Hypophosphatemia can be caused by malnourishment, alcohol withdrawal, or use of phosphate-binding antacids. It leads to muscle weakness, pain, confusion, and cardiac issues. Treatment includes oral or IV phosphate supplementation and increasing phosphate-rich foods. Nursing focuses on monitoring vital signs, labs, nutrition, and cardiac and respiratory function.
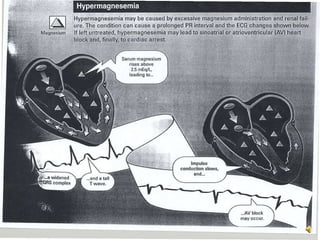
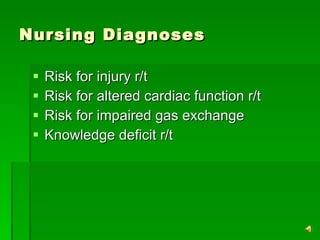
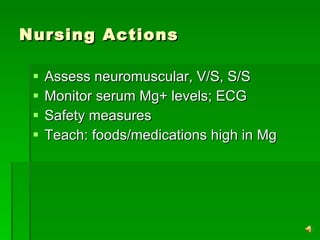
Hypermagnesemia is caused by increased magnesium intake in those with renal issues. It causes lethargy, drowsiness, impaired reflexes, and potentially respiratory and cardiac arrest. Treatment involves IV calcium and fluids. Nursing assesses for neuromuscular and cardiac issues, monitors magnesium levels and ECG, and teaches about magnesium sources.