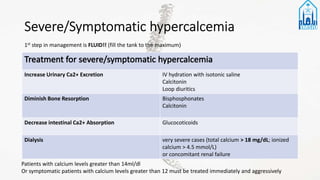
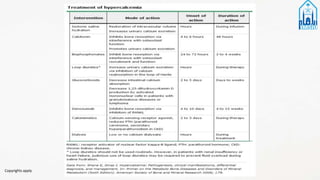
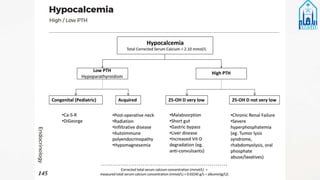
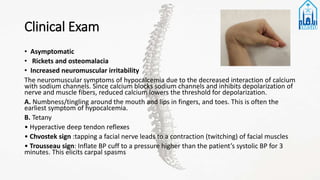
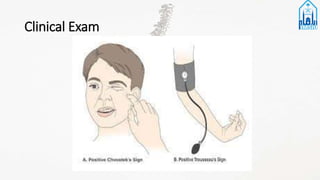
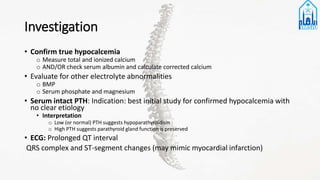
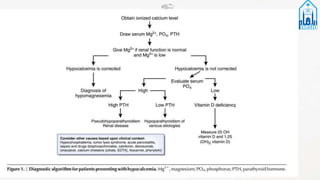
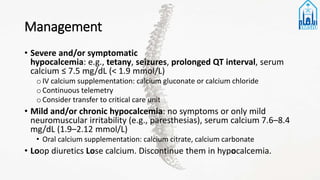
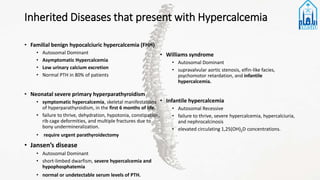
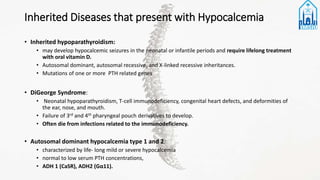
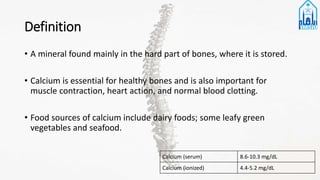
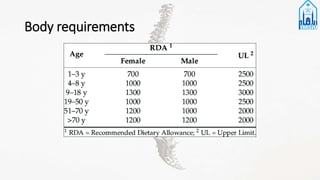
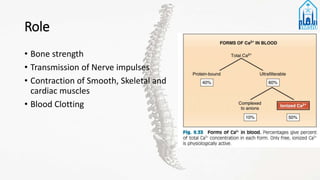
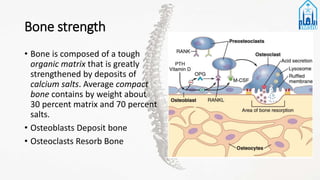
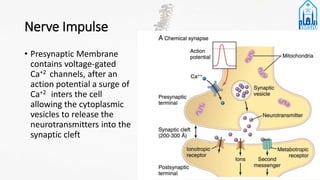
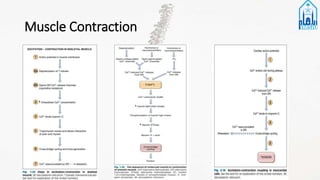
This document discusses calcium disorders including an overview of calcium, hypercalcemia, hypocalcemia, and inherited calcium disorders. It defines calcium and its roles in the body. Hypercalcemia is defined as a serum calcium level >10.5 mg/dL and can be caused by increased bone resorption, gastrointestinal absorption, or decreased renal excretion. It discusses the etiology, clinical exam, differential diagnosis, investigations, management, and complications of hypercalcemia. Hypocalcemia is defined as a total calcium <8.5 mg/dL and discusses its etiology including hypoparathyroidism, renal insufficiency, hypomagnesemia, vitamin D deficiency, and others. It also discusses the






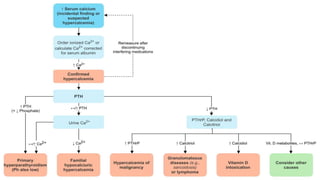
![1. Evaluate calcium imbalance
• Initial test: serum calcium concentration
• Confirm true hypercalcemia:
• measure ionized calcium or calculate corrected calcium.
Corrected calcium (mg/dL) = measured total Ca (mg/dL) + 0.8 (4.0 - serum albumin
[g/dL]). where 4.0 represents the average albumin level.
• Increased ionized calcium, regardless of total calcium levels → true hypercalcemia
(potentially symptomatic)
• Increased total calcium with normal ionized (active) calcium → factitious
hypercalcemia (asymptomatic finding)](https://image.slidesharecdn.com/calciumdisorders-201004093742/85/Calcium-disorders-23-320.jpg)