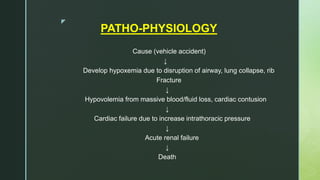
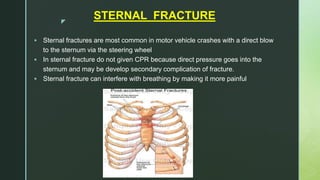
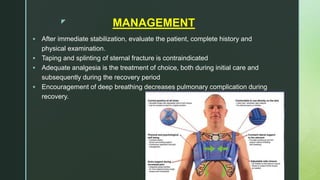
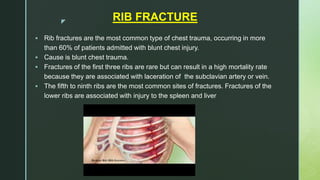
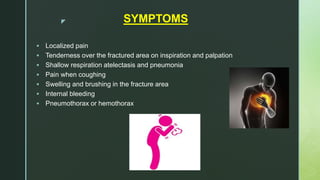
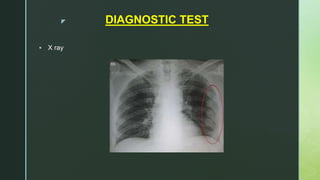
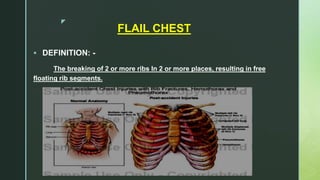
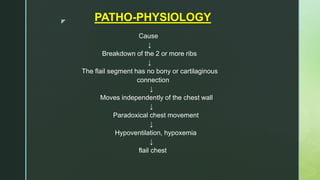
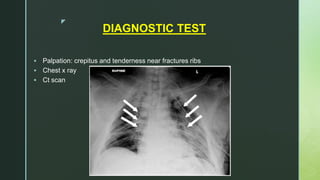
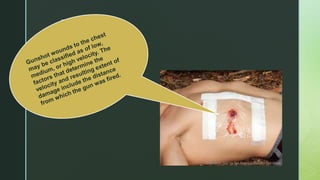
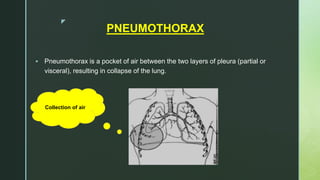
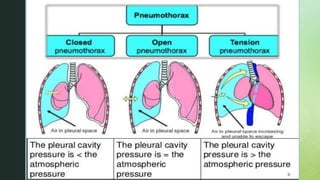
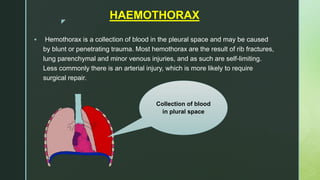
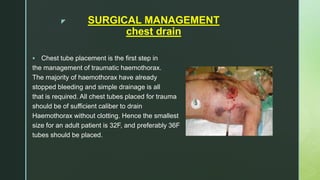
Chest trauma is one of the leading causes of death worldwide. It can be classified as either blunt trauma or penetrating trauma. Blunt chest trauma is more common and results from forces like compression or impacts. Common injuries include rib fractures, sternal fractures, pulmonary contusions, pneumothorax, hemothorax, and flail chest. Diagnostic tests include chest x-rays and CT scans. Treatment depends on the severity and type of injury but generally involves pain management, breathing treatments, and surgery to repair damage and drain fluids if needed.