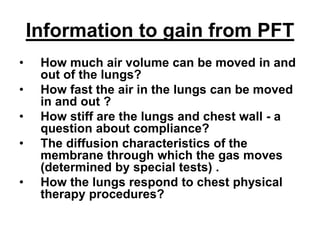
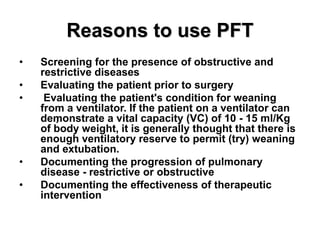
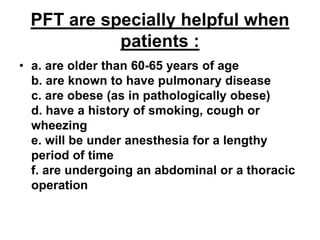
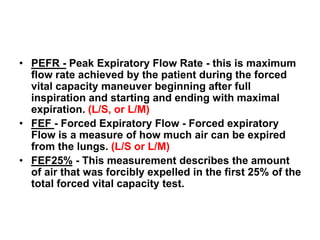
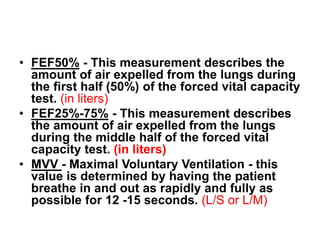
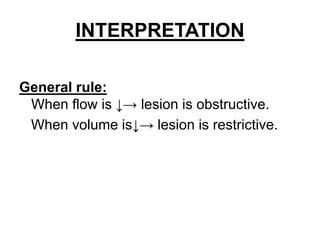
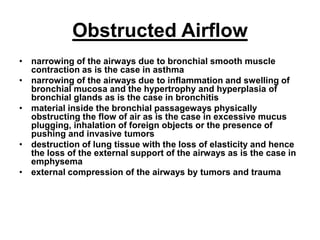
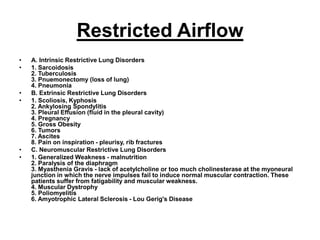
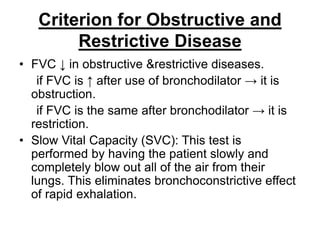
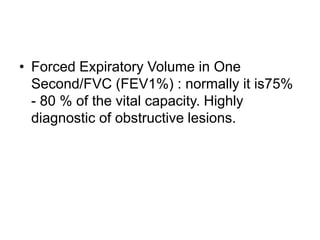
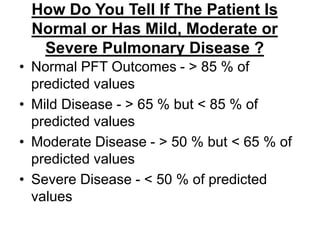
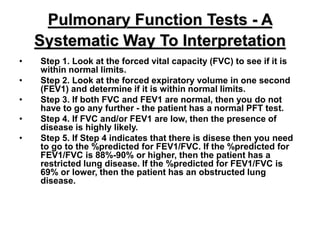
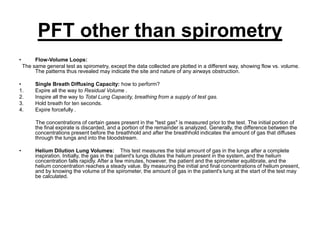
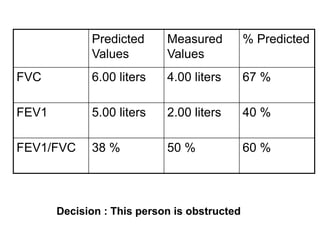
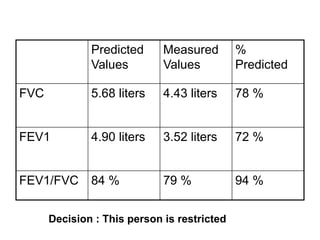
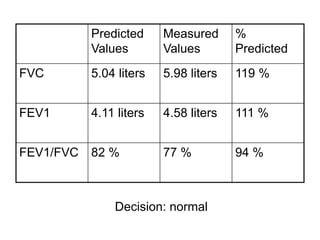
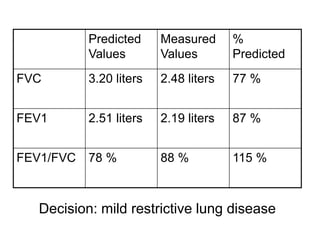
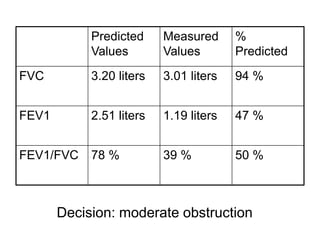
The document discusses the clinical applications of pulmonary function tests (PFTs), detailing important metrics such as lung volume, airflow, and lung compliance. It outlines the reasons for using PFTs, including disease screening, surgical evaluations, and the assessment of pulmonary disease progression. Additionally, it provides insights into the interpretation of test results, the equipment used, and the criteria for distinguishing between obstructive and restrictive lung diseases.