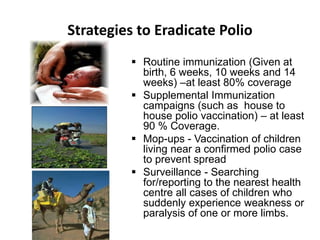
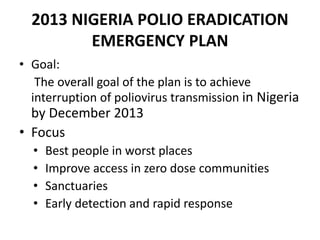
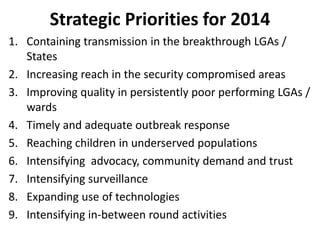
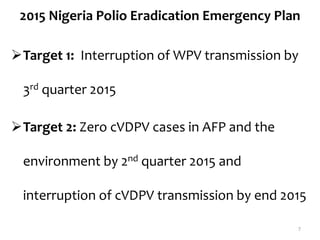
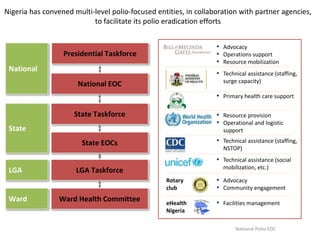
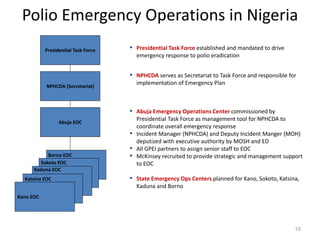
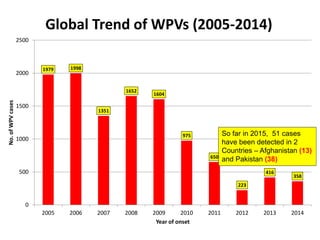
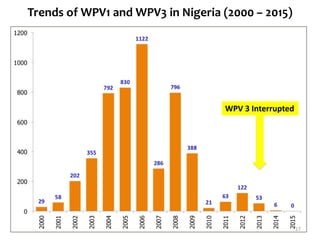
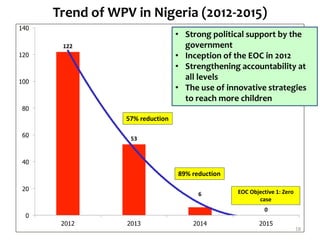
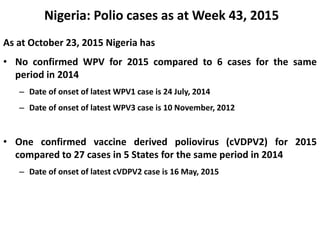
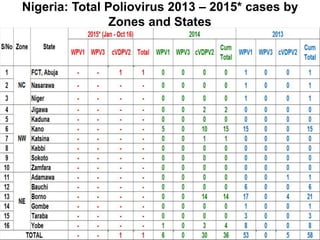
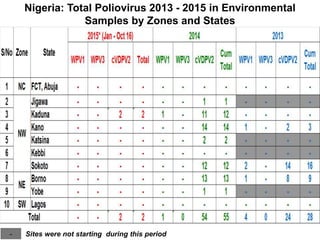
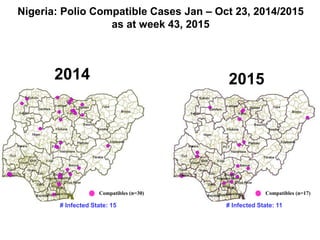
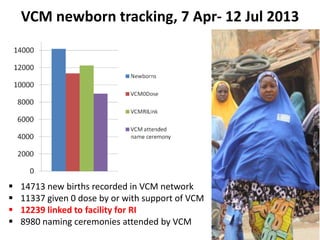
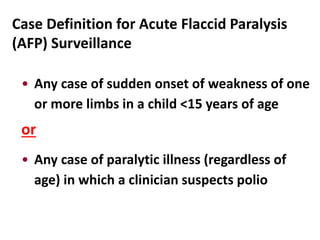
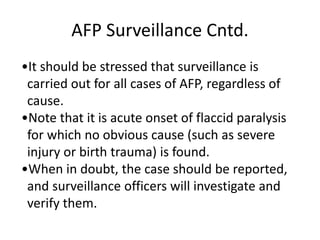
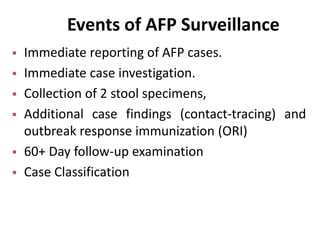
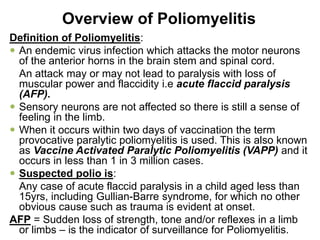
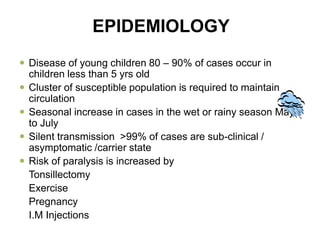
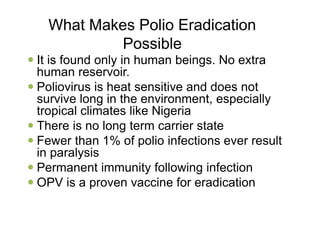
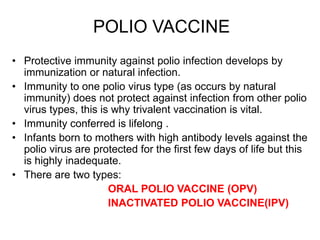
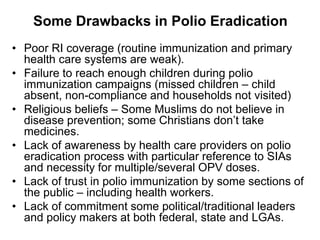
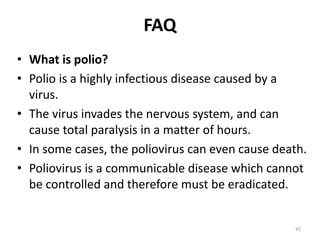
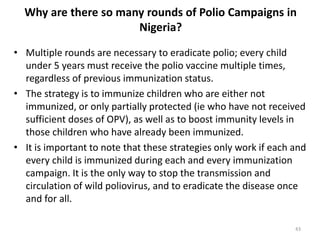
The document provides background information on Nigeria's polio eradication efforts. It discusses the establishment of the Global Polio Eradication Initiative in 1988 and Nigeria's declaration of polio as a national public health emergency. It outlines Nigeria's strategies for polio eradication including routine immunization, supplemental immunization campaigns, surveillance of acute flaccid paralysis cases, and inter-agency coordination mechanisms. It also summarizes Nigeria's progress in reducing polio cases from 2013-2015 and ongoing challenges to achieving eradication.