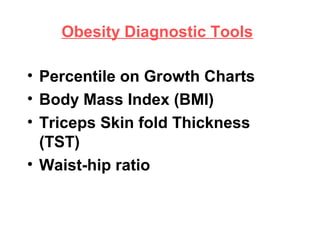
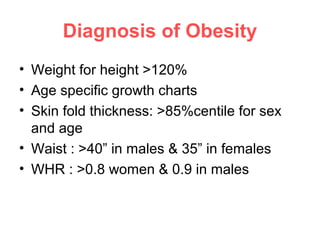
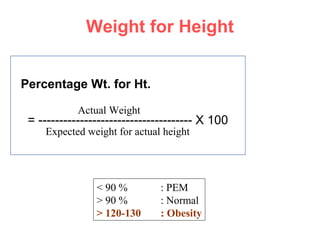
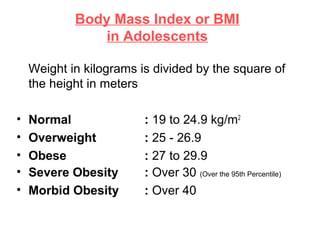
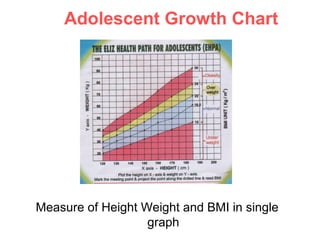
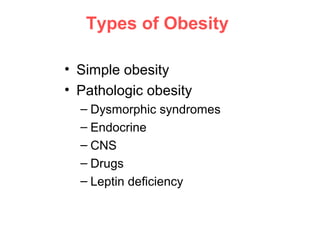
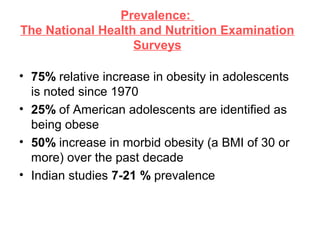
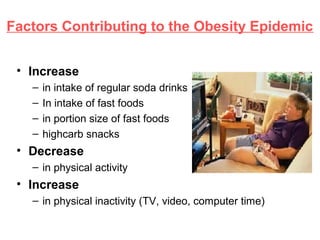
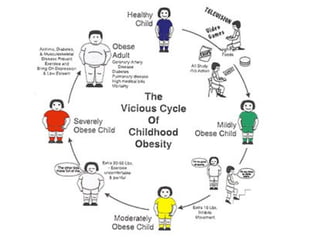
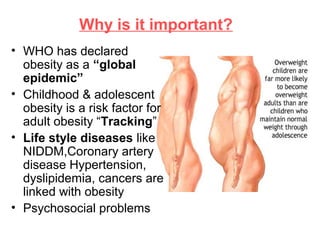
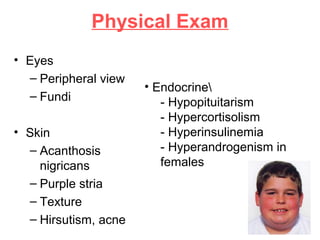
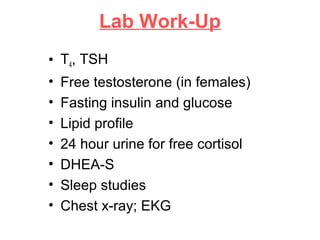
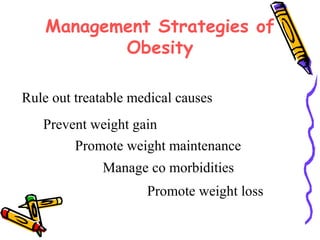
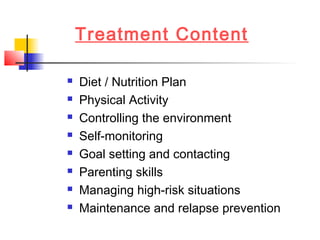
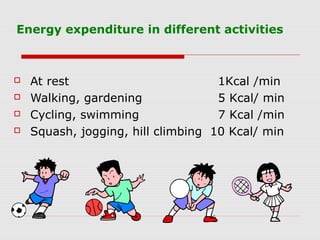
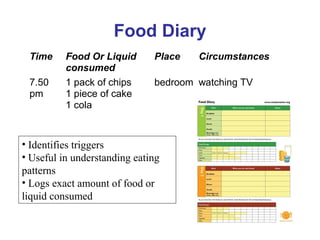
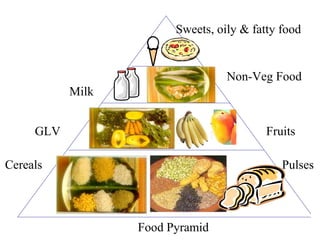
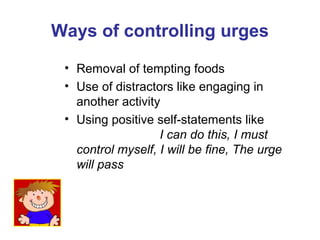
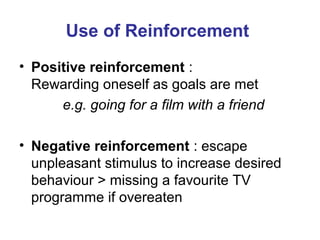
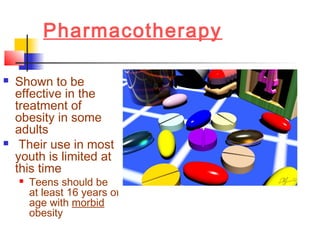
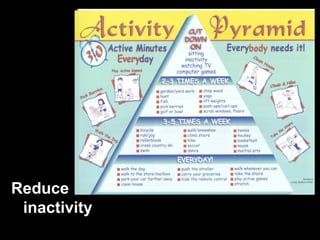
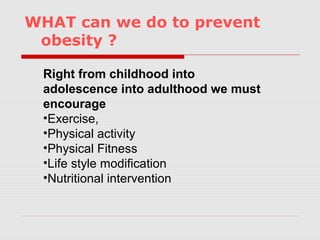
The document discusses diagnostic tools and criteria for diagnosing obesity including body mass index (BMI), skin fold thickness measurements, and waist-hip ratios. It notes the increasing prevalence of obesity among adolescents globally and contributing factors such as increased consumption of sugary drinks and fast food alongside decreased physical activity. Management strategies for obesity include lifestyle modifications like diet, exercise, controlling environmental cues, self-monitoring, and addressing any underlying medical conditions.