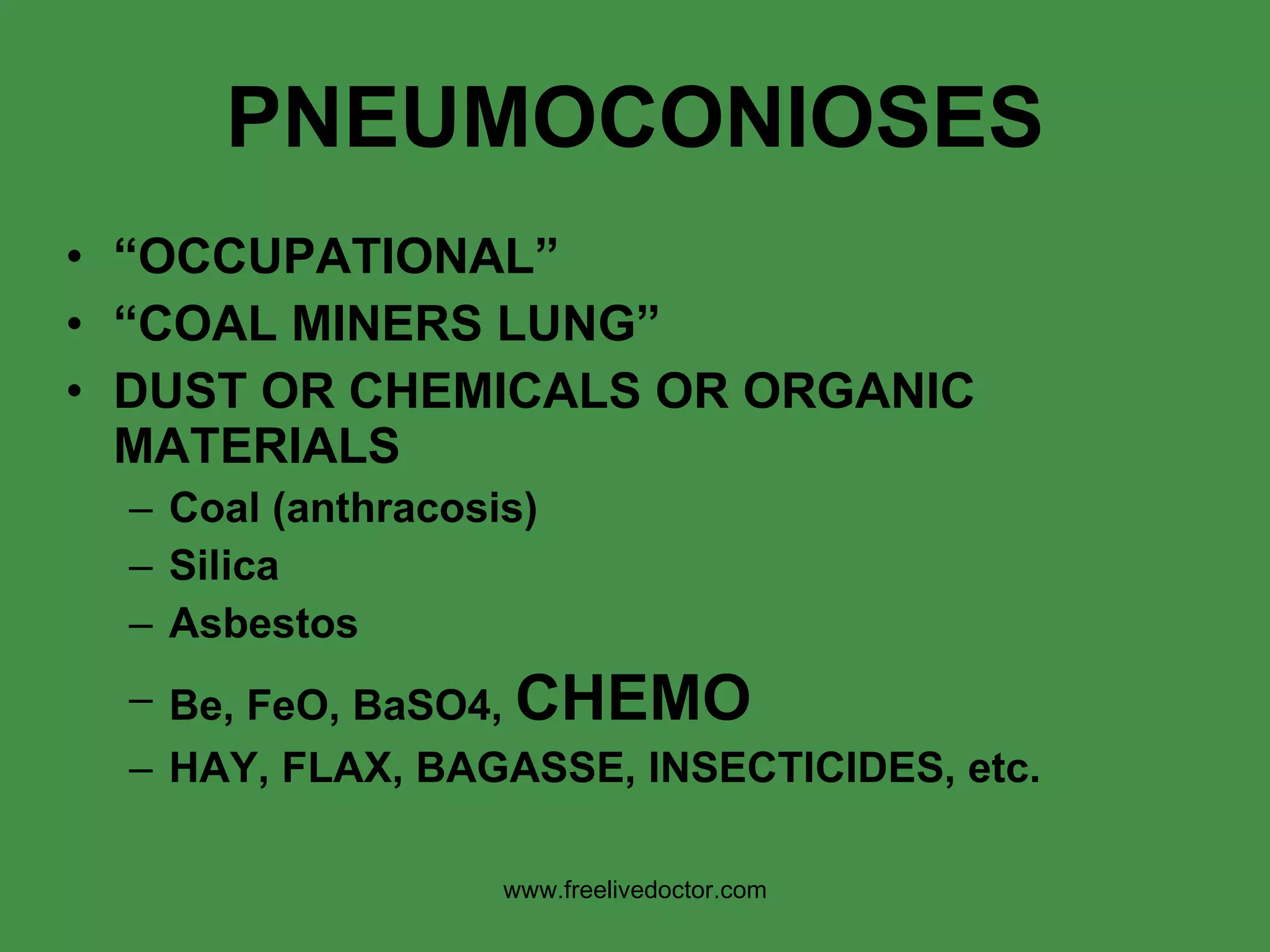
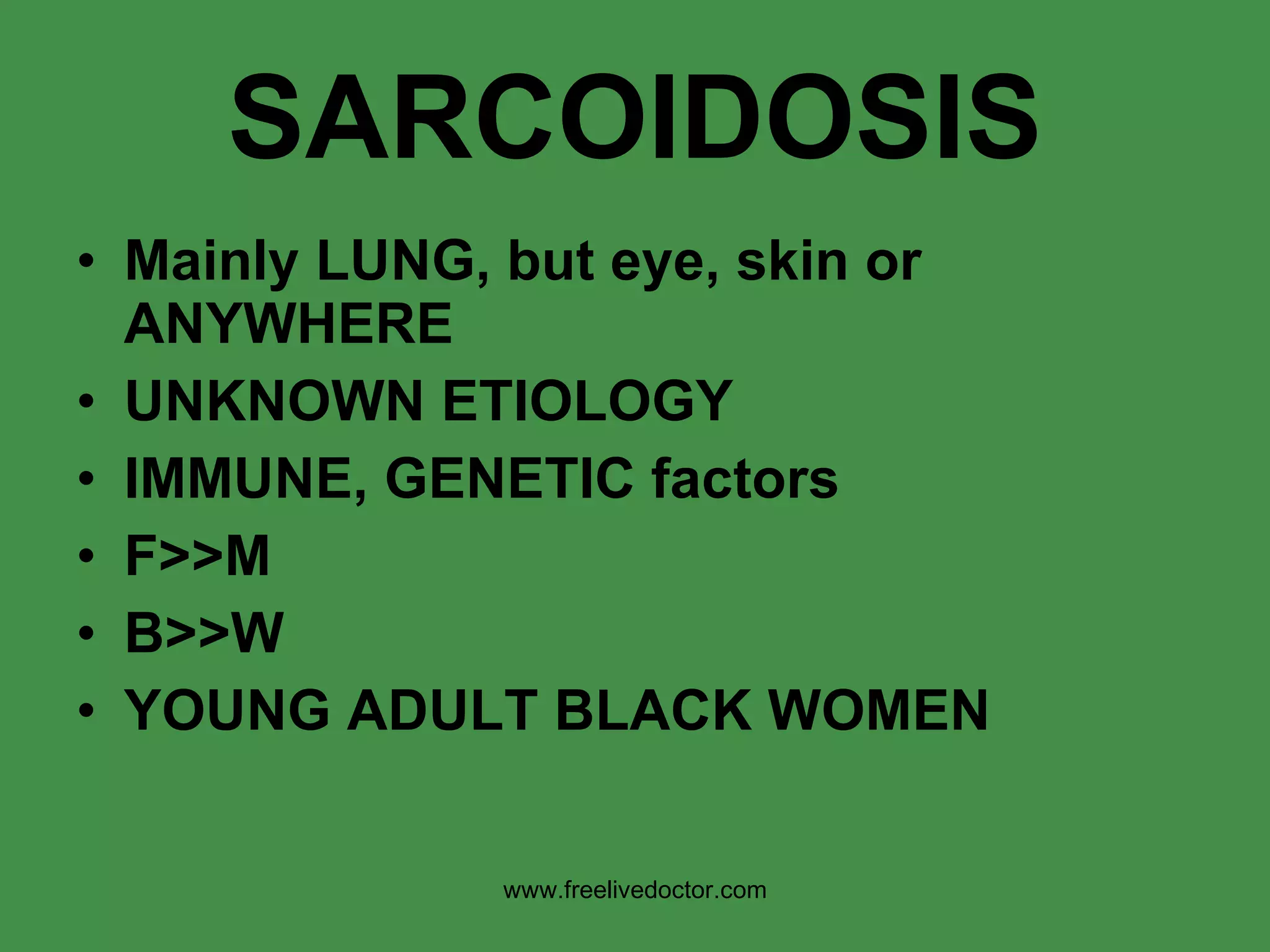
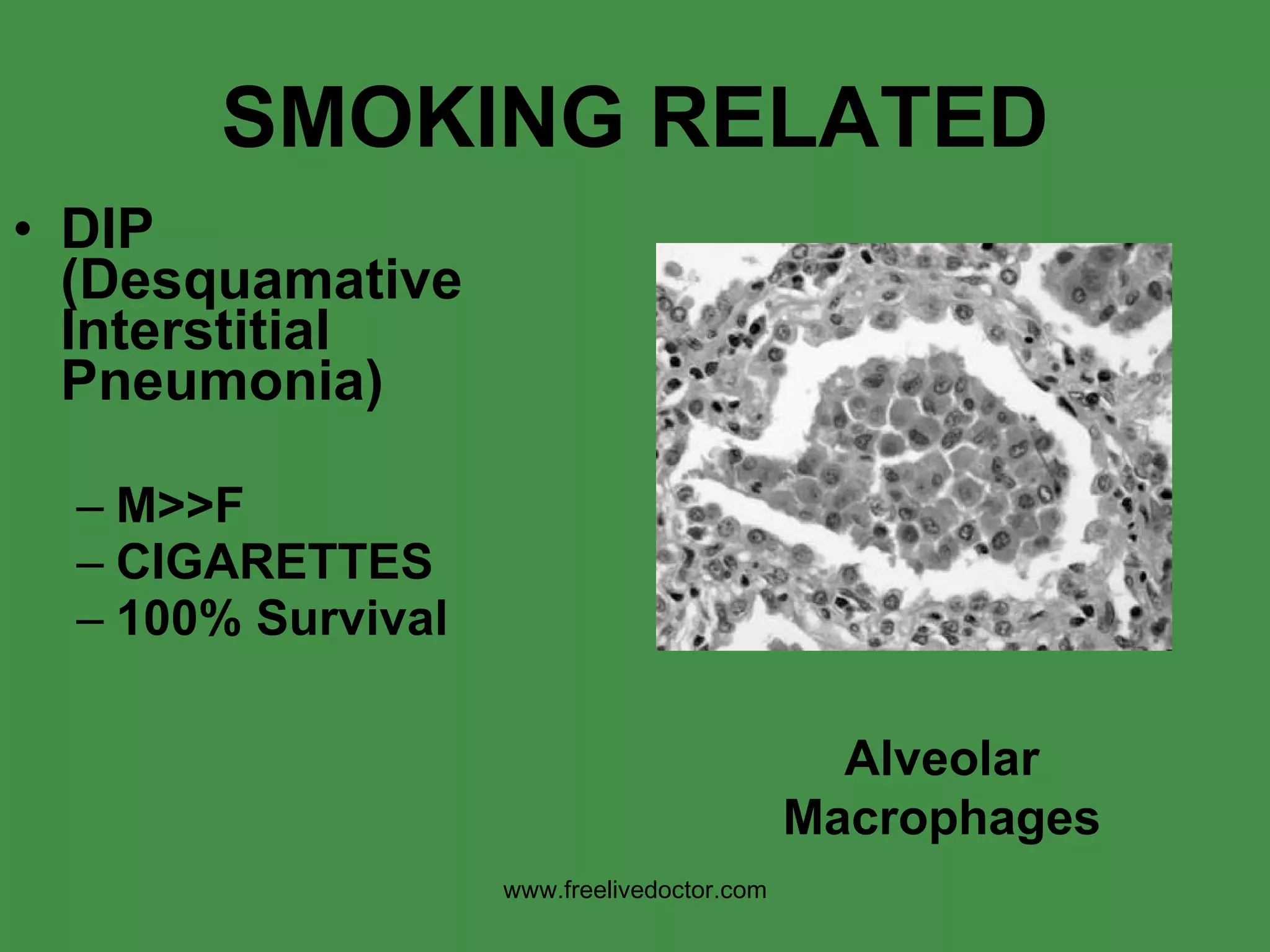
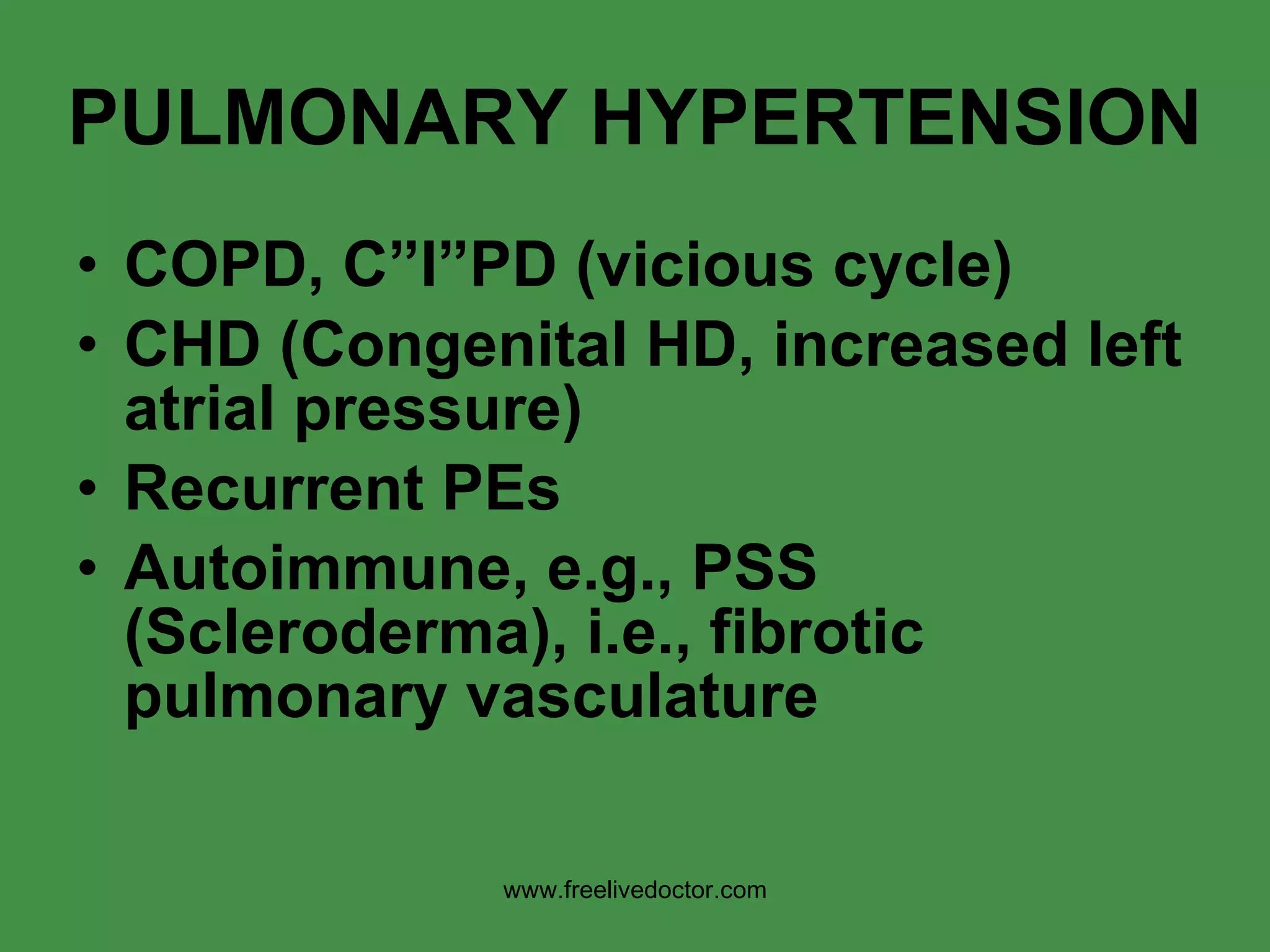
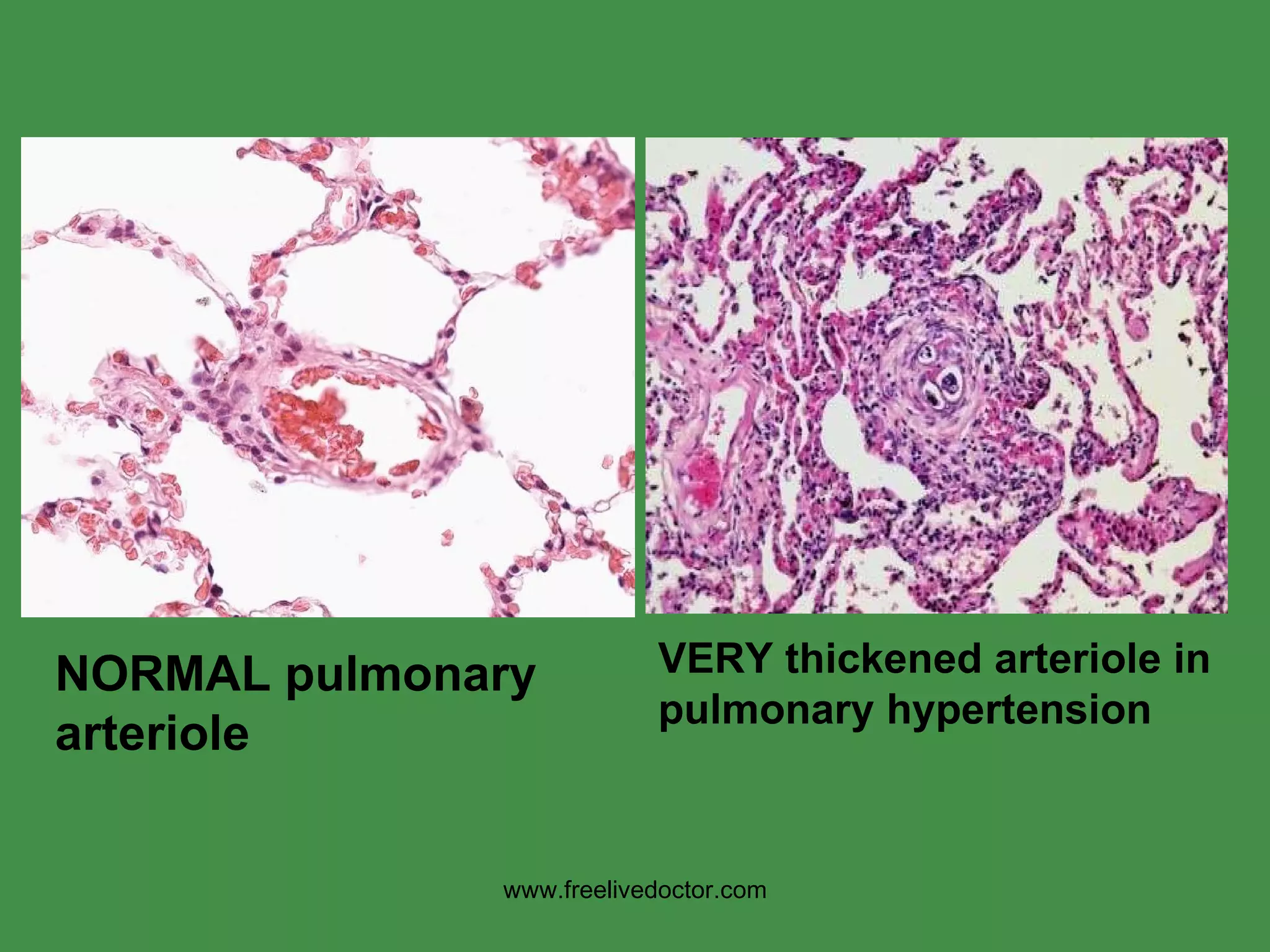
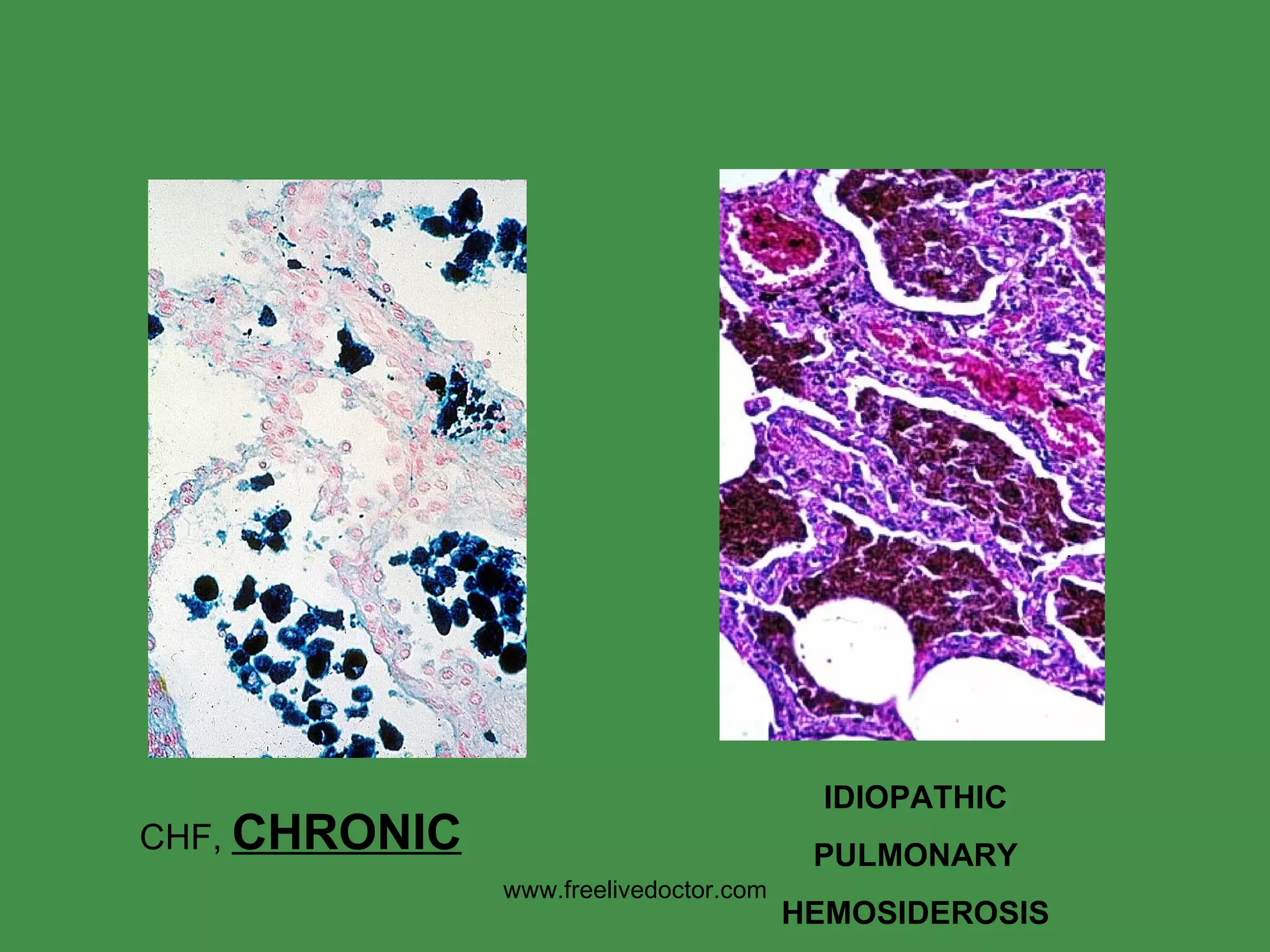
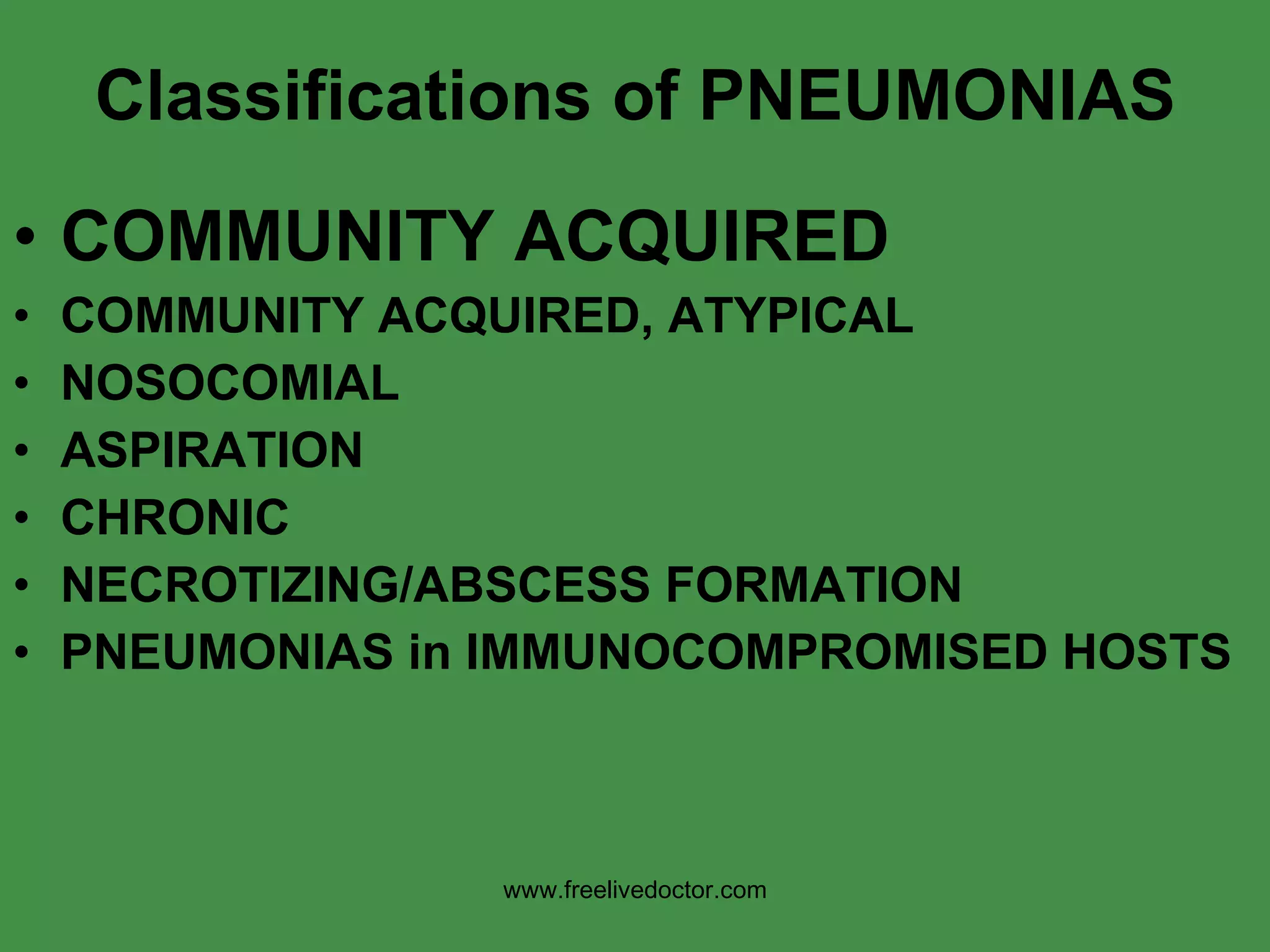
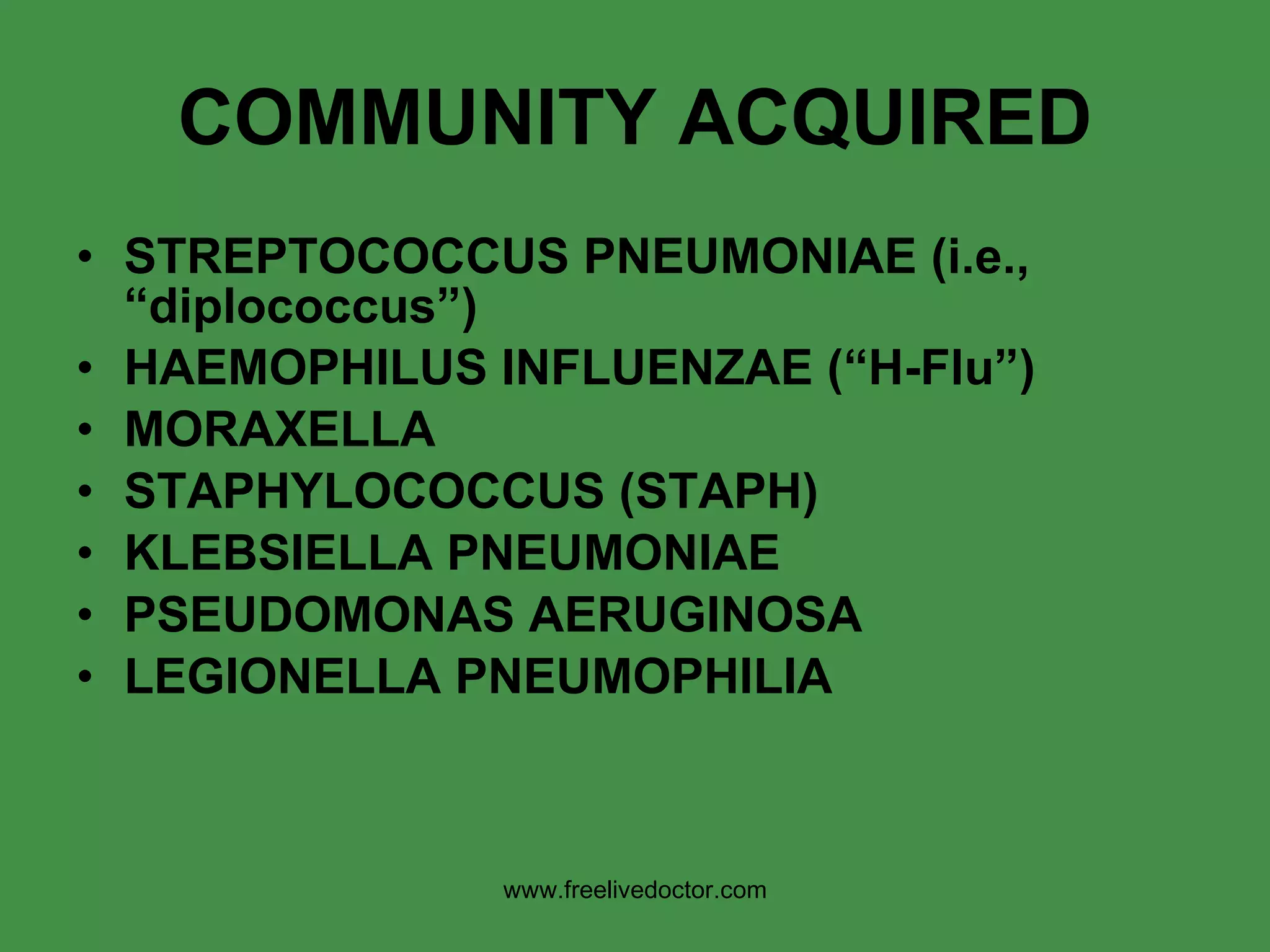
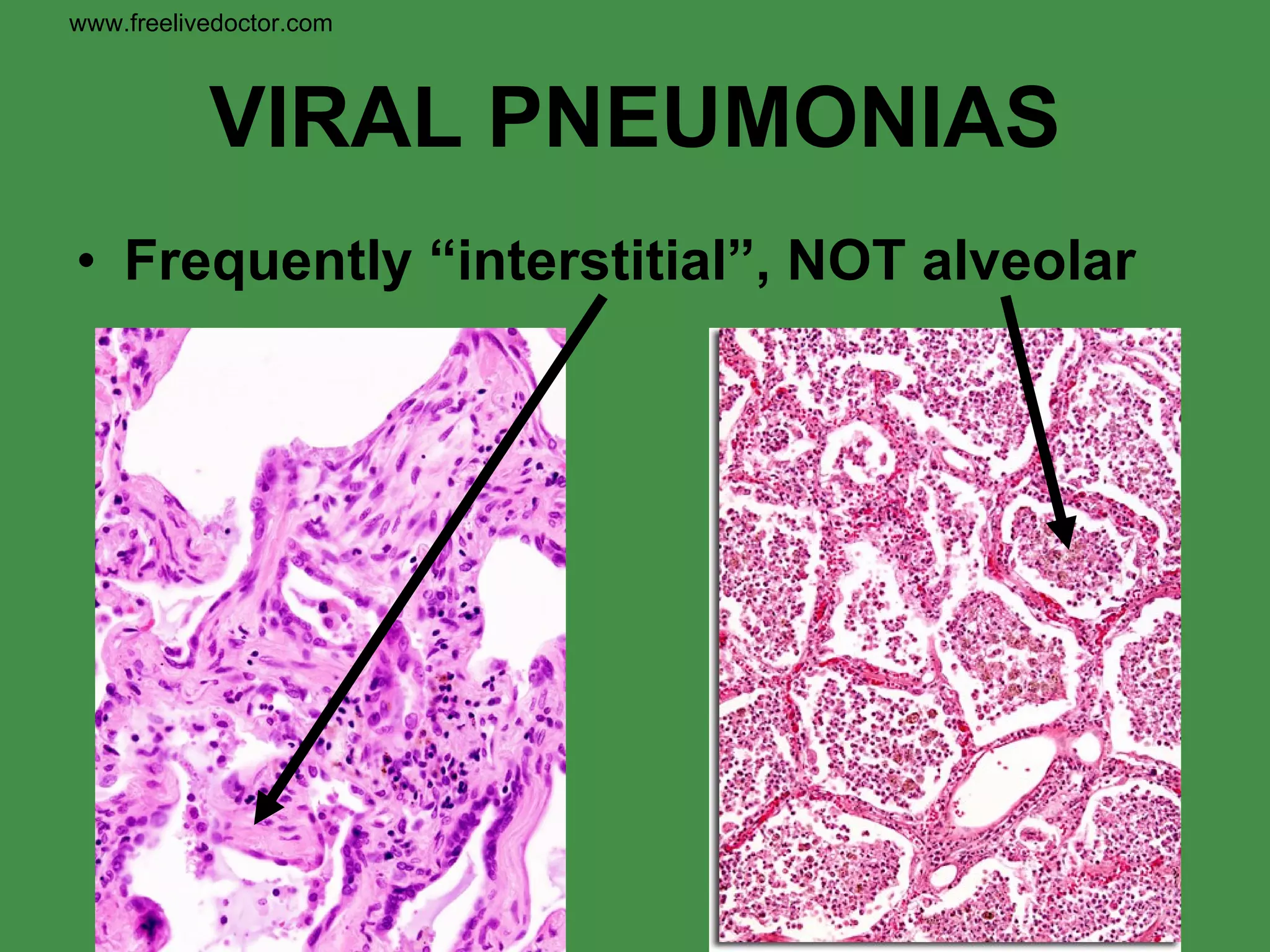
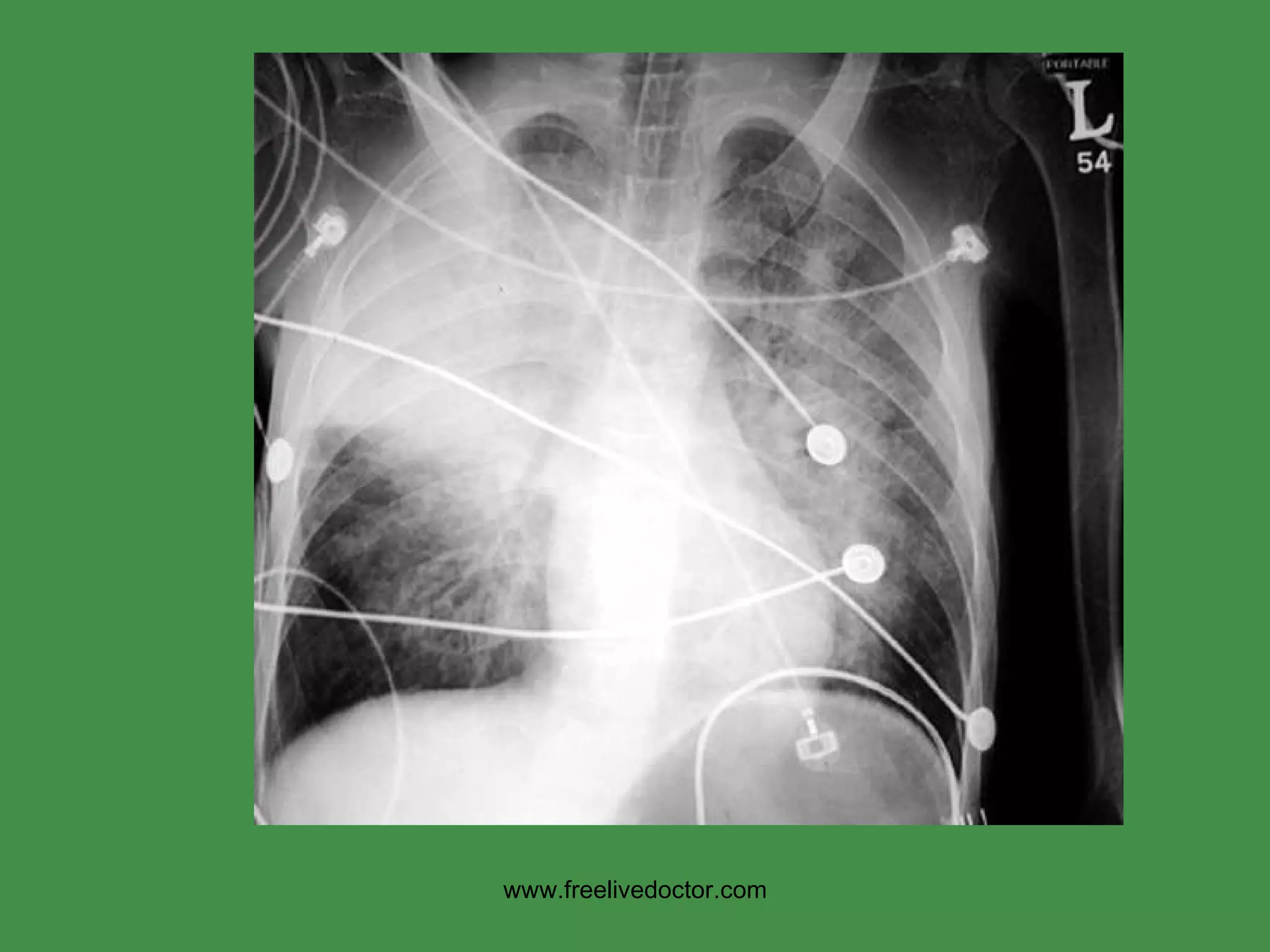
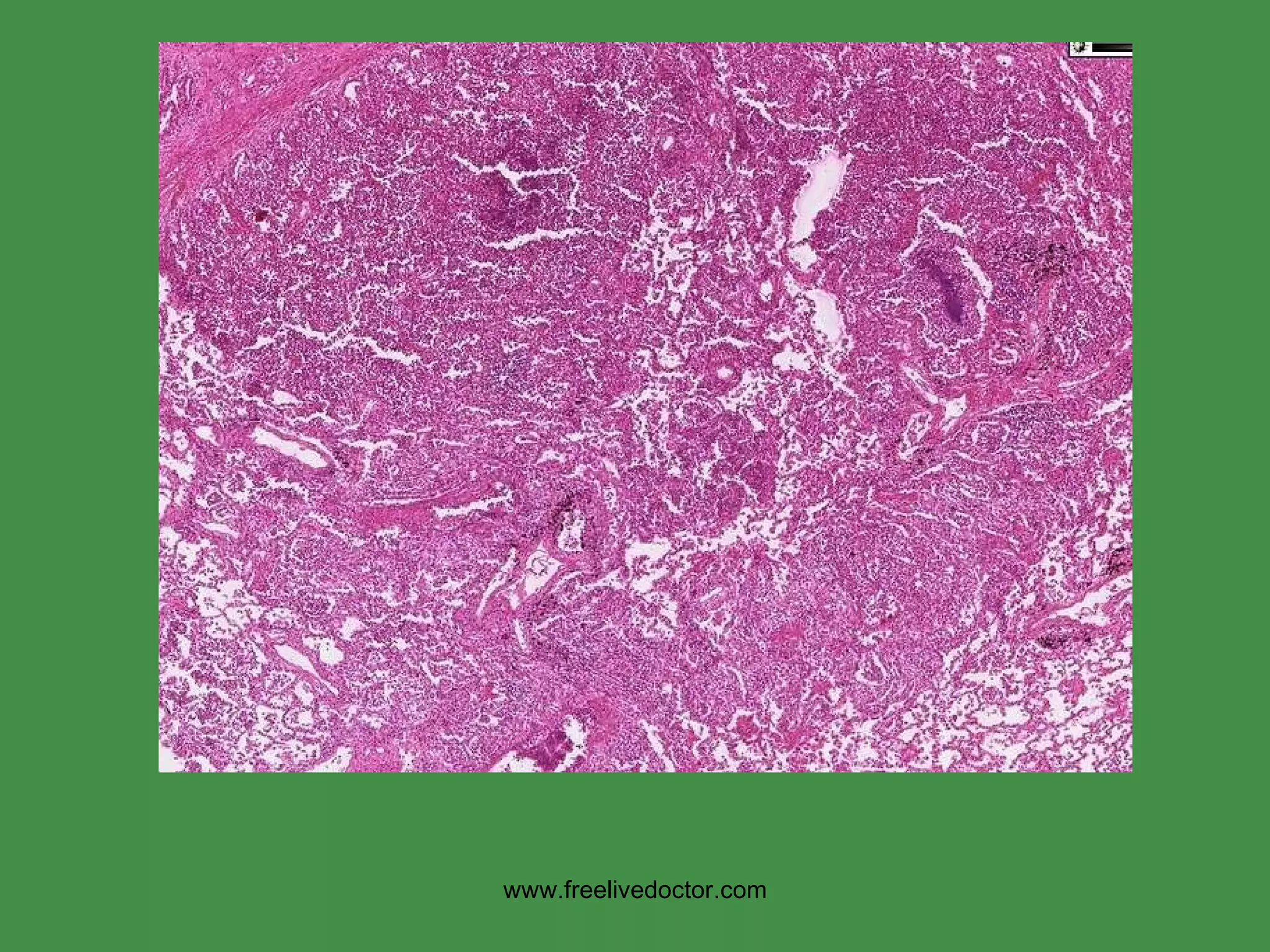
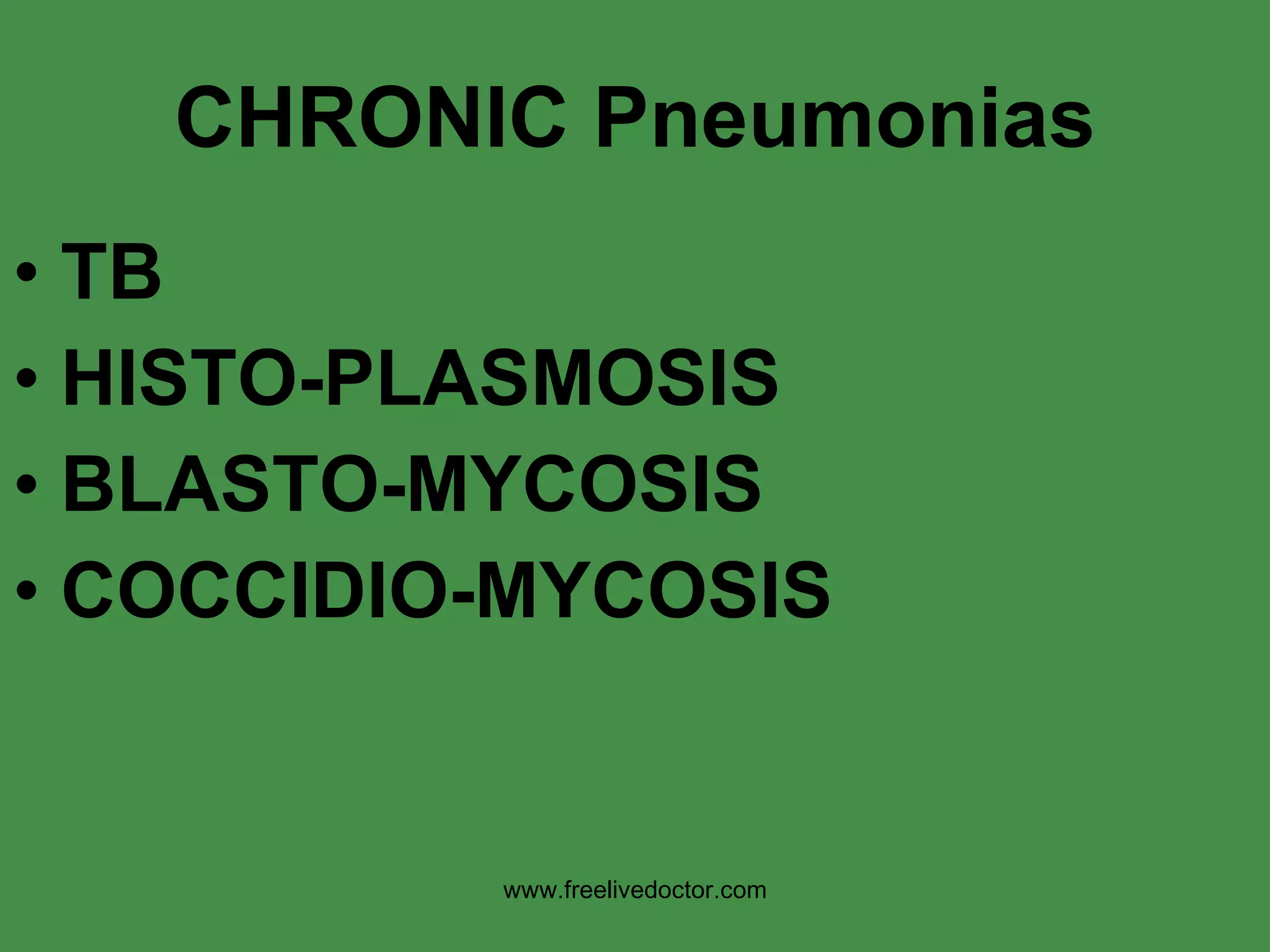
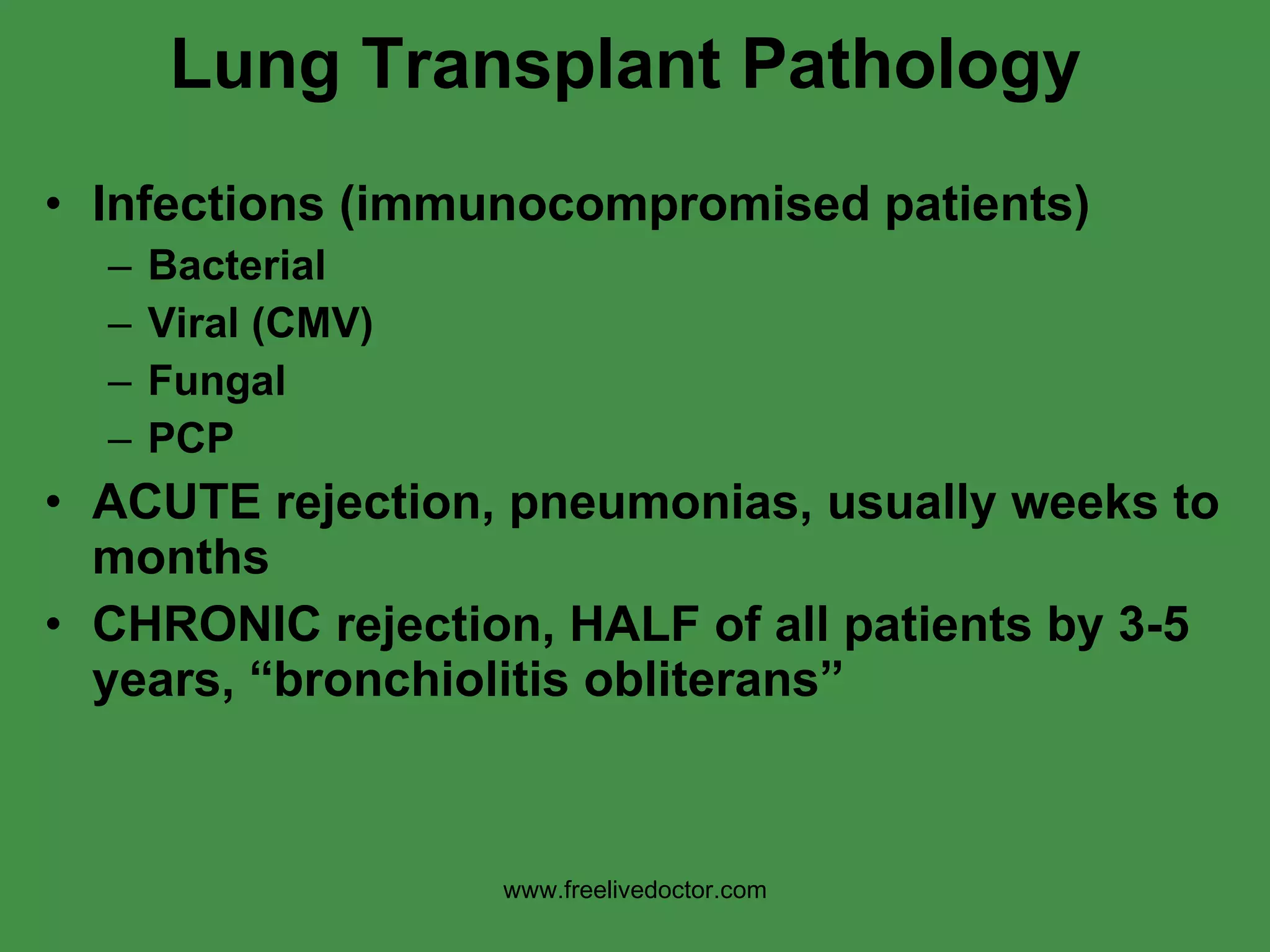
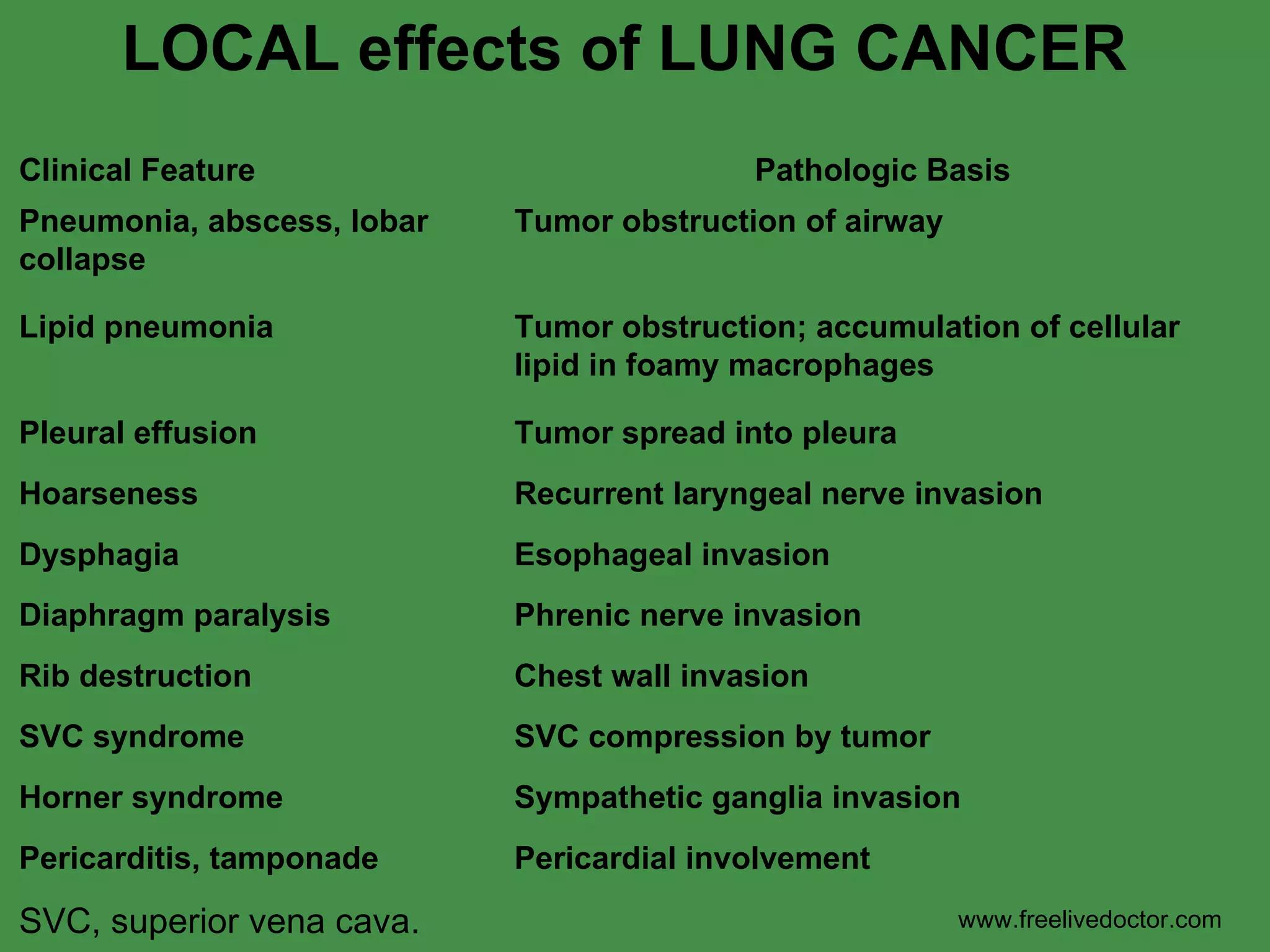
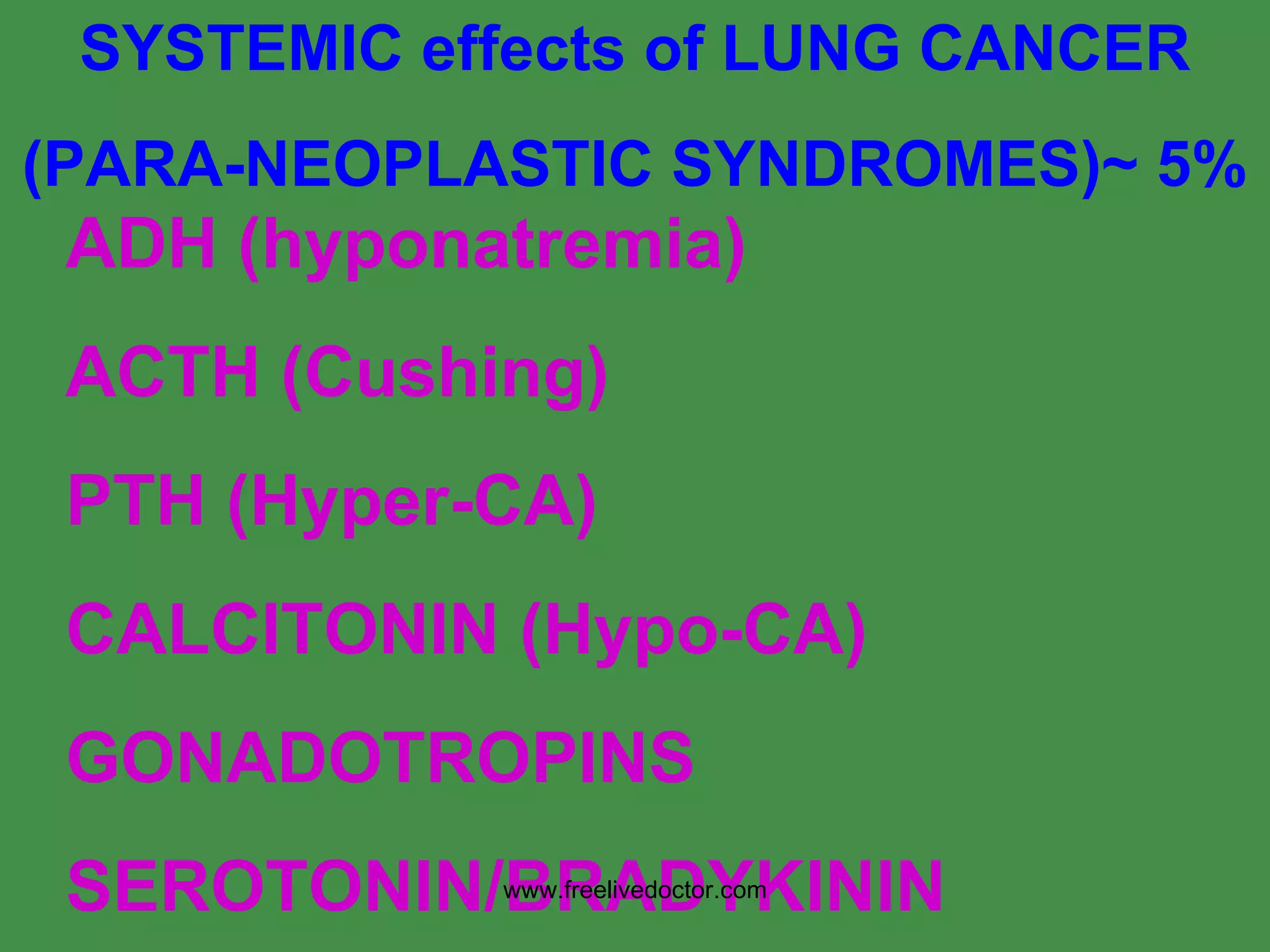
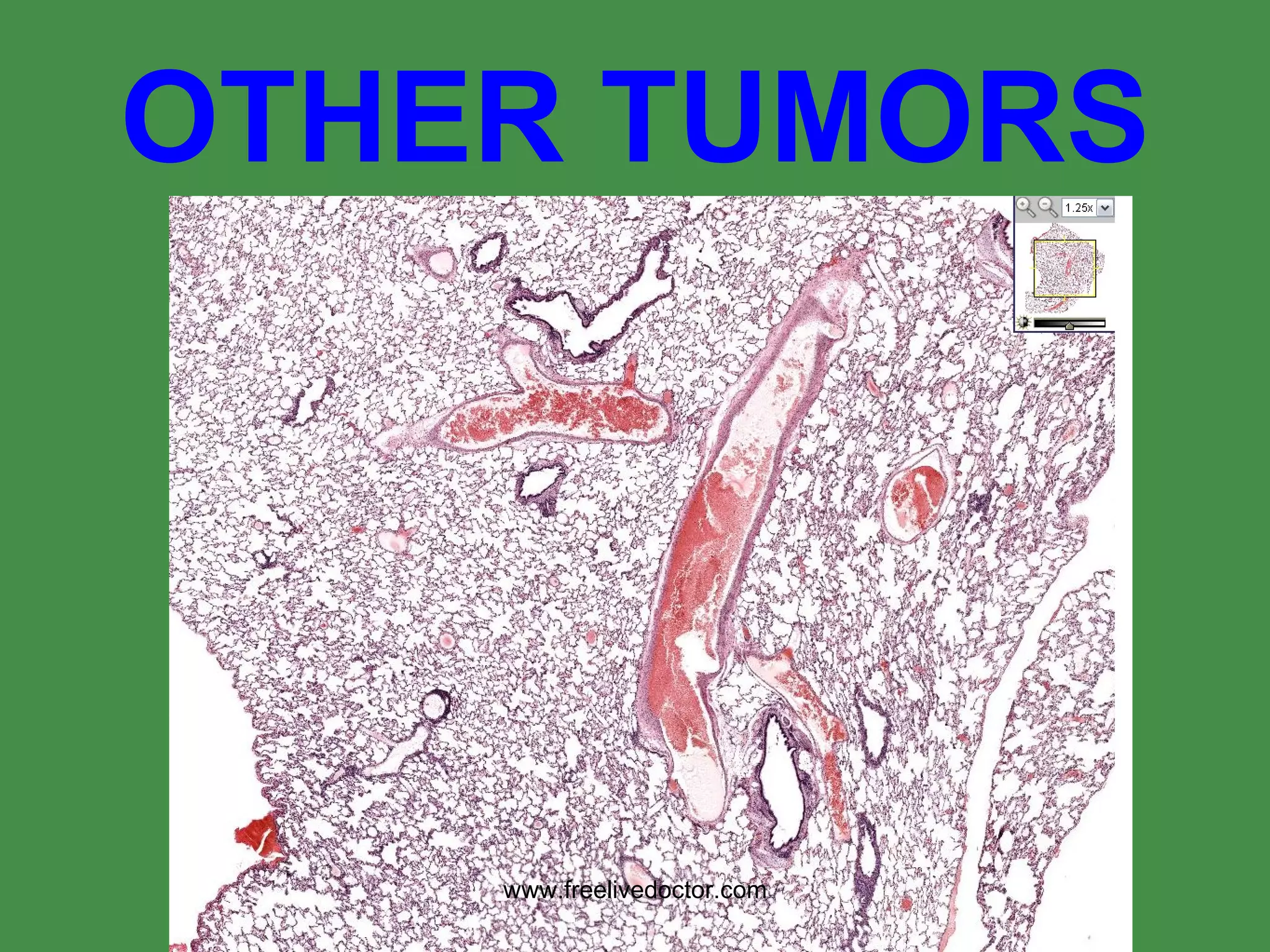
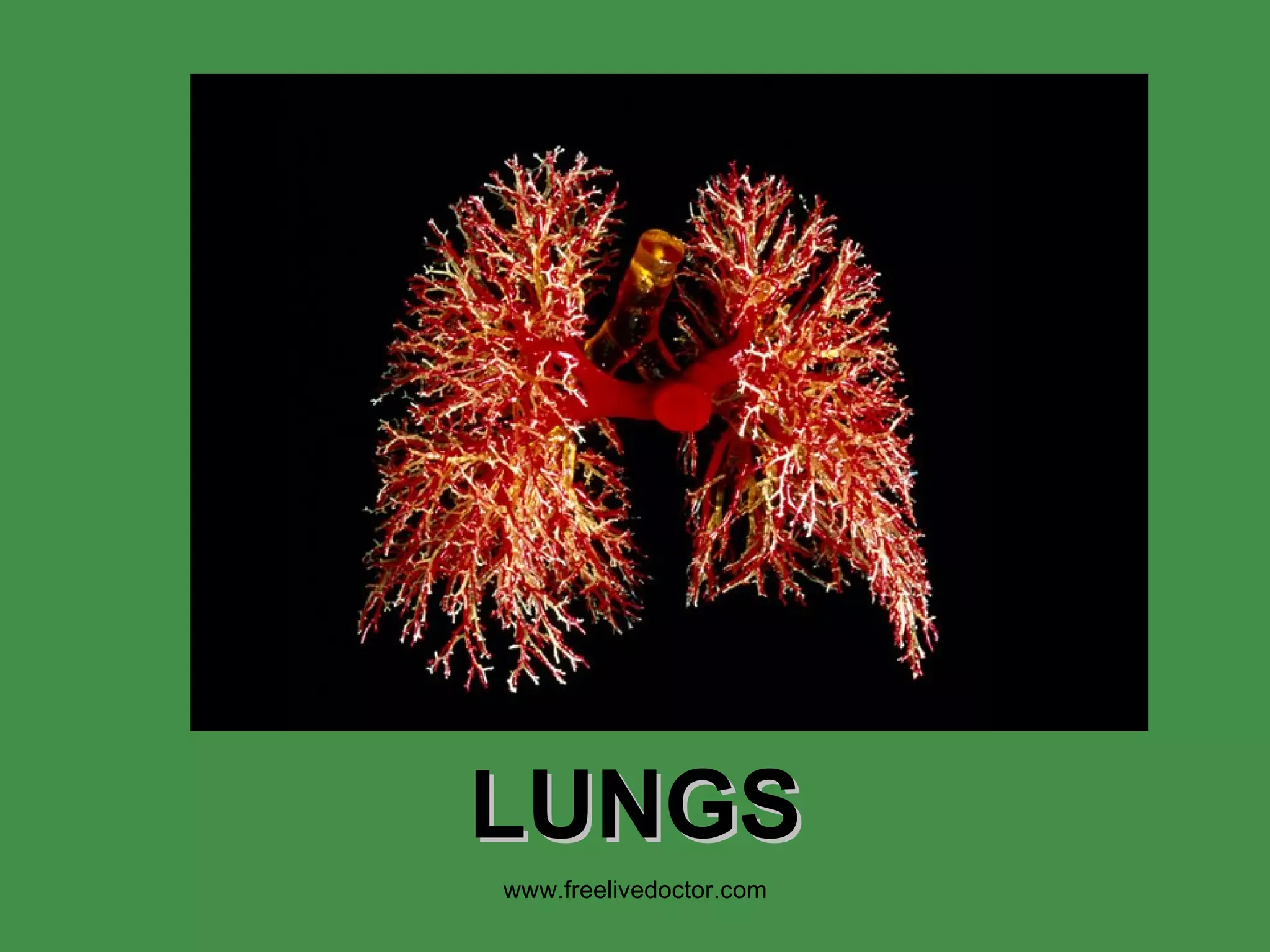
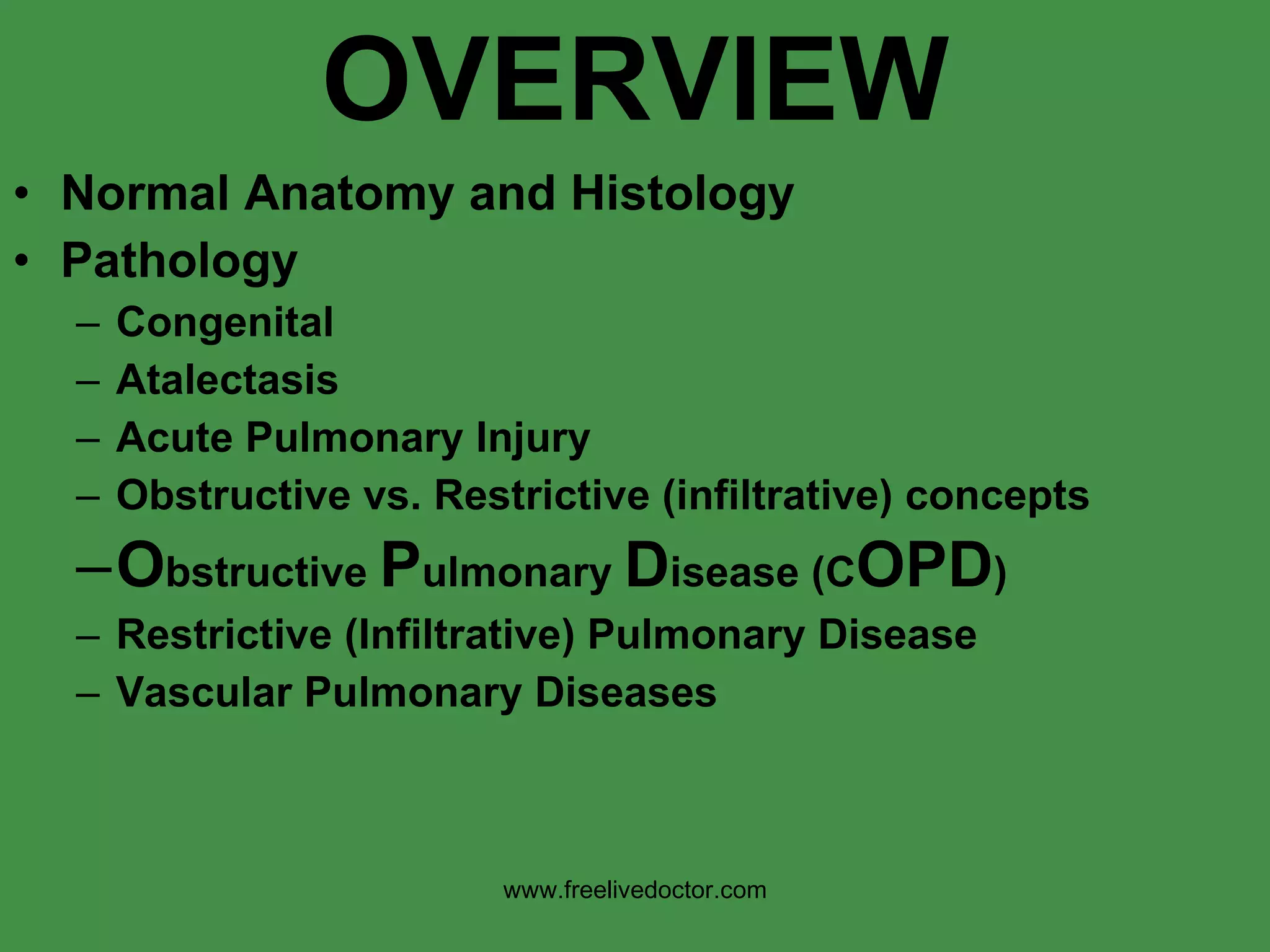
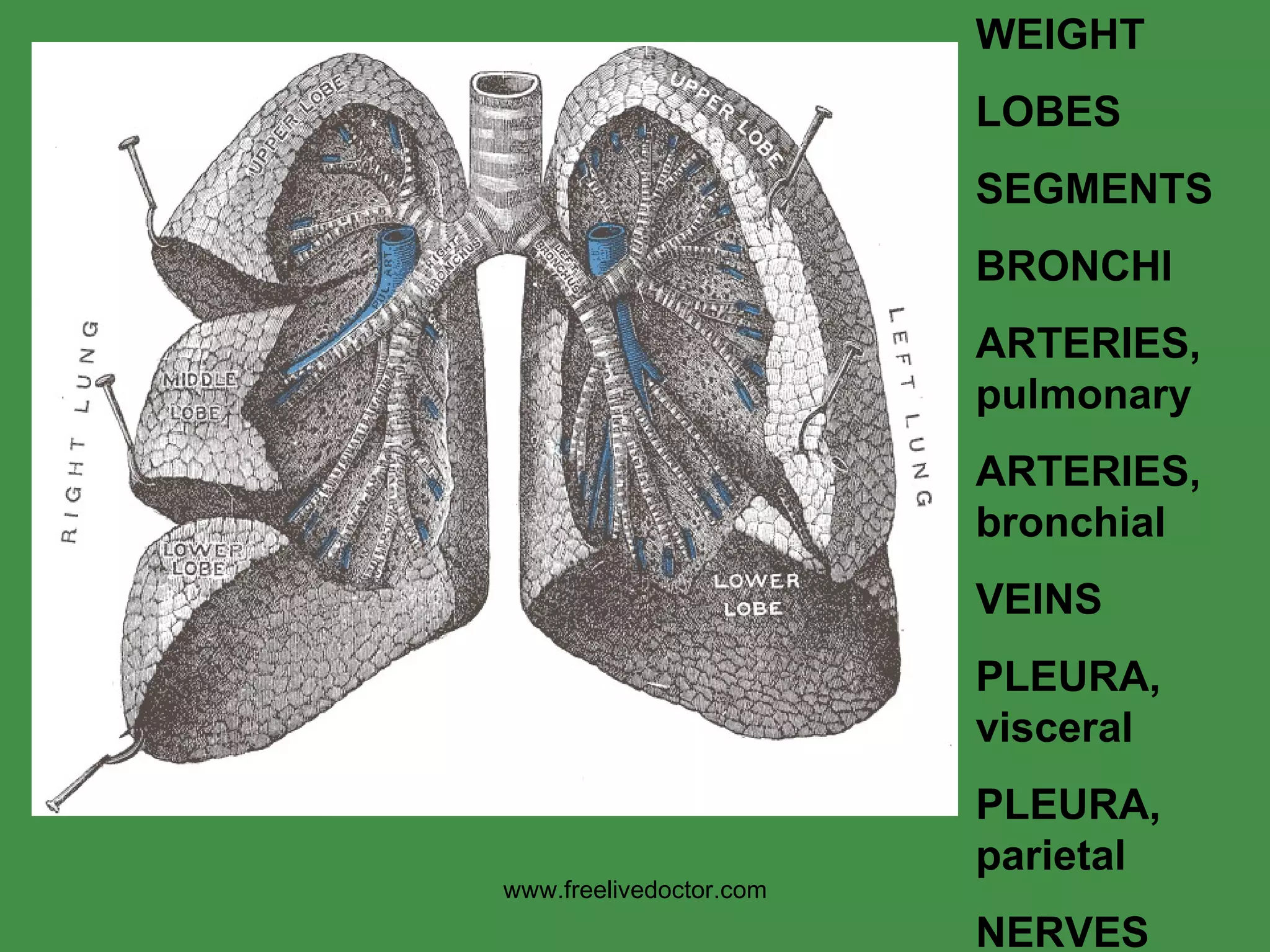
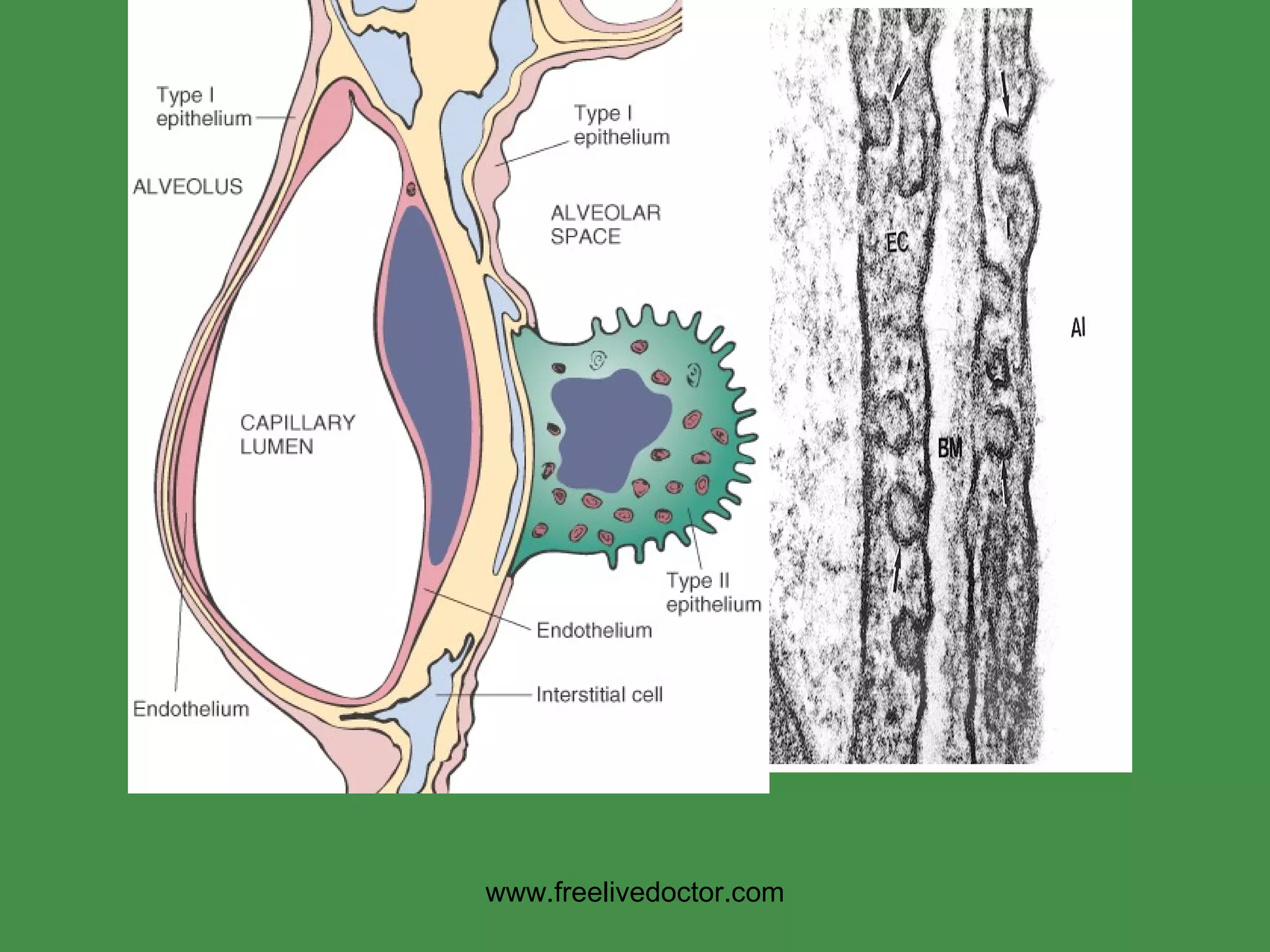
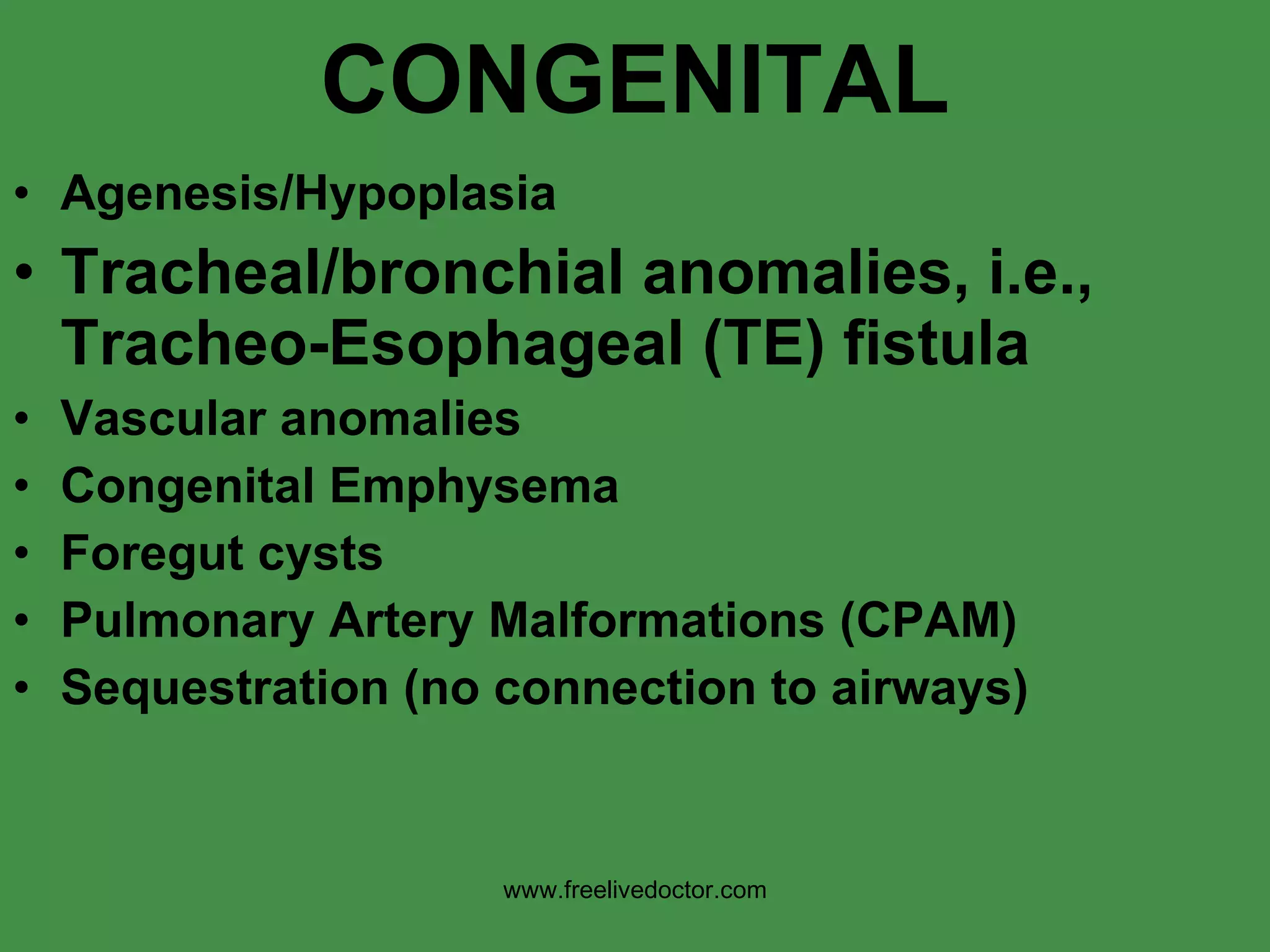
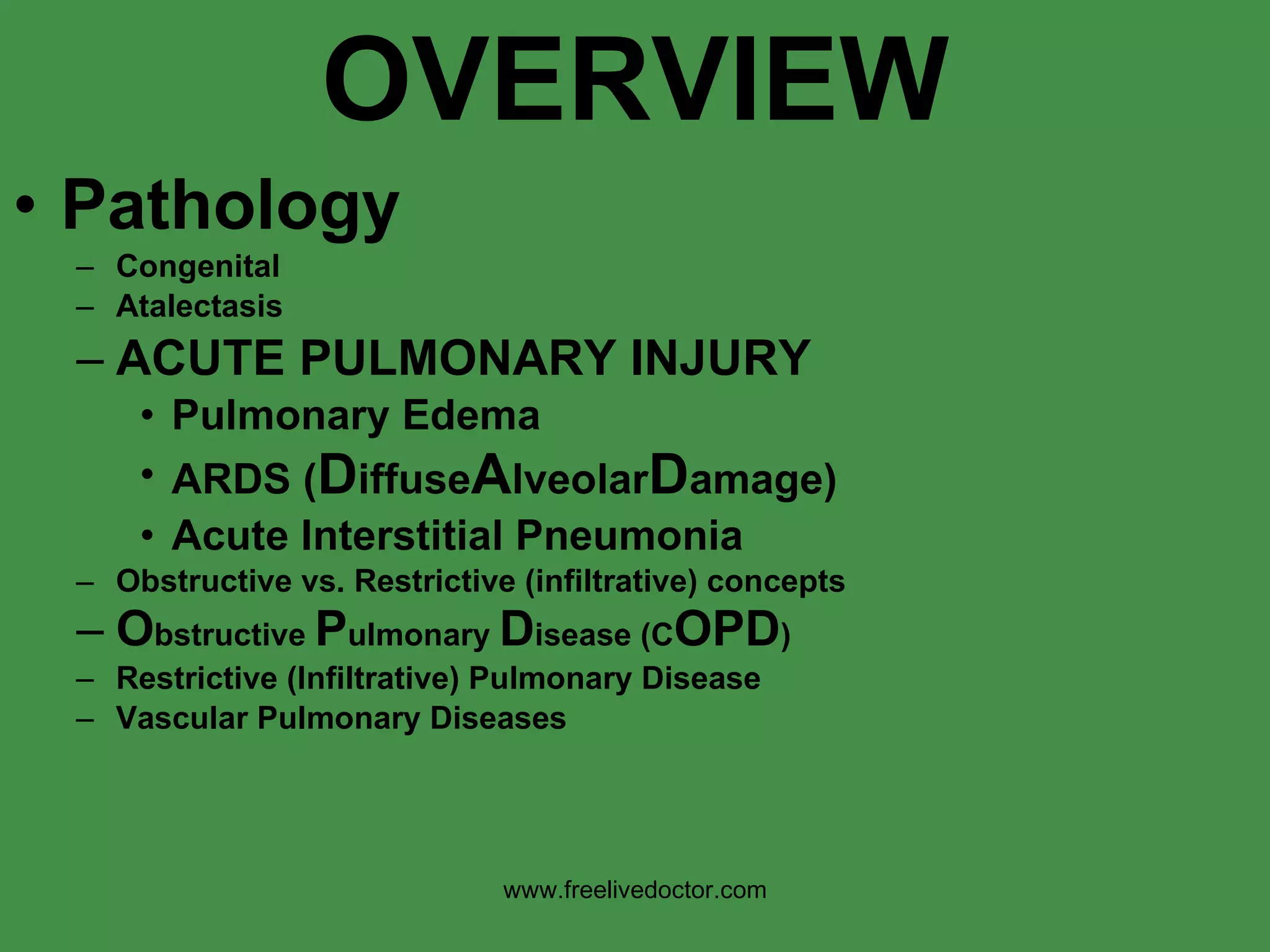
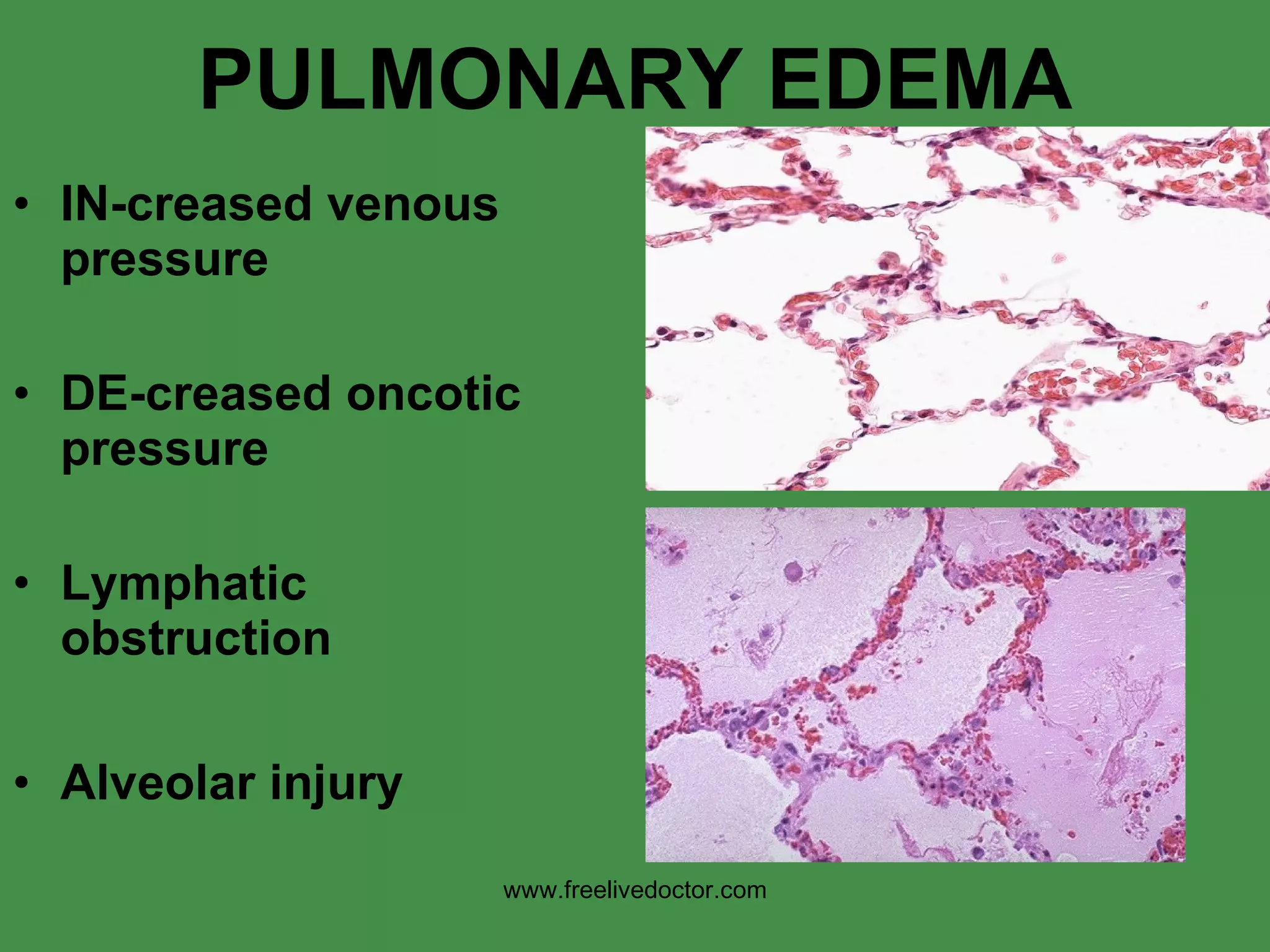
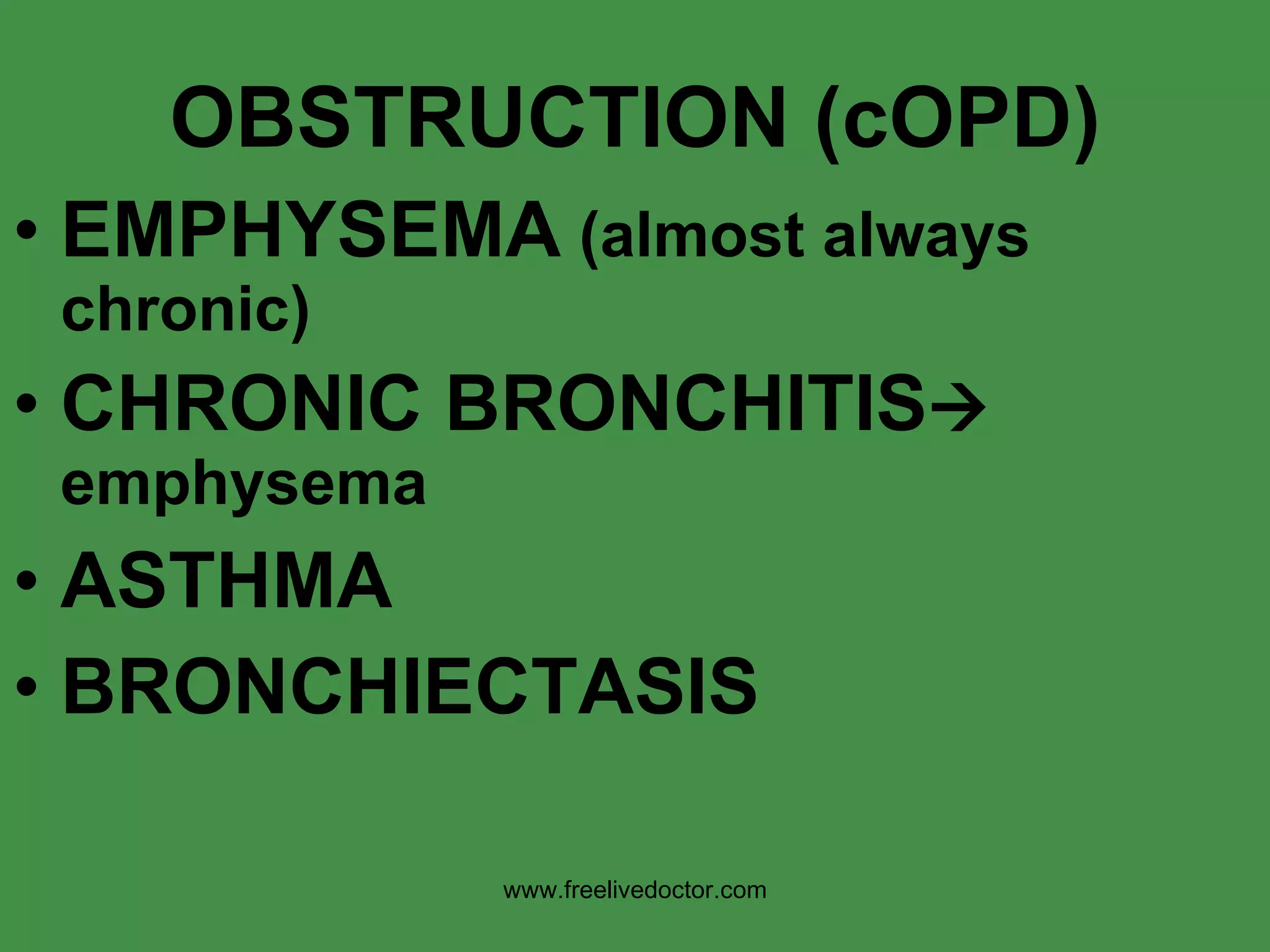
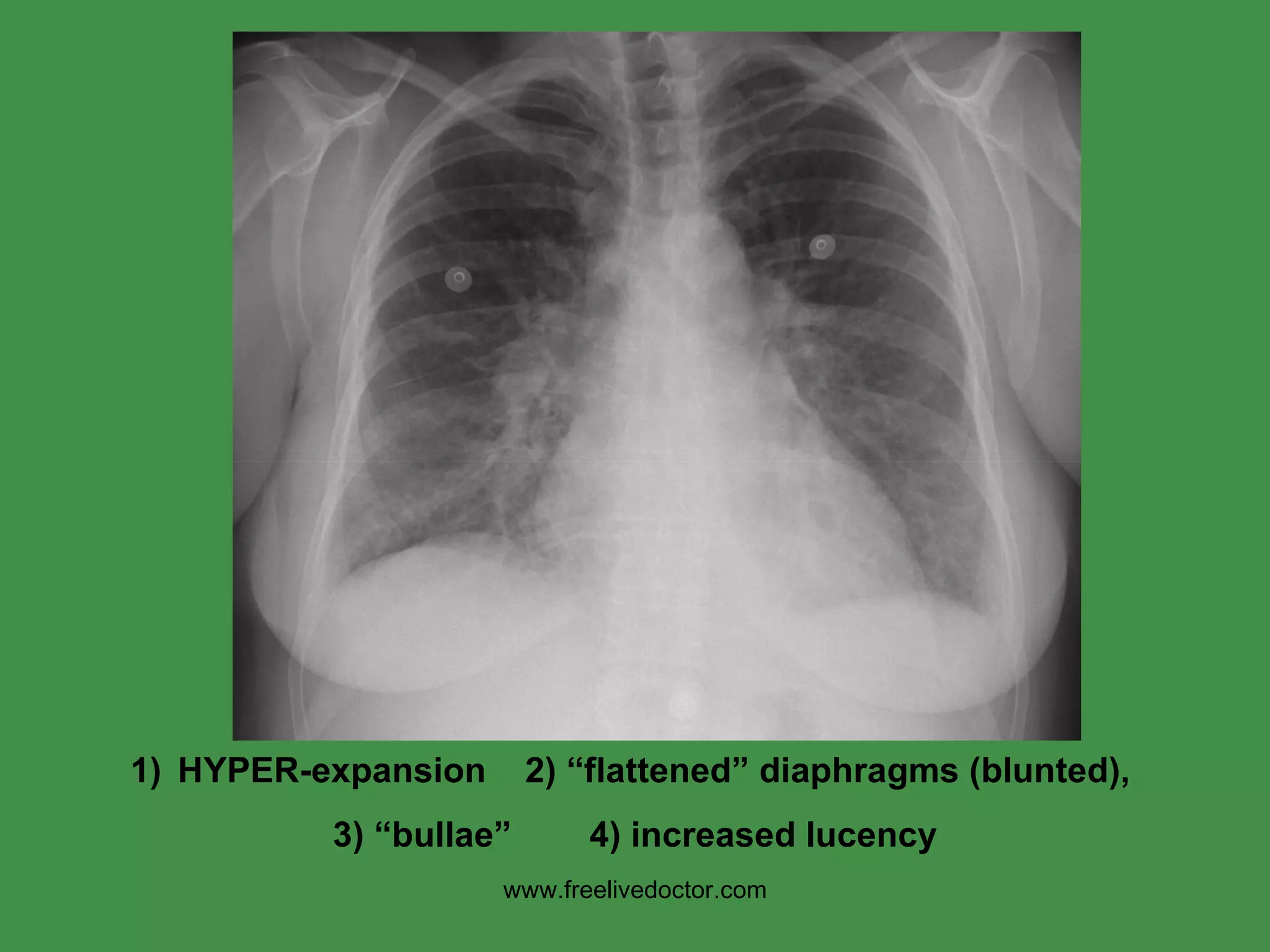
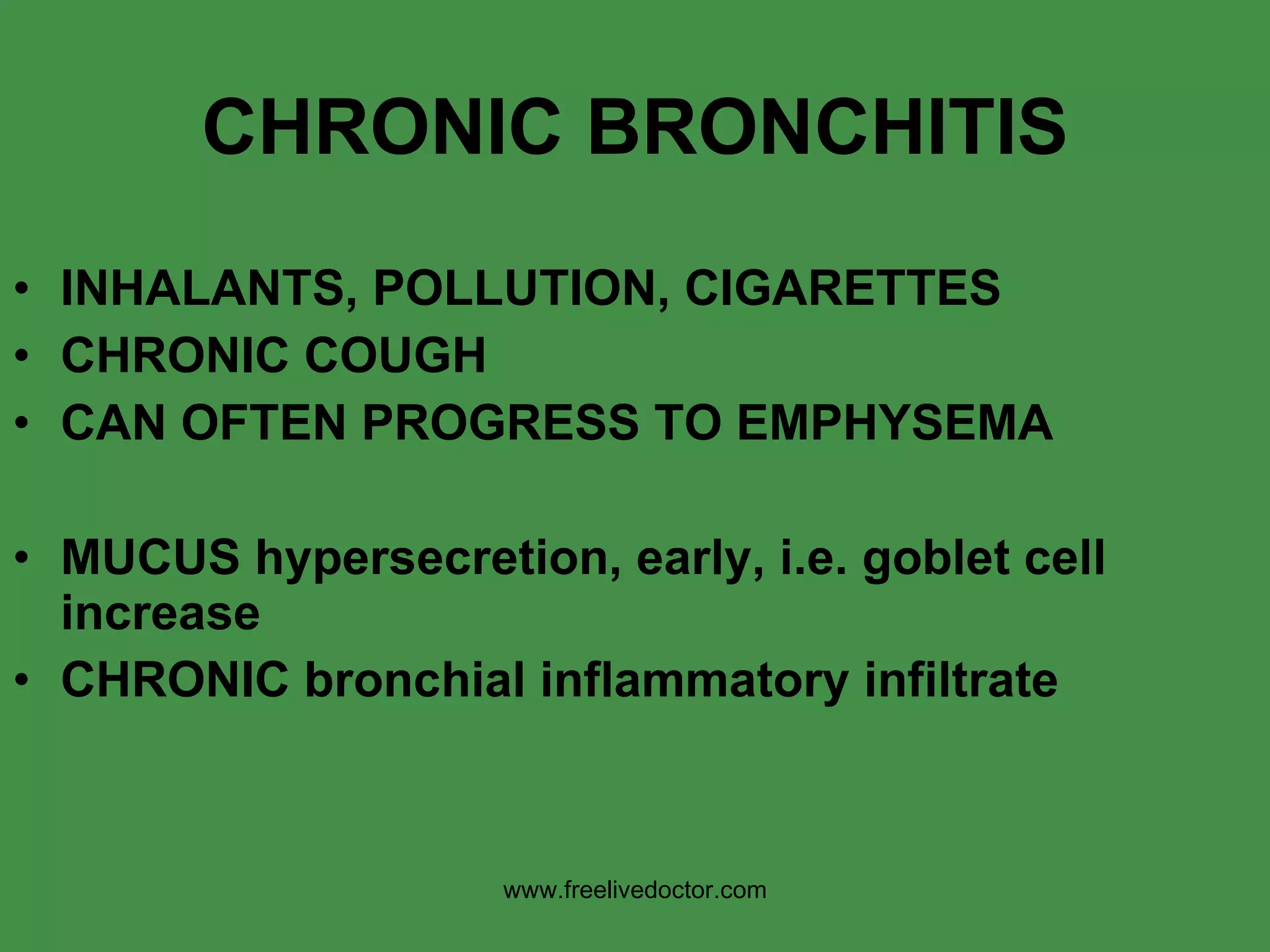
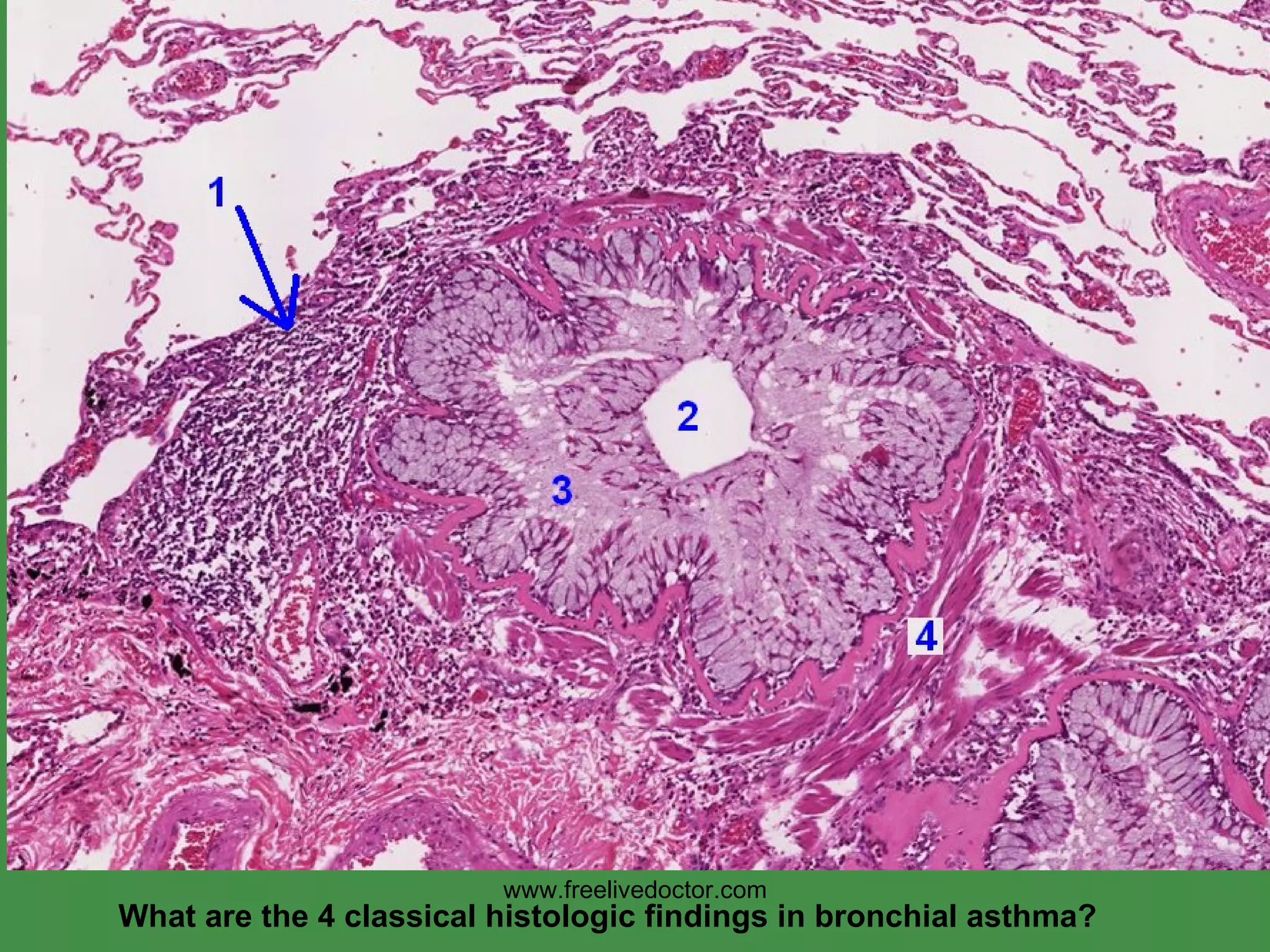
The document discusses the anatomy and pathology of the lungs. It covers normal lung anatomy and histology. Key topics include congenital lung abnormalities, acute and chronic lung injuries, obstructive and restrictive lung diseases such as COPD, pulmonary infections, neoplasms, and vascular diseases of the lungs. Specific lung pathologies like pneumonia, tuberculosis, and lung cancers are examined in detail.




![www.freelivedoctor.com NORMAL” chest X-Ray [CXR]](https://image.slidesharecdn.com/pulmonarypathology-100417025745-phpapp01/75/Pulmonary-pathology-9-2048.jpg)

















![RESTRICTIVE (INFILTRATIVE) REDUCED COMPLIANCE, reduced gas exchange) Are also DIFFUSE HETEROGENEOUS FIBROSING GRANULOMATOUS EOSINOPHILIC SMOKING RELATED PAP [Pulmonary Alveolar Proteinosis] www.freelivedoctor.com](https://image.slidesharecdn.com/pulmonarypathology-100417025745-phpapp01/75/Pulmonary-pathology-35-2048.jpg)