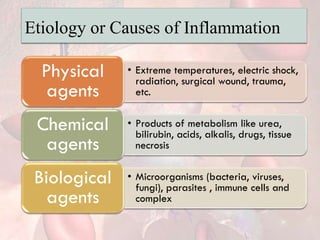
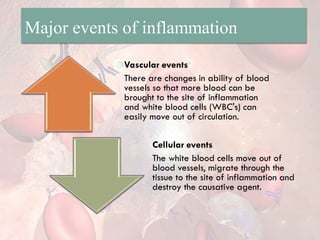
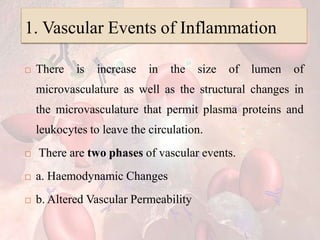
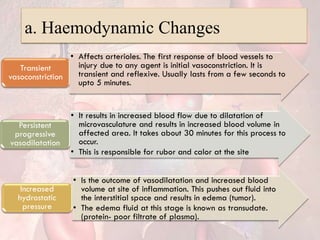
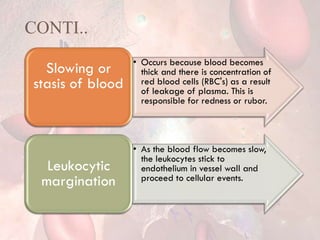
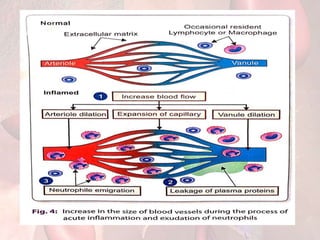
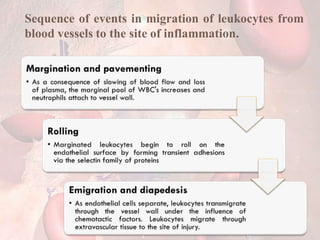
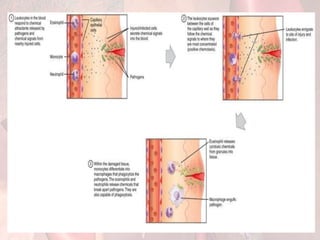
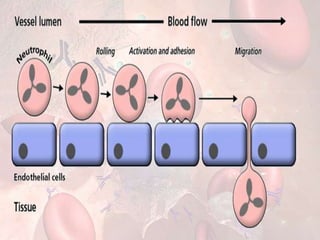
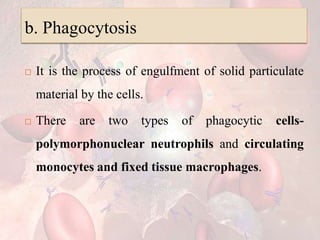
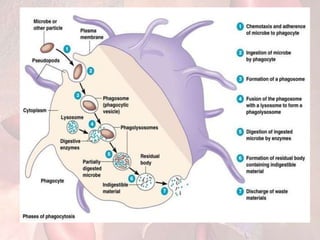
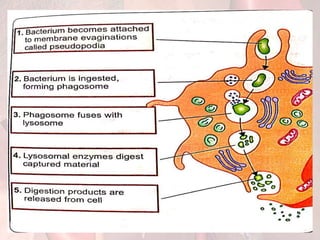
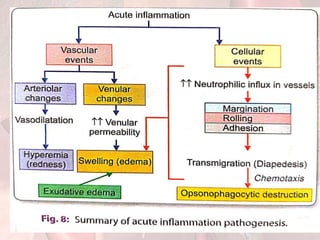
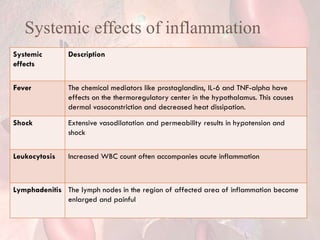
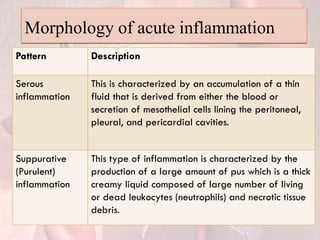
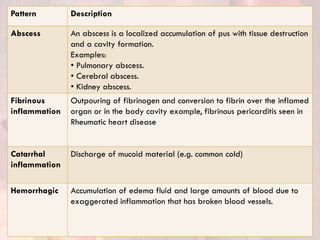
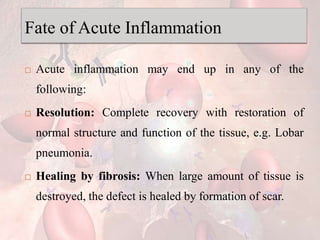
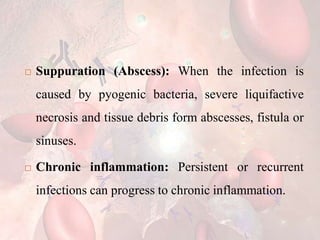
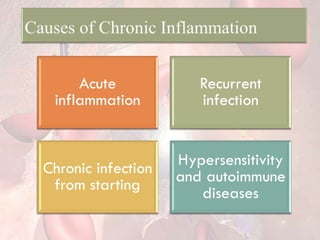
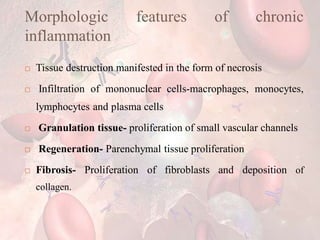
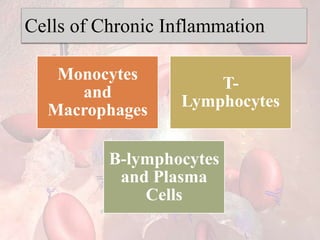
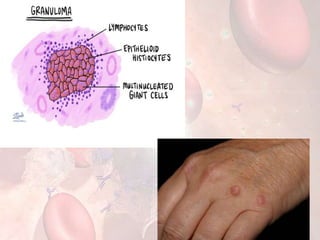
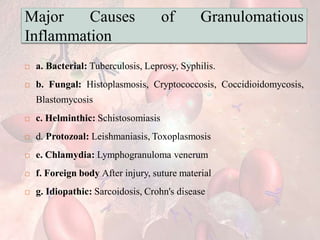
The document provides an extensive overview of inflammation, highlighting its definitions, roles, cardinal signs, and types such as acute and chronic inflammation. It details the pathogenesis, cellular events, chemical mediators, and systemic effects of inflammation, along with the morphologic patterns and fates of acute inflammation. Additionally, it explores granulomatous inflammation, its causes, types, and significant diseases associated with it.