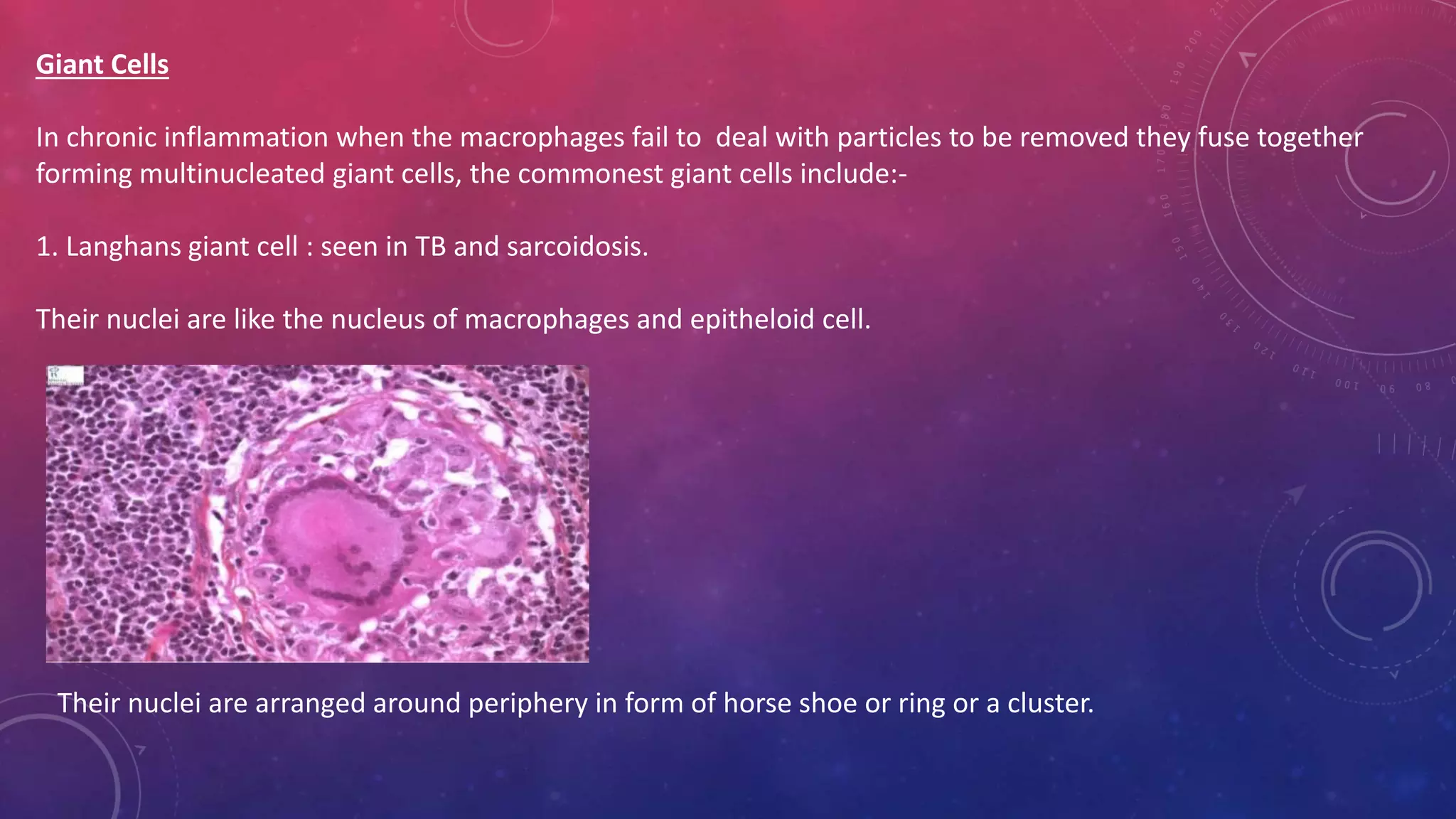
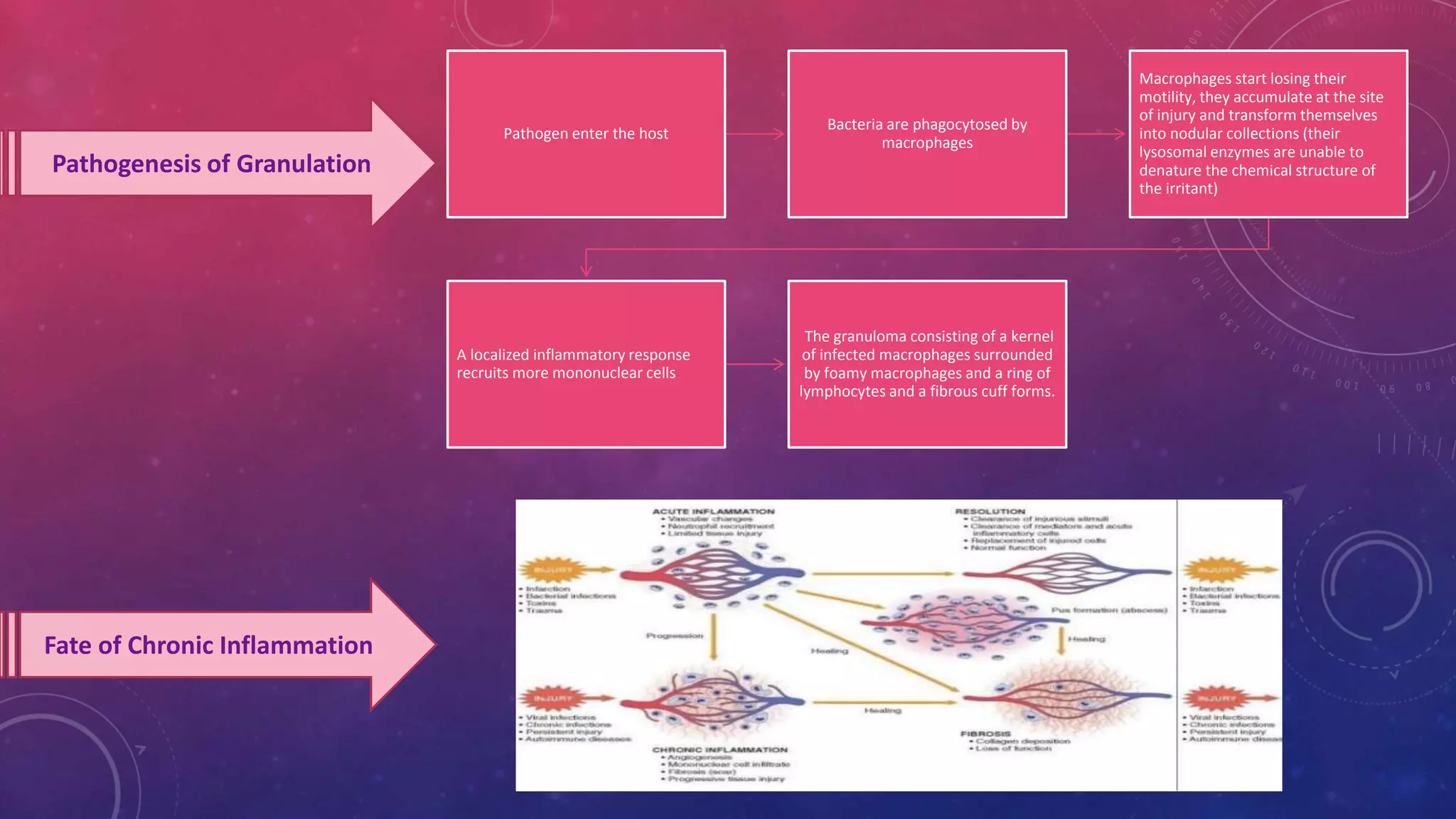
This document discusses chronic inflammation. It defines chronic inflammation as a prolonged process where tissue destruction and inflammation occur simultaneously. Chronic inflammation can result from acute inflammation becoming chronic, recurrent acute inflammation, or starting as a chronic process. It is characterized by mononuclear cell infiltration, tissue destruction, and proliferative changes. The main cell types involved are macrophages, lymphocytes, plasma cells, and sometimes giant cells. Chronic inflammation can lead to risks like cardiovascular disease and cancer if left unchecked.