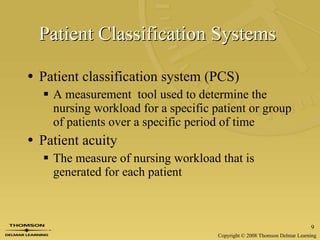
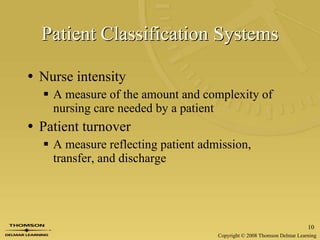
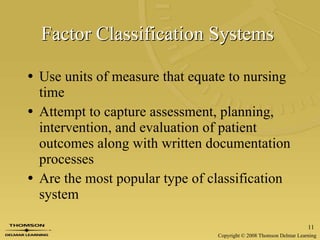
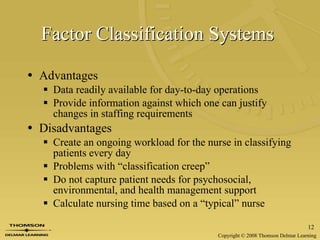
This document discusses effective staffing for nursing units. It covers calculating staffing needs using full-time equivalents, determining needs based on patient volume and acuity, and different units of service to measure nursing workload. Factors to consider in developing a staffing plan include regulatory requirements, skill mix, models of care delivery, and evaluating effectiveness. Different models of care delivery like total patient care, team nursing, and primary nursing are also summarized.