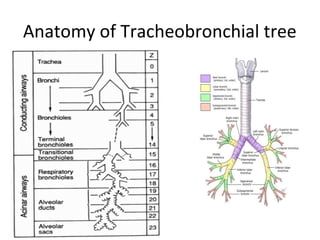
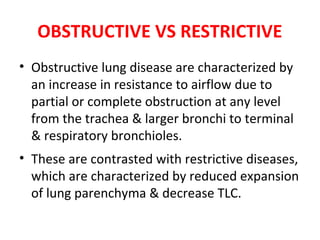
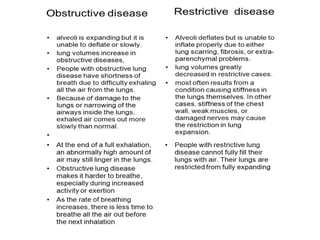
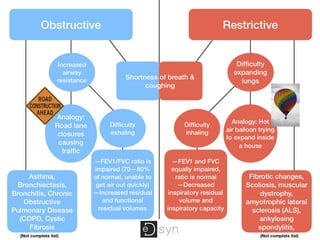
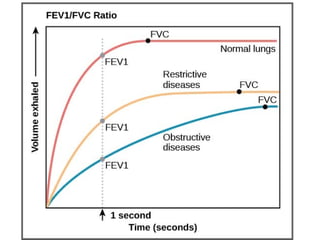
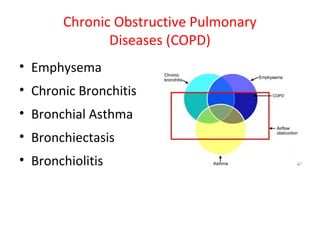
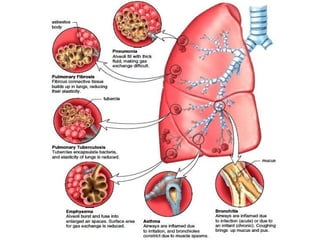
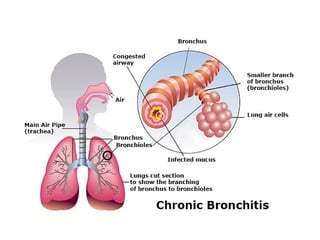
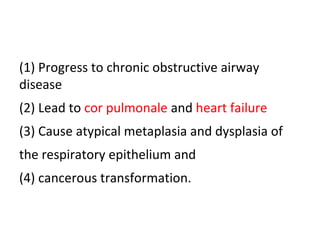
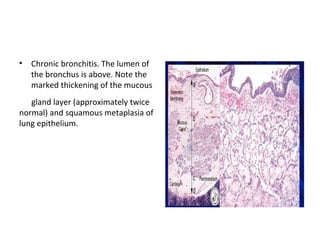
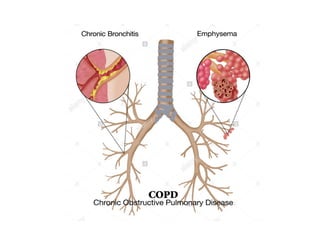
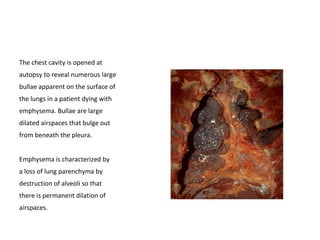
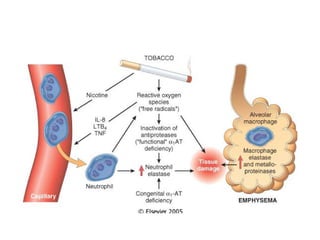
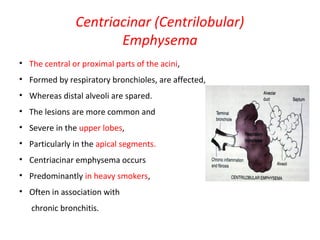
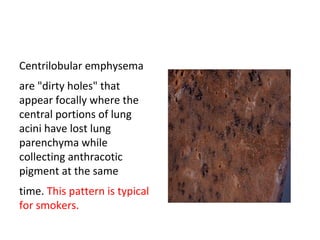
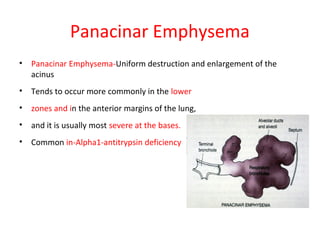
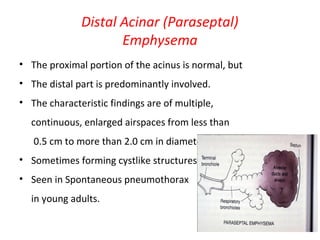
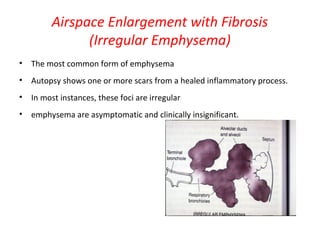
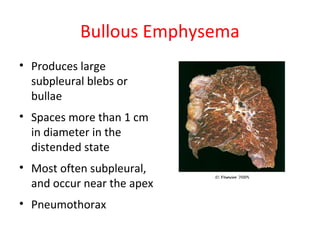
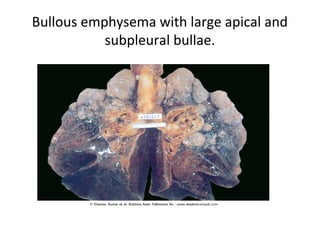
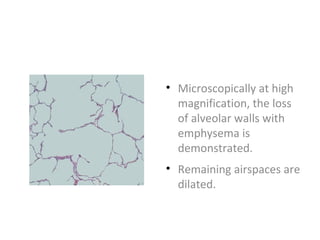
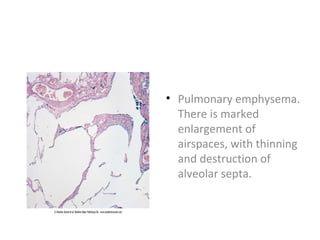
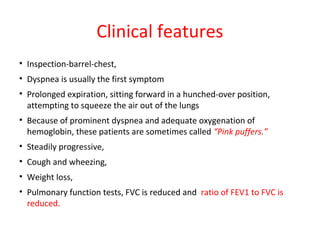
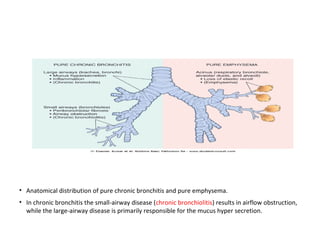
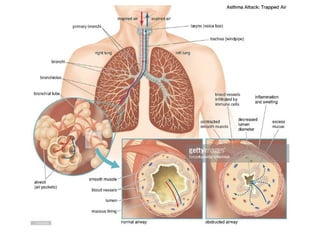
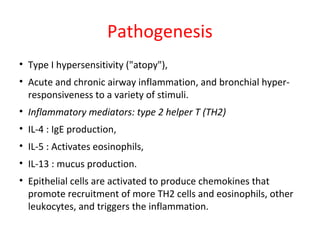
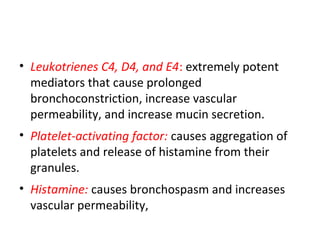
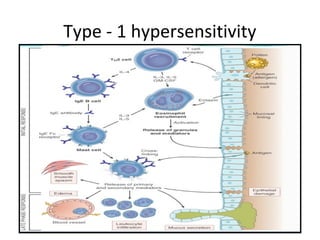
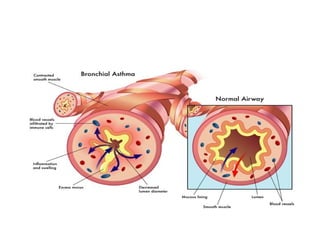
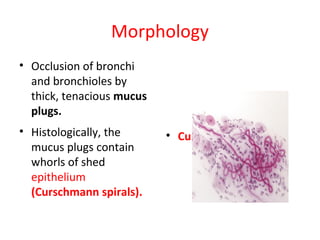
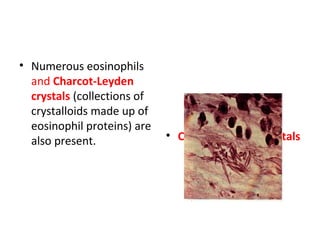
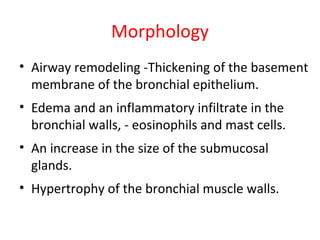
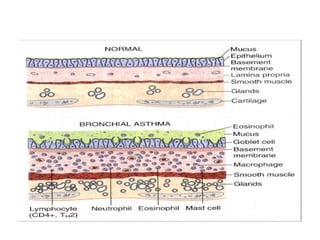
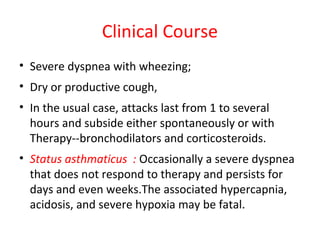
The document outlines chronic obstructive pulmonary diseases (COPD), focusing on chronic bronchitis, emphysema, and bronchiectasis, highlighting the pathogenesis, clinical features, and complications associated with each. It details the mechanisms of airflow obstruction, inflammation, and the impact of factors like smoking and genetic conditions such as alpha-1 antitrypsin deficiency. Additionally, it discusses the morphological and histological characteristics of these diseases as well as their clinical manifestations and treatment considerations.