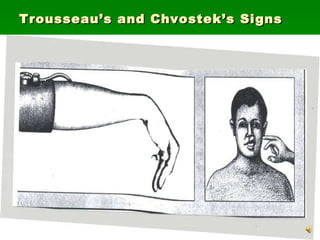
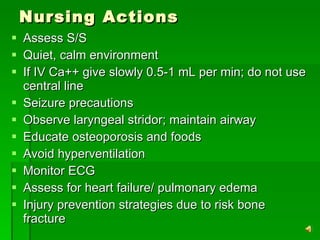
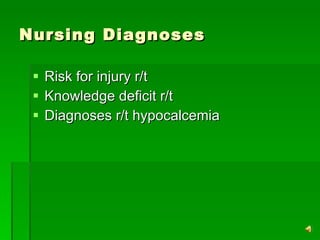
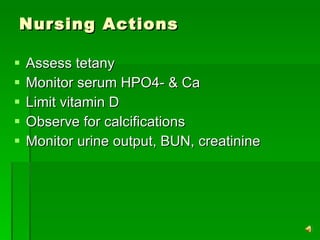
Hypocalcemia can be caused by decreased PTH production, pancreatitis, blood transfusions, or alkalosis. It presents with positive Trousseau's and Chvostek's signs, laryngeal stridor, numbness, and tingling. Treatment includes treating the underlying cause and giving oral or IV calcium supplements while preventing hyperventilation. Nursing focuses on monitoring for symptoms, providing a calm environment, slowly administering IV calcium if needed, educating on prevention, and monitoring for complications like heart failure.