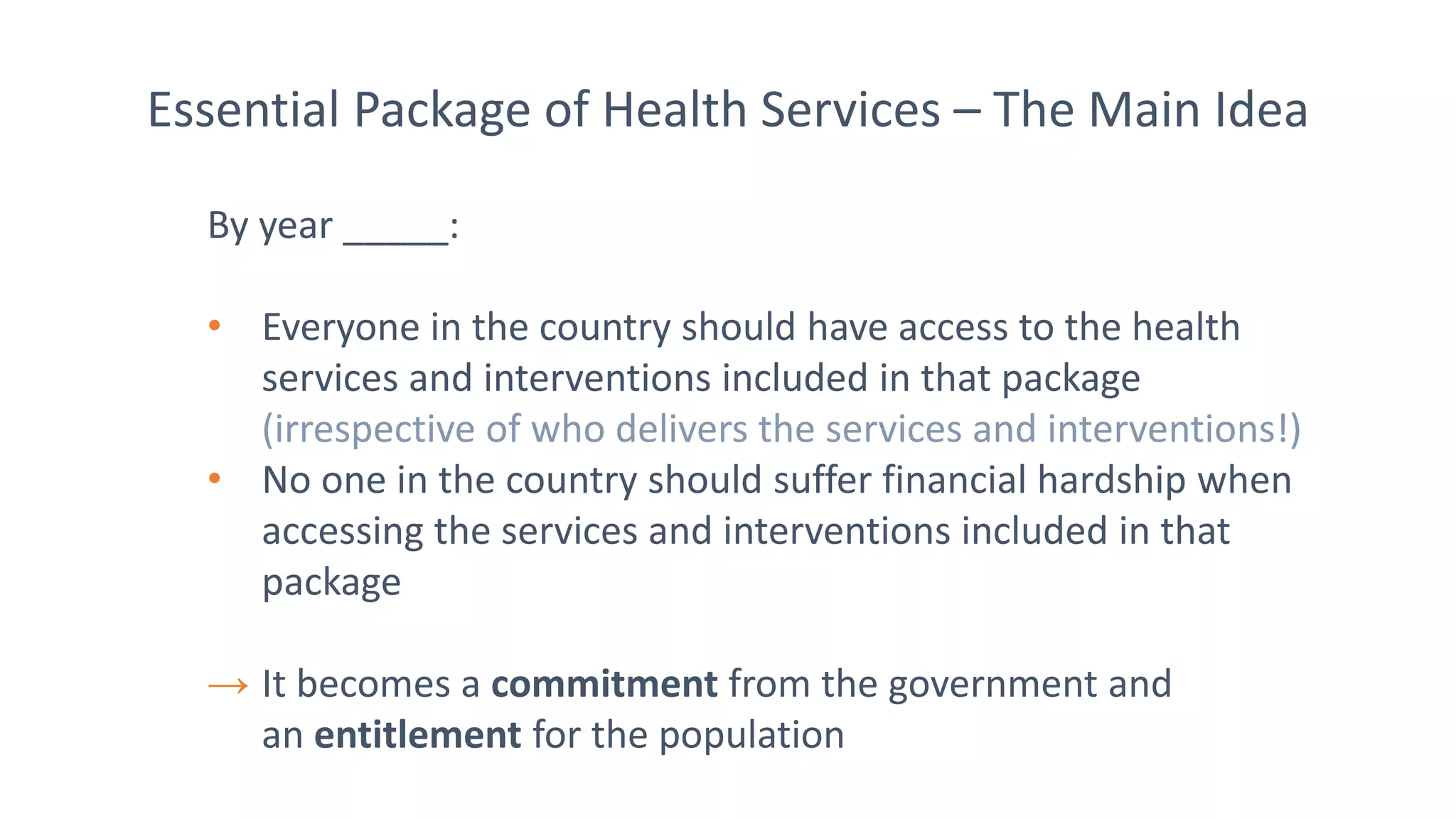
![Essential Package of Health Services – The Main Idea
→ The EPHS should be:
• Effective – it should include services and interventions that will
result in the greatest improvements in population health
• Realistic – it should include services and interventions for which
access can be guaranteed for everyone by year _____
[irrespective of who delivers those services and interventions]
• Affordable – its should be affordable for the country, considering
(i) the different sources of funding and (ii) the condition that
no-one should suffer financial hardship when using the services
and interventions](https://image.slidesharecdn.com/ephsandnhp-170626083352/75/Ephs-and-nhp-6-2048.jpg)




![Key questions regarding the EPHS
• Who can deliver the services and interventions?
[this will vary by service/intervention and by location]
• Where will the money come from?
• To ensure service availability and readiness
• To actually ‘purchase’ the services
These questions should be the focus of the National
Health Plan, not the actual content of the basic EPHS](https://image.slidesharecdn.com/ephsandnhp-170626083352/75/Ephs-and-nhp-16-2048.jpg)